Bacteria: The good, the bad, and the ugly. SEPA BioScience

Introduction:
Bacteria: The good, the bad, and the ugly.
SEPA BioScience Montana
Module 2
The following reading will give you a basic introduction to bacteria and their role in illness. It will explore some of the details about their structure, the way they reproduce, how they cause infection, and the role of antibiotics in fighting them. This information will help prepare you to maximize your time in BioScience Montana learning module 2, understand the science behind the techniques you are applying in the lab, and concepts you are exploring as part of your time here on campus.
Bacteria: The good
You are probably aware that you are host to a diverse community of microorganisms that are happy to call you home. The vast majority of the “non-you” inhabitants living on and inside your body are bacteria. In fact, there are about ten times as many bacterial cells living inside your body as there are cells that make up your body. For the most part, you are happy to have these tiny helpers on board.
They help fulfill such vital roles as aiding in digestion and nutrient absorption in your digestive tract, maintaining a healthy immune system, reducing inflammatory response, and keeping your skin healthy.
You and your bacteria usually coexist peacefully, largely unaware of one another. So maybe you should know a little more about these microbes that are such an important part of you.
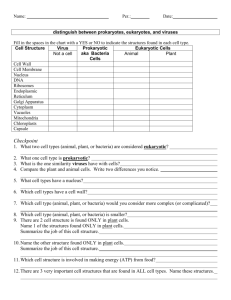
Just what are bacteria? Bacteria are single celled organisms that exist in a wide variety of environments on our planet and on us too. Bacteria are classified as prokarotes, meaning they lack a
“true” nucleus that is enclosed in a membrane. Instead, their genetic material is packed tightly into a
1
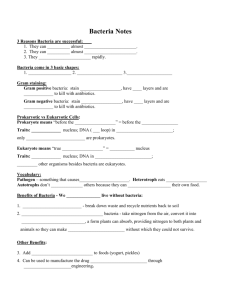
ball-like structure called a nucleoid. They have a single chromosome that contains about 3000 genes, depending on the type of bacteria. Bacteria can be classified in a variety of different ways and are most frequently divided into groups based on their shape. The three main shapes are rod-like (bacillus), spherical (coccus), and spiral (spirillum).
Bacteria reproduce through a form of asexual reproduction called binary fission. Binary fission allows them to clone themselves by replicating their DNA and then dividing. Bacteria are very good at replicating this way and in proper conditions can do so rapidly; it's one of the reasons why they are so successful on our planet and in our bodies. Take for example Escherichia coli ( E. coli), a bacteria common in your intestinal tract. E. coli can reproduce extremely rapidly, dividing every twenty minutes under optimal growth conditions. That means one E. coli in a petri dish can become two in twenty minutes, those two become four in another twenty, those four become eight in another twenty minutes, and so on and so on. Perhaps not so impressive while talking about numbers in the single digits but if you keep the clock running, the numbers get a lot more interesting. After two hours the same petri dish will contain 64 bacteria. After three that number will be 512 and hour four it will be
4096 bacteria. (How many of you could you clone in four hours?) Now, keep in mind that there are millions of bacteria throughout your digestive tract and the following won't surprise you. In an average human being 20 billion E. coli are replicated each day. This is a staggering number but it also happens to be pretty close to the amount lost every day. So on average your natural digestive flora (the microbes that live in your digestive tract) should stay pretty constant. Which is good because they do a lot of good things to help you digest food and regulate your digestive tract.
2
Figure 1: A diagram showing the structural differences between a Gram positive and Gram negative bacterium.
Another interesting characteristic about bacteria is that they have a cell wall made out of a material called peptidoglycan. Although not structurally the same as a plant cell wall (because plant cells make their cell walls out something totally different, cellulose) it serves a similar function, helping to provide structure for the cell and resist osmotic pressure. There is another important way that bacterial cell walls are different from plant cell walls and that is in their location. You may recall
3
that plant cells have their cell wall located on the outside of the cell membrane. Some bacteria are like that but not all. As it turns out, there are two different structural layouts for the cell wall the bacteria and this difference actually leads to another type of bacteria classification. Early on in bacteriological research, scientists noticed that the two different groups of bacteria responded differently to the stains they used in microscope work. One group of bacteria absorbed the stain and were thus called Gram positive. The other type of bacteria didn't and were called Gram negative. Structurally, it is the Gram positive bacteria that construct a thick cell wall as the outside of their cell and it was this peptidoglycan layer that absorbed the stain. Gram negative bacteria are different, they use the peptidoglycan as a cell wall layer between an inner and outer membrane. Because it is sandwiched between two membranes, it doesn't interact with the stain and, therefore, the stain is not absorbed. In figure 1 you can see the basic structural differences between Gram positive and Gram negative bacterial cell walls.
The structural differences between these Gram positive and Gram negative bacteria have important implications in that way that they make us sick and also how they respond to antibiotics.
Unfortunately, it is the harmful aspects of bacteria's interactions with us that we most often associate with them. Bacteria can and do harm the human body. Sometimes we get sick from outside invaders that are new to our system but even our own helpful bacteria can grow out of control and harm us under the right circumstances and that's when things get bad.
Bacteria: The bad
Scientists have a specific word for the things that make us sick, pathogens. A pathogen is defined as a disease causing particle or microorganism. Our bodies are constantly exposed foreign particles and microbes and we usually we don't get sick. That's because we have an immune system and other defenses that do a fantastic job of defending us the majority of the time. Therefore, in order for us
4
to get sick, a pathogen must invade us and resist our defenses well enough that the we become ill.
There are four major classes of pathogens: viruses, bacteria, protists, and fungi. Each of them has their own unique way to attack the body and cause disease. By far, viruses and bacteria are the most common types of pathogens in humans. Viruses and bacteria are very different in many ways; particularly in what they are, but also in how they replicate and what that means for how modern science fights them when they get out of control in the body and become pathogens.
Viruses are actually not classified as organisms. Viruses are not considered living things because they are not made of cells and can't reproduce on their own without a host. They also don't need to eat and don't grow or develop. Structurally viruses are simple and surprisingly yet elegant.
They have an outer coat, called a capsid, that is made of proteins. Their capsids are constructed of geometric patterns, often in elaborate arrangements. Inside the capsid lies the heart of the virus, its
DNA or RNA. This is what holds the genetic code for the virus and, more importantly, the directions for how to make more of the virus. Viruses can't replicate on their own so they must find a suitable host cell. They do this entirely by chance as they float through the environment. If they happen to encounter a cell that is a good host, the virus particle attaches to the outside of the cell and injects its
DNA or RNA into the cell through the cell membrane. The virus DNA or RNA then takes over the cell and forces it to make copies of the virus. The cell fills with new virus particles until it bursts, releasing more viruses to infect more cells in the host organism. A virus infects your cells and attacks them causing them burst, this makes you feel icky. Also, your body reacts to this attack in a variety of ways, depending on the type of virus, and the result is you feel sick.
Bacteria make you feel sick too, but mostly for a different reason. There are two main ways bacteria cause illness, by destroying tissue in the host organism and by making toxins. Bacteria that cause the diseases of tuberculosis, gonorrhea, and leprosy actually invade the tissues they infect and destroy them. Obviously this causes damage to the individual and the living tissues the bacteria have
5
invaded. These are not the most common form of pathogenic bacteria, however. More common are the toxin producing varieties. There are two types of toxins made by bacteria, exotoxins and endotoxins.
Exotoxins are types of toxins released by bacteria; they are extremely potent and even small amounts can kill. Botulinum toxin a neurotoxin produced by the bacterium Clostridium botulinum is one of the world's most potent toxins. One gram of the toxin is potent enough to a million people.
Endotoxins are toxins that are actually present on the bacteria themselves, they are the lipopolysaccharides on the outside of their outer membrane (illustration b on figure 1). Because the endotoxin is the lipopolysaccharide chain found on the outer membrane, endotoxins are found only in
Gram negative bacteria. Salmonella and Escherichia coli are both examples of Gram negative bacteria that have endotoxins. When they grow unchecked in your digestive system you feel sick largely because of endotoxins present in your intestinal tract. The net result of the toxins, whether they are an endotoxin or an exotoxin, is that they make you sick and produce the symptoms of illness.
When a virus infects a host's cells it is actually hiding inside the host's cells, therefore it's hard to find ways to fight a virus without damaging the host cell. That's why your doctor will tell you that you have to let a virus run it's course, generally there's not a drug you can take to help your body fight the infection. This is not the case for bacterial infections. For bacterial pathogens we can take an antibiotic. Antibiotic comes from greek terms that literally mean “against life.” There are different types of antibiotics that attack bacteria in different ways but all basically either attack the bacteria or disrupt the way it functions. To fight bacteria we need a selective poison, one that works against bacterial cells but does no harm to your cells. Luckily bacteria have a very distinct structural difference from your cells, can you recall what it is? If you are thinking about a cell wall, you're right! Many antibiotics work by keeping the bacteria from properly assembling a truly functional cell wall, or by causing the peptidoglycan making up the cell wall to disintegrate. The bacterium then succumbs to osmotic pressure, bursts, and is destroyed. Antibiotics that work this way are extremely effective
6
against Gram positive bacteria but tend to be less effective against Gram negative bacteria because
Gram negative bacteria have their peptidoglycan layer sandwiched between two membranes. For Gram negative bacteria other classes of antibiotics are more effective. The other classes of antibiotics work against bacteria in a variety of ways. Some reduce the bacteria's ability to properly make proteins so the structure of their cell suffers. Others interfere with their ability to copy their DNA so they can't reproduce. Still others make it difficult for them to manufacture energy from glucose. The end result is that the reproductive rate of the bacteria slows down so your immune system can catch up and defeat the bacteria. In the end your immune system wins and you feel better. The unfortunate side effect is that antibiotics target all the bacteria in your body, both the good and the bad, but it is a small price to pay when you are really overrun and ill from a bacterial infection. In a perfect world you get sick, you take a pill, and you get better. But bacteria are tenacious and they have some distinct advantages when it comes to adapting to the drugs we throw at them. Without really trying they sometimes find a way to get by when we try to wipe them out, that's when things get ugly.
Bacteria: The ugly
Have you ever heard the term antibiotic or drug resistant bacteria? This is a term used to describe bacteria that has developed a way to cope with antibiotics. Antibiotic resistance can have some disastrous implications for those who have to deal with one of these so called “Superbugs.” The whole idea of antibiotic resistance actually stems from a pretty cool aspect of bacteria, their ability to rapidly evolve to adapt to their environment. It happens to be one of the characteristics that has helped them to be so successful on our planet and it would be really impressive if we weren’t talking about them infecting us.
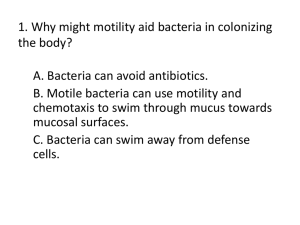
Bacteria are extremely adaptable through natural selection because of their very rapid rates of
7
reproduction but also because they mutate. You may recall that bacteria don't reproduce sexually, they clone themselves, so their genetic variation comes from random mutations that occur when the DNA is copied in preparation for cell division. If one of those random mutations happens to help a bacterium to be resistant to effects of an antibiotic, it will have an rapid impact on the genetics of the bacterial population. For example, let's say we had a group of bacteria living and replicating in a petri dish.
Now say we introduced an antibiotic to that petri dish. Ideally, the antibiotic would kill all the bacteria in the dish but what if it didn't? What if just one bacterium living in the petri dish had some mutation that made it slightly resistant to the antibiotic? That single survivor would go on to replicate and after four hours it would have more than four thousand antibiotic resistant buddies to keep it company. In fact the entire new population of bacteria in the petri dish would all have this antibiotic resistant genetic mutation. This petri dish scenario is similar to what happens in your body except you are talking about much larger populations of bacteria with much more broad range of mutations and a lot more genetic diversity to start with.
MRSA is a superbug that has gotten quite a bit a press lately. MRSA stands for Methicillinresistant Staphylococcus aureus ; Methicillin is a class of antibiotics related to Penicillin.
Staphylococcus aureus is a type of bacterium that is very common on your skin and normally lives there without bothering you. Sometimes the bug overwhelms your immune system and you get a
“Staph” infection but these are commonly treated with antibiotics and rarely cause for concern. MRSA is different, this type of bacteria has become resistant to several classes of antibiotics. This has researchers working hard to develop new lines of antibiotics and doctors mindful to be conservative and appropriate in their use of antibiotics.
As you delve more deeply into concepts of microbiology and apply the techniques used in the research lab during this BioScience Montana learning module, think about how your newly acquired knowledge can impact your life. How will you use this knowledge and experience to build a better
8
community, build leadership, and develop life skills? Enjoy, explore, learn, and discover!
9