Final Report
advertisement

The South Carolina Epidemiological Studies of Epilepsy
& Seizure Disorders
(SCESESD)
Final Report
THE MEDICAL UNIVERSITY OF SOUTH CAROLINA
In Partnership with
The SC Budget and Control Board
The Office of Research & Statistics
PRINCIPAL INVESTIGATOR
Anbesaw Selassie, DrPH
Co-Principal Investigator
Braxton Wannamaker, MD
Investigators
Elisabeth Pickelsimer, DA
Robert Turner, MD, MSCR
Gigi Smith, RN, MSN, CPNP
Walter “Pete” Bailey, MPH
Mary Tyrell, PhD
Epidemiologist & Research Manager
Pamela Ferguson, PhD
Research Associate
Lee Lineberry, BS, (PhD Student)
Statistician & Programmer
Ja Kook Gu, MSPH
CDC Technical Advisor
David Thurman, MD, MPH
Project Office: (843) 876-1100
Executive Summary
The South Carolina Epidemiological Studies of Epilepsy and Seizure Disorders
(SCESESD) in the Department of Biostatistics, Bioinformatics, and Epidemiology at the
Medical University of South Carolina (MUSC) proposed to conduct a population-based
study to determine the prevalence and incidence of epilepsy in South Carolina. The study
targeted the general population of South Carolina. According to the 2002 census data, the
total population of the state is 4,100,000 and it is the 26th most populated state in the union.
The population is 30% black, 67% white, and 3% other races. The lifetime prevalence of
epilepsy has been determined to be 2%.
Persons with epilepsy and seizure disorders were identified from four major data
sources: Statewide Hospital Discharge (HD), Emergency Department (ED) Visits, Physician
Outpatient Visits (POV), and the epilepsy module of the SC Behavioral Risk Factor
Surveillance System (BRFSS). The first three data sources supplied information on persons
with epilepsy and seizure disorders that have been clinically evaluated. Persons were
identified with the diagnosis codes (International Classification of Disease 9th Revision
Clinical Modification, ICD-9-CM) of 345.x (epilepsy and status epilepticus), 780.31 (febrile
seizures), 780.39 (seizure unspecified), 780.2 (syncope), and 293.0 (delirium). Case
identification through BRFSS relied on self-report using random-digit dialing telephone
survey of the adult population of the state. Broader case ascertainment codes were used to
identify individuals that could be misclassified. Detailed clinical information was abstracted
from medical charts of representative sample of 3,983 persons (5.4%) with these conditions
clinically evaluated in 2001 and 2002. By the end of the third year, a total of 21,480
individuals had completed the BRFSS telephone survey making SCESESD among the
largest population-based epidemiological study of epilepsy in the United States.
SCESESD personnel abstracted medical record information on 3,881 randomly
selected persons with epilepsy and seizure disorder. Case-level uniform billing
abstracted data were acquired on 73,955 individuals using the expanded case
ascertainment codes and a database has been developed. The database includes one
primary and up to 9 secondary diagnoses, demographics, number of visits made during
the year, payer information, CPT codes, and unique identifiers tied to SSN. The
database also includes extensive and detailed information from chart abstraction on
ii
3,881 individuals. Case-level data with the appropriate weights on 21,480 respondents
has been generated. SCESESD will make these data public domain after major findings
have been published. This is expected to be no later than October 31, 2008.
Among the major activities completed by the project, determination of prevalence,
incidence, venues of epilepsy care, and measures of data validity are proud
accomplishments. Within such a short time, SCESESD impacted public policy debate,
and enhanced social activism and awareness about epilepsy and seizure disorders. A
steering committee comprised of persons and families with epilepsy, key stakeholders,
and community leaders has been formed to promote further research on epilepsy. Data
generated by the SCESESD has been used to formulate legislative initiative for social
support and waiver programs for persons with epilepsy. Governor Mark Sanford declared
November as epilepsy awareness month and more than three major public campaigns
have been initiated to promote support groups and raise funds.
BRFSS-based prevalence estimate in SC indicate a rate of 2.0% (95% CI: 1.8-2.3)
for ever having epilepsy and 1.1% (95% CI: 0.9-1.2) for active epilepsy among
individuals age 18 and older. For the two year period, the annualized estimate of
prevalence derived from healthcare encounters for 2001 and 2002 ranges from 0.8% to
0.9% and appears to be in total agreement with the lower range estimate of active
epilepsy derived from BRFSS. We further generated a model-based prevalence rate that
provided a conservative estimate of 0.8% using information from the case-level data on
70,000 individuals in a loglinear model. The model shows potential to be tested
elsewhere and uses uniformly available variables from administrative data systems.
The estimated annual incidence rate of epilepsy for the general population of the
state solely based on HD and ED data is 3 per 10,000 (0.03%) based on a follow-up
period of 3 years. This suggests that there are at least 1,200 individuals who develop
epilepsy every year. Assuming a reduction due to the force mortality at 1.68%, a rate 2.5
times higher than the mortality rate in the general population of the state, SC could have
about 120,000 persons living with epilepsy by 2011 if all other contributing causes of
seizure are held constant. Our incidence estimate also shows that the incidence rate of
epilepsy is at least 30 times higher among persons with TBI. Our TBI Registry data
indicate that the incidence of epilepsy after TBI is 2.6/100 person-year within the first
iii
three years of follow-up. With increased incidence of TBI due to various causes, the
influx of persons who develop epilepsy may be higher than the current estimate our
analysis provides.
Our study showed that the healthcare data sources we used can be used to monitor
the prevalence of epilepsy and seizure disorders. The predictive value positive (PVP) of
HD, ED, and POV suggest usefulness of these data sources for surveillance activities.
Our findings indicate that the PVP of 345.x code is remarkably high for all the sources
ranging between 93% and 96%. However, the PVP of 780.3x is very low ranging
between 14% and 20%. It can be assumed that about 80% of those coded with seizure
unspecified code of 780.3x are epilepsy cases based on 3,983 records we reviewed.
Given that 70-80% of the persons coded with780.3x are misclassified as seizure and the
probability of a case of epilepsy being coded as 780.39 is 11 times higher than being
coded as 345.x, it is imperative to develop a surveillance guideline that takes into
account this prolific use to generate a reliable estimate. Our experienced team is more
than willing to work with the CDC in assisting the development of such a guideline.
Finally, we are proud to declare that SCESESD met all of its objectives according
to the stipulation of the award. We have developed a strong, multifaceted surveillance
system with diversified data sources that are complementary to each other. A decision
analysis tool with an exquisite algorithm addressing each set of diagnosis codes has been
developed and validated. Our team and partners are well prepared and ready for more
productive research to better the lives of persons with epilepsy.
iv
Table of Contents
Page
Executive Summary…………………………………………………………………. i
Prevalence rates……………………………………………………………………... 1
Behavioral Risk Factor Surveillance System data……………………………… 1
Chart abstraction data…………………………………………………………...
3
Inpatient and emergency department (HD/ED)……………………….
3
Physician office visits (POV)…………………………………………
5
Prevalence combining HD/ED/POV data……….........................……
7
Model-based approach to estimate prevalence……………………….
7
Incidence rates……………………………………………………………………… 12
Posttraumatic epilepsy……………………………………………………….
12
Incidence of epilepsy utilizing HD/ ED data………..............……………….
22
Causes (triggers) of seizures and etiologies of epilepsy………………………….
28
Target populations for intervention………………………………………………
35
Medication use - HD/ED data…………............……………………………
35
Medication use - POV data……………….........................………………..
38
Posttraumatic epilepsy………………………………………………………
40
Behavioral Risk Factor Surveillance System data…………………………..
40
Focus groups data…………………………………………………………… 41
Severity and subtypes of epilepsy…………………………………………………. 42
HD/ED data…………........…………………………………………………. 42
POV data…………………………..........................………………………… 45
Behavioral Risk Factor Surveillance System data…………………………… 48
v
Venues and levels of care………………………………………………………….. 48
Behavioral Risk Factor Surveillance System data………………………….. 48
POV data…………………….........................…………………………….. . 49
Focus groups data……………………………………………………..…….. 50
Traumatic Brain Injury among persons with seizure disorder………....…..…... 50
Data quality………………………………………………………………..…….….. 56
Population and sample information………………………………..………... 56
HD/ED data…………...............................................……....…….….. 56
POV data……….........................…………………………..………... 58
Predictive Value Positive and Sensitivity of seizure and epilepsy codes…..... 60
HD and ED Data.........................................……………………….….60
POV Data...........................…………………………………………. 61
Estimates of PVP and Sensitivity for HD/ED.data………….……… 62
Estimates of PVP and Sensitivity for POV data....…………….…… 63
Algorithm to identify epilepsy patients from administrative datasets….…… 63
Data quality measures……………………………………………………….. 68
Dissemination of results…………………………………………….……………… 72
Purpose and Plan……………………………………………………….……. 73
Reports, Websites, Presentations, and Publications…………………….…… 73
Appendices……………………………………………..…………………………… 76
A. Abstraction manual for HD/ED charts….............................................….. 77
B. Abstraction manual for POV charts……….........................………….… 108
vi
C. Comparison of HD/ED sample to population........……………………… 122
D. Comparison of POV sample to population….........................………….
125
E. Model-based case-level likelihood of an epilepsy diagnosis…………… 127
F. Posttraumatic epilepsy incidence analysis………………………………
133
G. Sampling plan for HD/ED charts……..............................................……. 136
H. Sampling plan for POV charts………..........................…………………… 138
Acknowledgement..……………………………………..…………………………… 139
vii
I. Prevalence Rates
Aim—Provide reliable and stable population-based estimates on the incidence and prevalence
rates of epilepsy and other seizure disorders.
Prevalence rates were generated using a multifaceted approach. The state-based Behavioral
Risk Factor Surveillance System (BRFSS) was used to generate self-reported epilepsy
covering three years (2003-2005) of surveillance. A total of 21,480 individuals age 18 and
older responded to the survey questions. Existing data sources pertaining to 2001 and 2002
Hospital Discharges (HD), Emergency Department (ED) and Physician Office Visits (POV)
provided statewide information on persons with seizure disorders. Each of these is described
below. Prevalence rates were generated from both state-based BRFSS and data collected
from the clinical encounters
A. BRFSS is a state-based, random-digit–dialed telephone survey of the noninstitutionalized, U.S. civilian population aged >18 years. The South Carolina Behavioral
Risk Factor Surveillance System surveys for 2003 through 2005 included questions on
epilepsy listed in Table 1. The survey included questions regarding history of epilepsy
and number of seizures experienced during the past three months. Respondents were
considered to have active epilepsy if they 1) reported ever having been told by a doctor
that they had a seizure disorder or epilepsy and 2) either were currently taking medicine
to control epilepsy or had had one or more episodes of seizure during the preceding 3
months. Active epilepsy was categorized further by whether the respondent had had one
or more seizures during the preceding 3 months. Data was weighted by sex, race and age
to adjust for differences between the survey population and the South Carolina
population. 2003 and 2004 survey results were reported earlier (MMWR, October 28,
2005 / 54(42);1080-1082). By the end of the third year, a total of 21,480 individuals had
completed the survey—5,926 in 2003, 7,114 in 2004 and 8,440 in 2005—for response
rates of 41.6%, 43.8% and 59.1% respectively. The first question was considered as
measuring the lifetime prevalence of epilepsy, and had a response rate of 92.0%.
Respondents were considered to have active epilepsy if they 1) reported ever having been
told by a doctor that they had a seizure disorder or epilepsy and 2) either were currently
taking medicine to control it or had had one or more episodes of seizure in the preceding
1
3 months. Active epilepsy was further categorized as controlled or uncontrolled based on
whether the respondent had had a seizure in the preceding 3 months. Condensed results
for the five questions, with active, non-active, controlled, and non-controlled are shown in
Table 2, with 95% confidence intervals (CI).
Table 1. Survey questions included in the SC BRFSS epilepsy module
1. Have you ever been told by a doctor that you have a seizure disorder or epilepsy?
1. Yes
2. No†
7. Don’t know/Not sure†
9. Refused†
2. Are you currently taking any medicine to control your seizure disorder or epilepsy?
1. Yes
2. No
7. Don’t know/Not sure
9. Refused
3. How many seizures have you had in the last three months?
1. None
2. One
3. More than one
4. No longer have epilepsy or seizure disorder†
7. Don’t know/not sure
9. Refused
4. During the past 30 days, to what extent has epilepsy or its treatment interfered with
your normal activities like working, school, or socializing with family or friends?
Would you say...
1. Not at all
2. Slightly
3. Moderately
4. Quite a bit
5. Extremely
7. Don’t know/Not sure
9. Refused
5. In the past year have you seen a neurologist or epilepsy specialist for you epilepsy or
seizure disorder?*
1. Yes
2. No
7. Don’t know/Not sure
9. Refused
†
If these responses were given, interviewer skipped the rest of the epilepsy questions.
*Included years 2004-2005 only.
2
Table 2. Weighted summary of the SC BRFSS survey, 2003-2005
Total
Epilepsy Status
Do not have epilepsy
Have epilepsy
N
% (95% CI)
19,390
379
98.0 (97.7-98.2)
2.0 (1.8-2.3)
Taking medicine
190
46.1 (39.6-52.5)
Not taking medicine
189
53.9 (47.5-60.4)
24.5 (18.4-30.6)
84
Had seizure in prev. 3 mos.
72.9 (66.7-79.1)
277
No seizures in prev. 3 mos.
2.6 (1.0-4.2)
11
No longer have epilepsy
Epilepsy interfered
92
28.2 (21.7-34.7)
Epilepsy did not interfere
272
71.8 (65.3-78.3)
Epilepsy, nonactivea
172
1.0 (0.8-1.1)
207
1.1 (0.9-1.2)
Epilepsy, activeb
c
Active, controlled
117
52.8(43.7-62.0)
84
47.2(38.0-56.3)
Active, uncontrolledd
Seen neurologist in past year
Yes
88
37.8(29.4-46.3)
No
160
62.2(53.7-70.6)
a
nonactive=’yes’ to question 1, but not taking medication and no seizure in
previous 3 months
b
active=taking medication or seizure in previous 3 months
c
active, controlled=taking medication and no seizure in previous 3 months
d
active, uncontrolled=seizure in previous 3 months
The results show prevalence rate of 2.0% (95% CI: 1.8-2.3) for ever having epilepsy
and 1.1% (95% CI: 0.9-1.2) for active epilepsy among individuals age 18 and older.
Chart Abstraction Data—following are data sources with abstracted information:
B. Inpatient and Emergency Department— The SC Budget and Control Board, Office of
Research and Statistics (ORS), is the entitled by state law to serve as the repository of
data from all nonfederal hospitals and EDs. Data are dumped 90 days after the end of the
calendar quarter and the format of data submission is based on the Uniform Billing, 1992
layout, often referred to as UB-92. We obtained data on 70,955 unduplicated individuals
from all 62 nonfederal hospitals and 64 emergency departments (EDs) across the state for
the calendar year 2001 and 2002 to capture persons with a diagnosis of epilepsy, seizure
disorders, syncope, and delirium. Data were unduplicated using the patients’ unique
identifiers. A representative sample of 3,881 unduplicated records (5.5%) were
abstracted to collect additional data (please see Appendix A–Abstraction manual for
3
inpatient/ED charts for information collected). Table 3 compares patient characteristics
by abstraction status.
Table 3. Characteristics of Patients by Abstraction Status
Total
Abstracted
Characteristics
N=70,955 (%)†
n1=3,881 (%)‡
Year:
2001
30,948 (43.6)
2,428 (7.9)
2002
40,007 (56.4)
1,453 (3.6)
Age group:
0-9
5,233 ( 7.4)
439 (8.4)
10-19
5,715 ( 8.1)
256 (4.5)
20-39
14,944 (21.1)
925 (6.2)
40-59
19,210 (27.1)
1,207 (6.3)
60-79
17,425 (24.6)
789 (4.5)
80-89
6,980 ( 9.8)
226 (3.2)
90+
1,448 ( 2.0)
39 (2.7)
Primary Payer: Private
20,528 (28.9)
892 (4.4)
Medicaid
11,865 (16.7)
963 (8.1)
Medicare
28,429 (40.1)
1,458 (5.1)
Uninsured
10,133 (14.3)
568 (5.6)
UB-92 diagnosis: 345.x
2,954 ( 4.2)
1,186 (40.2)
7803
32,892 (46.4)
2,566 ( 7.8)
7802
33,094 (46.6)
112 ( 0.3)
2930
2,015 ( 2.8)
17 (0.8)
†
Column percent ‡ Row percent
Not abstracted
n2=67,074 (%)‡
28,520 (92.1)
38,554 (96.4)
4,794 (91.6)
5,459 (95.5)
14,019 (93.8)
18,003 (93.7)
16,636 (95.5)
6,754 (96.8)
1,409 (97.3)
19,636 (95.7)
10,902 (91.9)
26,971 (94.9)
9,565 (94.4)
1,768 (59.9)
30,326 (922)
32,982 (99.7)
1,409 (97.2)
Cases were selected after stratification by diagnosis category using ICD-9-CM codes
of epilepsy (including status epilepticus) (345.x), convulsions (780.3), syncope and
collapse (780.2), and acute delirium (293.0). In our evaluation to determine the
prevalence of epilepsy from these sources, the following general principles were
observed:
1. All characteristics of the sample (sex, race, age, or payer) are comparable with the
referent population from which the sample is per diagnosis strata (345.x or 780.3)
and calendar year (2001 or 2002). (Appendix C for actual comparisons). A total
of 3,983 charts were sampled and reviewed. The accuracy of the charts reviewed
is summarized in Table 4.
2. ICD codes of 780.2 and 293.0 are listed as independent diagnosis when there is
neither a 345.x nor 780.3 diagnoses.
3. If there is more than one seizure-related code, the code utilized is assigned
according to the following hierarchy: 345.x > 780.3.
4. Data were combined for 2001 and 2002 and annualized.
4
5. For duplicate observations in 2001 and 2002, individuals present in both years
were unduplicated. If they had both a 780.3 and a 345.x code, the 345.x visit was
retained.
Abstracted records were reviewed by trained neurology nurse practitioner and nurses.
When information extracted required a second opinion, an adult epileptologist (BW) and
a pediatric epileptologist (RT) provided their opinion. Following is the summary of the
abstracted HD and ED charts comparing diagnosis assigned in UB-92 and clinical
reviewers.
Table 4. Accuracy of abstracted HD and ED charts, SC 2001-02
Diagnosis after clinician review
Diagnosis
UB-92
Epilepsy
Status
Seizure
Syncope
345.x
1016 (85.2%) 61 (5.1%)
41 (3.4%)
0
780.3
2040 (73.1%) 94 (3.4%)
430 (15.4%) 3 (0.1%)
All
3056 (76.7%) 155 (3.9%) 471 (11.8%) 3 (0.0%)
Inadequate
information
74 (6.2%)
224 (8.0%)
298 (7.5%)
Total
1192 (29.9%)
2791 (70.1%)
3983 (100%)
Based on the findings of Table 4, 85.2% of 345.x codes, and 73.1% of 780.3 codes, have
evidence of epilepsy. When the proportion of clinically confirmed epilepsy is applied to
the referent population, the following annualized frequency is obtained:
Diagnosis†
Proportion
Estimated # of
Group
Frequency
after review
epilepsy cases
345.x:
3177
85.2%
3177*.852 = 2,707
780.3:
31,695
73.1%
31,695*.731 = 23,169
Estimated number of HD and ED visits with epilepsy
= 25,876
†
There is 4.8% difference in diagnoses when compared to sample population .
If we make the assumption that the inconclusive cases due to inadequate information
would follow the same distribution as those records that furnished adequate information
and ignore them, the proportion of epilepsy will be 90.9% and 79.5% respectively for
345.x and 780.3 codes. This latter proportion yields 28,086 persons with epilepsy and
could be interpreted as upper range of the estimate.
C. Physician Office Visit—For data obtained from POV, the sample of records reviewed
were 302 records, 9.3% of 3,253 unduplicated encounters. Although the sampled of
proportion is nearly twice that of HD/ED sample, the smaller number of patients in the
POV setting makes it difficult to conduct subset analysis by various attributes due to
5
scanty distribution in some of the cells. Hence, categories were collapsed for payer status
and only epilepsy (345x) and seizure (780.3) were identified. Detailed distribution by
abstraction status with 95% confidence limits is presented in Appendix D. Unlike the
HD/ED data, POV data were not identified by year excepting Medicare data which came
from 2001 visits. The POV patients have had no ED/HD encounters for the years in
mention. The diagnosis codes were hierarchically ranked in the following order: 345.0,
345.1, 345.4, 345.5, 345.6, 345.7, 345.8, 345.9 > 345.2, 345.3 > 780.3. Table 5 shows
the distribution of billing codes after review of the records by the clinical nurse
practitioner and nurses, and input of the two epileptologists.
Table 5. Accuracy of abstracted POV charts, SC 2001-02
Diagnosis after clinician review
Diagnosis
Inadequate
UB-92
Epilepsy
Status
Syncope
information
345.x
202 (91.4%)
1 (0.5%)
10 (4.5%)
8 (3.6%)
780.3
74 (91.4%)
0
4 (4.9%)
3 (3.7%)
All
276 (91.4%)
1 (0.3%)
14 (4.6%)
11 (3.6%)
Total
221 (29.9%)
81 (70.1%)
302 (100%)
For both 345.x and 780.3 codes, the proportion of the records determined to be epilepsy
cases was 91.4%. When these proportions were applied as weighting factor, of the 1,157
patients with 345.x, 1,057 and of the 2,096 patients coded with 780.3, 1,916, total 2,973
were deemed to be epilepsy cases. If the 11 records were ignored, the total number
would be 3,086. More detailed sample information is found on page 57.
The data analyzed from POV is not generalizable to the general population since the
data sources are limited to selected practices and do not include children under the age of
2 years. However, epilepsy in this age group is expected to be small and negligible. To
approximate the POV data to the general population of epilepsy patients from physician
offices through out the state, we assumed that the prevalence of epilepsy among patients
encountered in physician offices elsewhere is approximately comparable to the
distribution noted in the sampled records among Medicare, Medicaid and SHP insured
patients. Based on state demographic data, we assumed that the sample area coverage is
approximately 39% of the state. If these values are extrapolated to the rest of the state,
the sample analyzed represents a low of 8,494 (2,973/0.35) and a high of 8,817
(3086/0.35) patients with epilepsy. These numbers are most likely an underestimate
until we can obtain the number of SC Medicare patients with a 345.x or 780.3 diagnosis
6
code in 2002 who were not seen as an HD/ED patient during 2001 or 2002. Following is
a step-by-step calculation of prevalence based on the three data sources.
Prevalence for Combined HD/ED/POV Data
•
Average population of the state for 2001-2002= 4,081,794 (Source: US Census
Bureau)
•
Individuals with epilepsy in SC:
o Lower range: 25,876 HD/ED + 8,494 POV = 34,370
o Upper range: 28,086 HD/ED + 8,817 POV = 36,903
•
Annualized prevalence estimate of clinically attended (~Active) epilepsy in SC
for 2001 and 2002
o Lower range: 34,370/4,081,794= 0.84%
o Upper range: 36,903/4,081,794= 0.90%
D. Model-based Approach to Estimate Prevalence:—this approach utilized the 2001 and
2002 ED/HD data with 70,955 unduplicated observations shown in Table 3. The main
research effort of this modeling approach is to determine the utility of routinely available
surveillance variables in correctly predicting epilepsy using the case ascertainment
differential diagnosis codes of 345.x, 780.3, 780.2, and 293.0 and covariates. The
covariates selected for this modeling approach were seven variables: Demographics (age,
sex, race, and payer status) and clinical (UB-92 diagnosis, number of visits during the
two years, comorbid conditions frequently associated with seizure disorders). The
response variable was dichotomous level of clinically confirmed epilepsy (epilepsy vs. no
epilepsy) based on the adjudication of the clinical neurology nurse practitioner and nurses
and the two epileptologists on the 3,983 charts reviewed (Table 4). The final analysis
relied on 3,881 records after deleting 102 records that were abstracted and reviewed in
each year.
The covariates selected were first evaluated for their bivariate association with the
response and only those with p<0.10 were included in the multivariable logistic
regression. Only sex was excluded from the multivariable model due to lack of
association. The final model included the variables listed in Table 6 along with the
various levels of effect. The beta-coefficients from the model were applied to the
observations that were not reviewed (n=67,074) to identify the predicated probability of
7
epilepsy for each patient conditional on the covariate values each patient satisfied. We
used the following formulae to calculate the probability of epilepsy and its 99%
confidence interval for each case:
(1) P=exp(α+β*Χ)/(1+exp exp(α+β*Χ))
(2) 95%CI= exp(α+β*Χ)/(1+ exp(α+β*Χ)) +/- 1.96*sd.
where: α – the intercept
β = the vector of mean beta-coefficients from the 100 estimation sets
X = the vector of explanatory variables
sd = the standard deviation of the distribution of mean predicted probabilities
To assess the predictive power of the model, a Receiver Operating Characteristic
(ROC) curve was constructed for the validation data (n=3,881). A ROC curve is a
graphical representation of the trade off between false negative and false positive rates
for every possible probability cut off (for example, the tradeoff if only those with a
probability of 6% or higher are defined as likely to have epilepsy). Equivalently, the
ROC curve is the representation of the tradeoffs between sensitivity and specificity. The
curve shows sensitivity on the Y-axis and one minus specificity on the X-axis. A ROC
curve that climbs rapidly toward the upper left hand corner of the graph indicates that the
true positive rate is high while the false negative rate is low. When the ROC curve
follows a diagonal path from the lower left hand corner to the upper right hand corner, it
means that every improvement in false positive rate is matched by a corresponding
decline in the false negative rate. The Area Under the Curve (AUC) is a representation of
the model’s ability to correctly discriminate a pair of true epilepsy and non-epilepsy
patients—the larger the AUC, the higher the ability of the model to correctly discriminate
those who have epilepsy from those who do not. Generally, AUC 0.90-1.00 is considered
outstanding discriminatory power, 0.80-0.89 as excellent, 0.70-0.79 as very good, 0.600.69 as good, and values less than 0.50 are worse than chance 1. As shown in Figure 1,
the sensitivity analysis of our model shows an AUC of 0.75, suggesting very good
discriminatory power with the covariates identified (Figure 1). The model fit and
predictive power is also strong. Given that the model utilized the most parsimonious set
1
Hosmer DW, Lemeshow S. Assessing the fit of the model. In: Applied Logistic Regression. New York:
John Wiley & Sons; 2000:160-164.
8
of covariates that are routinely available in administrative datasets, the potential
usefulness of the model warrants further consideration in other settings.
Table 5. Logistic Regression Parameter Estimates
Wald Confidence Interval for Parameters
Parameter
Level of effect
Estimate
99% Confidence Limits
Intercept
β0
Baseline
-1.5612
-2.0566
-1.0658
Agegp
β10
0-9
Agegp
β11
10-19
1.4528
0.9692
1.9364
Agegp
β12
20-39
2.0098
1.6200
2.3996
Agegp
β13
40-59
1.8267
1.4561
2.1972
Agegp
β14
60-79
1.3783
0.9287
1.8278
Agegp
β15
80-89
1.3879
0.7920
1.9839
Agegp
Β16
90+
1.0141
-0.00274
2.0309
Racegp
β20
White
Racegp
β21
Black
0.2144
-0.0106
0.4394
Racegp
Β22
Other
-0.4160
-1.1813
0.3493
Comorbgp
β30
Lo/No risk
Reference
Reference
Reference
†
Comorbgp
β31
Hi-risk
0.4744
0.1215
0.8274
Visit
β40
1
Visit
β41
2-5
1.0356
0.7980
1.2732
Visit
β42
>=6
1.7164
1.0489
2.3838
Esdgp (UB-92)
β50
Syncope/Delirium
Esdgp (UB-92)
β51
Epilepsy
1.0584
0.5893
1.5276
Esdgp (UB-92)
β52
SeizureNos
0.2243
-0.1683
0.6168
Payer
β60
Private
Payer
β61
Medicaid
0.5911
0.2679
0.9143
Payer
β62
Medicare
0.5299
0.1769
0.8830
Payer
β63
Uninsured
0.1860
-0.1702
0.5422
Reference
Reference
Reference
†
Hi-risk comorbid conditions include the presence of mental retardation, psychiatric problems, depression,
substance abuse, paralysis, and anemia in the secondary diagnosis field.
We calculated the probability of epilepsy for each case in the 2001-2002 ED/HD
surveillance dataset by applying the parameter estimates. For individual cases, the
probability could be written in the following manner.
P(D) = {1+ exp – ( β0 + β10 + β11 + …….+ β62 + β63 )}-1
9
To illustrate how the model parameters work in assessing the probability of epilepsy based on the
covariates, the following three examples are provided.
Example 1: Patient A is 27 years-old, black, with right hemiplegia, had 6 visits during the
year, UB-92 diagnosis was 345.1, is Medicaid insured. The probability that this would turn out to
be true epilepsy is:
{1+exp-(-1.5612+2.0098+0.2144+0.4744+1.7164+1.0584+0.5911)}-1 = 0.9890 (98.9%)
Example 2: Patient B is 17 years-old, native American, with no comorbid condition, had
no previous visit during the year, UB-92 diagnosis was 780.2, is privately insured.
The
probability that this would turn out to be true epilepsy is:
{1+exp-(-1.5612+1.4528+0.0+0.0+0.0+0.0+0.0)}-1 = 0.1216 (12.2%)
Example 3: Patient C is 74 years-old, Hispanic, with alcoholism and anemia recorded as
comorbidities, had eight visits during the year with seizure episode, UB-92 diagnosis was 780.39,
is Medicare insured. The probability that this would turn out to be true epilepsy is:
{1+exp-(-1. 5612+1.3783+(-0.4160) +0.4744+1.7164+0.3522+0.2166)}-1 = 0.8967 (89.7%)
Based on the estimated probabilities and a cutoff point of 47%, patients A and C are likely to be
epilepsy cases while patient B is less likely to be an epilepsy case.
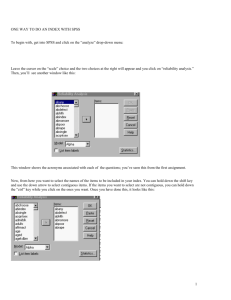
Figure 1. Sensitivity analysis for predicting Epilepsy from Administrative Datasets
Legend:
1. AUC= Area under the curve--ability of the model to correctly discriminate those with epilepsy from
those without. It is the reflection of the C statistics from the logistic output.
2. PoI= Point of intersection (0.695)--the point at which sensitivity and specificity are equal, i.e., a cutoff
point where false positives and false negatives are balanced.
10
To determine the appropriate cutoff point for the predicted epilepsy, we used the 50th
percentile (41.85) of the true positives cases as the cutoff for probable epilepsy and the
40th percentile (33.48) as the cutoff for possible cases. While it is customary to use the
mean and 1 standard deviation below the mean as the upper and lower range of the cutoff
points, the choice of the median is a good substitute when data are not normally
distributed, which is the case in our distribution. Based on these cutoff levels the
proportions of cases that are highly likely and likely to be epilepsy are shown in Table 7.
Table 6. Cutoff points and model-based distribution of epilepsy among HD &ED visits, 2001-2002
Epilepsy
Location
Cutoff Level
Frequency
Percent
Cumulative
Frequency
Cumulative
Percent
1)Probable
≥ 50th% of T.P
0.4185-1.000
21,046
29.66
21,046
29.66
2)Possible
40th % of T.P
0.3348-0.4185
9,875
13.92
30,921
43.58
3)Unlikely
<40th % of T.P
0.0000-0.3347
40,034
56.42
70,955
100.00
Any Epilepsy
≥ 40th % of T.P
03348-1.000
30,921 Rate = (30,921/4,100,000) =0.7500%
For individual prediction of epilepsy, we utilized the model parameters as
described earlier and calculated the probabilities across the variables reflected as risk
characteristics for each person. Appendix E shows a 0.1% randomly selected sample of
records to which such an estimate is demonstrated. Overall, when the UB-92 diagnosis is
345.x, the model’s prediction agrees with the clinically confirmed diagnosis in 8 out of
10 cases. Conversely, when the diagnosis is 780.3, the model’s prediction agrees with
the expert decision in 4 out of 10 cases. This suggests that the prediction has higher
sensitivity with a tradeoff on specificity. However, for the purposes of surveillance the
current cutoff appears to be adequate. Finally, it is important to note that our effort in
developing this model as an alternative to time/labor-intensive and costly review of
records is an important step towards improving epilepsy surveillance in the US. We feel
there is plenty of room to improve the model and test it in various settings. The global
estimate of epilepsy noted from our model is comparable with the approach presented
earlier.
11
II. Incidence rates
Aim—Determine the incidence of epilepsy in SC from existing data sources
A. Posttraumatic epilepsy—we utilized the SC Traumatic Brain Injury Follow-up
Registry (SCTBIFR) data to estimate the incidence of epilepsy after TBI. The cohort is
comprised of persons aged 15 years and older with TBI randomly selected from the SC
statewide non-federal hospital discharge data set over four years (January 1, 1999
through December 31, 2002) and recruited to participate in the follow-up telephone
interviews. TBI was defined as any discharge with a primary or secondary diagnosis of
trauma to the head associated with decreased consciousness, amnesia, other neurological
or neuropsychological abnormalities, skull fracture, or intracranial lesion, in accordance
with the CDC case definition of TBI. During the recruitment period 4,519 persons were
discharged alive. At time of first interview, 3,746 persons (82.9%) were alive and eligible
to participate. 2,118 (56.5%) of these were both able to be located and agreed to
participate for the first interview one year after their discharge.
This cohort was used to examine the relationship between TBI and epilepsy after
injury. During the interviews, individuals were asked about the presence of seizures or
epilepsy, both before and after their TBI. As detailed in Table 8, initially the questions
were less sensitive to the presence of epilepsy after TBI, since an individual with
epilepsy, but no recent seizures, might respond negatively. The questions were later
changed to be more sensitive and a few were added to gain additional information.
Table 8. Epilepsy-related questions used for initial identification of epilepsy cases.
1: Before your injury, did a doctor ever tell you that you had a seizure disorder or
epilepsy?
1=Yes
2=No
Used for first 1972 interviews:
2: During the past 4 weeks, have you had seizures or epilepsy?
1=Yes
2=No
Used from interview number 1973 onward in place of #2 above:
2a: Since your injury [since the last time we talked to you], has a doctor told you that
you had developed a seizure disorder or epilepsy?
1=Yes
2=No
2b: Are you currently taking any medicines to control your seizure disorder or
epilepsy?
1=Yes
2=No
All questions have response options of ‘refused’, ‘don’t know’, and ‘not applicable’.
12
If an individual had an ICD-9-CM discharge diagnosis code for epilepsy (345.x) or
seizure (780.39) at discharge, or if they responded positively to the epilepsy-related
questions during one of their interviews, their TBI charts were re-abstracted for
additional information pertaining to seizures or epilepsy. Information gathered from
chart re-abstraction included evidence of previous history of seizures or epilepsy, antiepileptic drugs (AEDs) prescribed prior to admission and those prescribed at discharge,
whether the TBI was a result of a seizure, whether a seizure occurred after the TBI and if
so when. The chart re-abstractions were completed prior to the completion of all followup interviews, however, and 30 additional potential cases of posttraumatic epilepsy (PTE)
were identified after interview completion. These cases were not re-abstracted for
additional information, but were evaluated in regard to seizures based on only the original
abstraction and interview information (Figure 2).
Due to changes in questions and skip patterns, we were not always able to determine
the year of epilepsy onset with certainty. Such cases were assigned the year of epilepsy
13
diagnosis. In analyzing incidence, we used epilepsy onset at anytime during the three
years following TBI discharge as our outcome.
Both interview and medical record information were used to determine the presence
of epilepsy prior to and after TBI (see Figure 2). Responses to the questions in Table 8,
and re-abstraction information (when available), were used to determine initial
categorization. After such determination, all cases with some indication of seizures or
epilepsy had all available information reviewed individually by an epidemiologist and by
a certified pediatric nurse practitioner who specializes in epilepsy to determine final
epilepsy categorization. Any questionable cases were discussed by the entire team,
including one or both of the epileptologists.
Individuals with pre-existing epilepsy and those with uncertain status were excluded
from all analyses of PTE. The incidence rate of PTE during the three years following
TBI was calculated based on aggregate data taking into account those individuals not
completing three years of interviews, and confidence intervals (CI) were calculated using
tabulated values for a Poisson-distributed variable. Incidence of PTE was also calculated
stratified by head injury severity using Abbreviated Injury Scale scores, categorized into
mild, moderate, and severe.
Possible factors involved in developing PTE were analyzed using Poisson regression,
with a scale parameter estimated by the square root of Pearson’s chi-square divided by
the degrees of freedom. The independent variables were derived from initial chart
abstraction, chart re-abstraction, and first interview. Independent variables that showed
no significant association with the dependent variable on chi-square analyses (p>0.10)
were excluded from the initial regression model. Fisher’s Exact Test was used in place of
chi-square when appropriate. Outcome variables were PTE and no epilepsy. Unlike the
incidence rate calculation above, since this analysis involved examining individual
characteristics related to outcome, a conservative approach was used and study
participants included in the analyses who did not complete all three years of interviews,
and who did not report epilepsy prior to their last interview, were assumed to have an
outcome of no epilepsy. Table 9 shows information on the independent variables. The
Cochran-Armitage test for trend was used to look for trends in outcome across ordinal
variables.
14
Diagnostics were used to examine the appropriateness of the model. Variance inflation
factors of the independent variables were calculated in an equivalent linear regression
model to check for multicollinearity. The age category 55+ was inflated, but since this
category was necessary in the model it was retained. Variables suspected of interaction
were checked, and none was found. Deviance and Pearson chi-square statistics showed
adequate fit with no evidence of overdispersion. Since there was attrition in the cohort,
those completing three interviews were compared by chi-square to those who did not, to
look for differences.
Of 3,746 eligible persons, 2,118 (57%) were both located and participated in the first
year interview. Of first year participants, 1,536 (72.5%) participated in the 2nd year
interview, and 1,173 (55.4%) participated in the 3rd year interview. ICD-9-CM codes and
interview responses were used to identify 325 potential cases with seizures or epilepsy, and
241 (74%) of their charts were re-abstracted. A total of 115 individuals were determined to
have developed PTE in the three years following discharge for TBI. The incidence of PTE
in the three years was 0.077 per person-year, which is equivalent to 2.6 cases per 100
person-years (95% CI 2.1, 3.1). Incidence by head injury severity was 1.2 cases per 100
person-years (95% CI 0.7, 1.8) for mild, 2.2 per 100 person-years (95% CI 1.3, 3.6) for
moderate, and 3.9 per 100 person-years (95% CI 3.1, 4.9) for severe. See Appendix F
(posttraumatic epilepsy incidence analysis) for more detail on the analysis.
Table 10 shows the characteristics of the cohort by epilepsy status. In this analysis, 834
individuals who did not complete all three annual interviews, if they did not report epilepsy
prior to withdrawal, were assumed to have an outcome of no epilepsy. Compared to
individuals who did not develop PTE, the group with PTE has higher proportions of
individuals who are middle-aged, male, Medicaid recipients, have severe TBI, early PTS,
have sustained their injuries from violence, have no other injuries, have three or more
comorbid conditions, and have a history of a previous head injury, stroke, or depression.
Variables in which no significant difference was seen included race, trauma level status of
hospital, and pre-TBI education, income, and substance abuse. It should be noted that preTBI income was unknown for 7.8% of the cohort, but did not differ between the outcome
groups.
15
Table 9. Independent variables evaluated for the regression model.
Variable and Source
Age – Discharge dataset
Sex - Discharge dataset
Ethnicity - Discharge dataset
Education – Interview report
Income – Interview report
Insurance - Discharge dataset
Severity of TBI – Discharge
dataset
Early posttraumatic seizure –
Re-abstraction information and
any information that
individuals may have
volunteered during interview
Etiology of TBI – Discharge
dataset and original abstraction
Number of concomitant
injuries – Discharge dataset
Number of comorbid
conditions – Discharge dataset
Trauma level status of hospital
– Discharge dataset
Previously knockedout/unconscious – Original
abstraction and interview
History of stroke – Interview
report
History of depression –
Interview report and discharge
dataset
History of substance abuse –
Discharge dataset, original
abstraction, and interview
Additional information on variable
At time of injury
Prior to TBI
In the year prior to TBI
Insurance status at time of discharge was grouped into the following
categories: uninsured, Medicare, Medicaid plus other indigent
programs, and private insurance, which included commercial insurance,
Champus, Worker’s Compensation (WC), other agencies, and unknown.
Commercial insurance made up 87% of the private insurance category.
Unknown was 1% of the total cohort.
Based on AIS (Association for the Advancement of Automotive
Medicine, 1990) score for the head. Assigned by ICDMAP-90 software
(Center for Injury Research Policy of the Johns Hopkins University
School of Public Health, 1997) based on ICD-9-CM codes.
Defined as any seizures within the first month, or if time was unknown,
during the acute hospitalization.
Violence category includes both with and without the use of weapons.
Sports/other/unknown category is 54% ‘other’ and 18% ‘unknown’.
Based on ICD-9-CM codes.
Based on ICD-9-CM codes and Elixhauser et al’s categories.(Elixhauser
et al. 1998)
Interview report of prior episodes of being knocked out or
unconsciousness and/or abstraction information on previous TBI.
Having been told by a doctor that they had a stroke prior to their TBI. In
less than 1% of cases were previous head injury or stroke unknown, and
these were grouped in with those categorized as negative for those
conditions.
Prior to, or at time of discharge from, TBI. Interview report (“Before
your injury, did a doctor ever tell you that you had depression?”) and/or
ICD-9-CM code 296.2, 296.3, 300.4, or 311 (the latter code, for
depressive disorder, was the most common of the 4 codes, representing
72% of individuals with one of these codes). 16% had an ICD-9-CM
code and 84% were self-report only. A total of 95% asserted they had
been told by a doctor before their injury that they had depression.
Prior to, or at time of discharge from, TBI. Based on ICD-9-CM codes
303 through 305 (excluding 305.1), information in chart, and interview
questions on drug and alcohol use.
16
Table 10. Comparison of characteristics in cases with and without posttraumatic epilepsy.
Characteristic
Age :
15-29
30-54
55+
Gender : Female
Male
Race:
Nonwhite
White
Education: <HS grad
HS grad
>HS grad
Income: <$20,000
$20-34,000
$35,000+
Unknown
Insurance: Uninsured
Medicaid/indigent
Private/Other
Medicare
TBI Severity: Mild (AIS=2)
Moderate (AIS=3)
Severe (AIS=4,5)
Early PTS: None known
Yes
Mechanism: Transportation
Fall
Violence
Other/Unknown
Multi Trauma: None
1-2
>=3
No. of comorbidity: None
1-2
>=3
Trauma level: 1
2
3
Undesignated
Hx. unconsciousess: No
Yes
Hx. of stroke: No
Yes
Hx. of depression: No
Yes
Hx. of substance abuse: No
Yes
Posttraumatic
epilepsy
(N=115)
27 (23.5%)
55 (47.8%)
33 (28.7%)
36 (31.3%)
79 (68.7%)
32 (27.8%)
83 (72.2%)
36 (31.3%)
43 (37.4%)
36 (31.3%)
57 (49.6%)
34 (29.6%)
17 (14.8%)
7 (6.1%)
13 (11.3%)
28 (24.4%)
52 (45.2%)
22 (19.1%)
21 (18.3%)
16 (13.9%)
78 (67.8%)
93 (80.9%)
22 (19.1%)
51 (44.4%)
39 (33.9%)
19 (16.5%)
6 (5.2%)
69 (60.0%)
20 (17.4%)
26 (22.6%)
51 (44.4%)
46 (40.0%)
18 (15.7%)
64 (55.7%)
14 (12.2%)
25 (21.7%)
12 (10.4%)
76 (66.1%)
39 (33.9%)
102 (88.7%)
13 (11.3%)
77 (67.0%)
38 (33.0%)
49 (42.6%)
66 (57.4%)
17
No known
epilepsy
(N=1846)
642 (34.8%)
600 (32.5%)
604 (32.7%)
740 (40.1%)
1106 (59.9%)
430 (23.3%)
1416 (76.7%)
613 (33.4%)
608 (33.1%)
614 (33.5%)
943 (51.1%)
441 (23.9%)
316 (17.1%)
146 (7.9%)
210 (11.4%)
242 (13.1%)
949 (51.4%)
445 (24.1%)
744 (40.3%)
306 (16.6%)
796 (43.1%)
1809 (98.0%)
37 (2.0%)
1028 (55.7%)
522 (28.3%)
144 (7.8%)
152 (8.2%)
837 (45.3%)
470 (25.5%)
539 (29.2%)
1069 (57.9%)
683 (37.0%)
94 (5.1%)
900 (48.8%)
273 (14.8%)
430 (23.3%)
243 (13.2%)
1387 (75.1%)
459 (24.9%)
1735 (94.0%)
111 (6.0%)
1479 (80.1%)
367 (19.9%)
895 (48.5%)
951 (51.5%)
Chi-square
p-value
.002
.062
.267
.643
.513
.008
<.001
<.001
.002
.009
<.001
.515
.031
.024
.001
.221
Table 11 shows the risk ratios of the independent variables and their 95% confidence
intervals from the multivariable Poisson Regression. Results show that after adjusting for
all the other variables in the model, individuals more likely to develop PTE had an early
PTS, a severe head injury, three or more comorbid conditions, depression prior to or at
the time of their TBI, and/or Medicaid health care coverage at time of TBI compared to
individuals with the respective referent characteristics. In those variables mentioned
above with multiple categories, the other categories did not show a significant impact on
risk of PTE. For instance, moderate head injury, being insured by private/Worker’s
Compensation(WC)/Champus/other/unknown insurance, being uninsured, and having
one to two comorbid conditions were not significantly related to risk of PTE when
compared to the reference categories. The model was also run with
private/WC/Champus/other/unknown as the reference category for insurance.
Individuals with Medicaid or other indigent insurance showed 2.31 (95% CI 1.38, 3.89)
greater risk than those with private insurance. There were significant trends of increased
risk of PTE with increasing head injury severity (p>.001) and an increasing number of
comorbid conditions (p<.001). There was no significant association noted for the
remaining variables.
Chi-square analyses compared length of participation in the interviews by
characteristics to calculate differential rates of attrition. A larger proportion of
individuals developing PTE participated all three years (p<.001), with 55% of individuals
not developing epilepsy completing all three years, and 70% of those with PTE
completing all years. However, chi-square analyses showed no differences between
length of participation when compared to severity of head injury (p=.891), or any other of
the independent variables except insurance status (p<.001) and education (p=.047).
Individuals participating all three years were more likely to have private insurance and to
have post high school education. The risk of PTE could be falsely inflated if individuals
who were more likely to develop PTE were more likely to participate all three years.
However, since there was no difference in participation by severity or most of the other
variables, it would appear more likely that the longer individuals remained in the cohort,
the more likely we were to identify PTE. This, together with all individuals not
18
developing PTE prior to their leaving the cohort early being given an outcome of no
epilepsy, might have reduced the strength of the actual risk relationships.
Table 11. Risk Ratios of PTE in first 3 years after TBI for 1961 individuals
Risk Ratio
Characteristics (Reference level)
(95% CI)
Age (Ref=15-29 years)
30 – 54
1.63 (0.96, 2.77)
55+
1.19 (0.54, 2.63)
Gender (Ref=Female)
Male
1.36 (0.85, 2.17)
Insurance (Ref=Medicare)
Medicaid or other indigent
3.52 (1.50, 8.25)
Uninsured
1.98 (0.75, 5.19)
Private/WC/Champus/other/unknown
1.52 (0.71, 3.26)
Severity of TBI (Ref=Mild, AIS=2)
Severe, AIS = 4 or 5
2.41 (1.39, 4.17)
Moderate, AIS = 3
1.70 (0.82, 3.50)
Early posttraumatic seizure (Ref=None known)
Yes
6.52 (3.81, 11.17)
Mechanism of injury (Ref=Transportation)
Violence
1.67 (0.89, 3,13)
Fall
1.05 (0.61, 1.83)
Other (incl sports)/unknown
0.61 (0.24, 1.60)
Number of concomitant injuries (Ref =3+)
None
1.26 (0.73, 2.18)
1-2
0.82 (0.42, 1.59)
Number of comorbid conditions (Ref=0)
3+
3.14 (1.57, 6.28)
1-2
1.22 (0.76, 1.96)
Previously knocked-out/unconscious (Ref=No)
Yes
1.30 (0.83, 2.03)
History of stroke (Ref=No)
Yes
1.83 (0.88, 3.80)
History of depression (Ref=No)
Yes
1.86 (1.17, 2.96)
Most studies have focused on clinical factors directly related to the TBI to
determine the risk of PTE. This study differs by including limited clinical factors related
to the brain injury, but a number of demographic, socioeconomic, and clinical factors
occurring prior to the TBI. In concordance with much of the literature, there was an
increased risk of PTE with increased severity.
19
Our study showed early PTS increased the probability of epilepsy more than any
other factors. Our definition of early was liberalized to include seizures within a month
of injury, or if time was unknown, anytime during the acute hospitalization. Since there
was no specific interview question concerning early seizures, and not all charts were reabstracted for additional seizure and epilepsy information, it is possible that we did not
identify all cases of early seizures. Choice of charts for re-abstraction was based on the
presence of epilepsy or seizure discharge codes, or a positive reply to pre- or post-TBI
epilepsy, with most of the early PTS identified through re-abstraction information. The
780.39 code had been used most often in our cohort for pre-existing epilepsy and/or for
early PTS. If there were a large number of cases in which 780.39 was not used for early
PTS, there could be a bias toward identifying early PTS in those developing PTE,
resulting in an inflated association between PTE and early PTS. Unfortunately, while we
know that 780.39 was often utilized for seizures other than early PTS (ie, pre-existing
epilepsy or seizures that caused the TBI) we do not know how often early PTS was not
given a 780.39 code.
Transportation-related injuries were the most common mechanism in our TBI cohort.
In our cohort, falls and violence had the highest proportions of severe head injuries, and
transportation had the greatest proportion of mild head injuries. Mechanism was not
significantly related to risk of PTE.
In our analysis there was no association between the development of PTE and
reporting prior episodes of being ‘knocked out’ or unconscious, or prior substance abuse.
Since alcoholism and the prior occurrence of TBI are more prevalent in individuals with
TBI, and both alcoholism and TBI are related to epilepsy, it could be argued that
including individuals with these characteristics in our cohort may have increased the
incidence of PTE. Ultimately we found no significant relationship between the
development of PTE and either characteristic. We were limited in the amount of
information we collected on previous substance abuse. Substance abuse included both
alcohol and illicit drugs, and was based on ICD-9-CM codes at TBI discharge, self-report
and abstraction information on alcohol or drug treatment, self-report on illicit drug use,
and self-report on current drinking with comparison to pre-TBI drinking (using the
COMBI definition of alcohol use (http://www.tbims.org/combi/subst/index.html)).
20
Since there was no specific measure of alcohol use prior to TBI, some individuals with
prior alcohol abuse may have been missed.
Individuals identified as having depression in our cohort were almost twice as likely
to develop PTE. Although the majority of these individuals were identified solely
through self-report of history of depression (84%), this provides further evidence of
depression as a risk factor not only for epilepsy in general, but also for epilepsy after
head injury.
Individuals in our study showed both an increased risk of PTE with three or more
comorbid conditions at discharge, and a trend of increasing proportion of PTE with
increased number of comorbid conditions. Since stroke can be a predecessor to epilepsy,
especially in older people, we included it as a separate variable. However, people
reporting that they had been told they had had a stroke prior to their head injury did not
show an increased risk of developing PTE. In addition, neither number of concomitant
injuries nor trauma level status of the hospital showed an association with risk of PTE.
In our cohort of TBI patients, no significant difference in risk of PTE between age
categories was found. It must be noted that among the 4,519 people with TBI eligible for
the study, 382 (8.5%) died prior to their first year anniversary of discharge. Of the
deceased, 80% were 55 years and older, while that age group made up only 33% of the
eligible population. Older persons were more likely to die in the first year, likely
removing more seriously injured individuals who would have been at higher risk for PTE,
and thus possibly lowering the reported risk of PTE in that age group and in the cohort.
Our study found no difference in risk of PTE by race, either before or after adjusting for
income, as well as no difference in risk of PTE by gender.
There was no difference in the development of PTE by pre-TBI income or education.
Interestingly, individuals with Medicaid or other indigent assistance on discharge from
their TBI had a significantly increased risk of developing PTE over individuals with
Medicare or some form of private health insurance. It is not known whether SES, quality
or continuity of health care, or some other factor is responsible for this relationship. The
relationship to insurance status remained significant when adjusted for both pre-TBI
income and trauma level status of the acute care hospital. It is possible that those
21
individuals requiring long-term hospitalization became Medicaid recipients prior to their
discharge.
Some limitations of this study have been previously mentioned. Most important is
the reliance on self-report of seizures or epilepsy status, as well as pre-TBI clinical
variables. Individuals could have erroneously reported the occurrence of epilepsy, stroke,
depression, substance abuse, or previous TBI, or have underreported them, since we had
corroborating clinical information in only some cases. It is possible that individuals who
only answered ‘yes’ to the interview question regarding taking medicine for epilepsy
were on medication prophylactically after their TBI. However, this would seem unlikely
because of the fairly long span of time between discharge and the beginning of
interviews.
While recognizing these limitations, our study has the advantages of being
population-based, including large numbers, demographic heterogeneity, three years of
follow-up, and representing all degrees of severity seen among hospitalized TBI. It also
identifies characteristics present either prior to or concurrent with injury associated with
the later development of PTE. While confirming some risk factors established by other
studies, such as early PTS and severity of head injury, our study has identified other
associations with PTE—especially depression, the presence of three or more comorbid
conditions, and Medicaid insurance—that are less well established and warrant further
research. Information on such associations can be used to better predict those at
increased risk of PTE, and may eventually enable early interventions to reduce this risk
or its consequences.
B. Incidence of epilepsy utilizing ED and HD data—A main difficulty in determining
epilepsy incidence is determining the onset of epilepsy. Rarely can a first seizure indicate
epilepsy. In general, this only occurs when an individual has a type of epilepsy with a
distinctive EEG pattern (for example, infantile spasms where the seizure and EEG
findings (hypsarrythmia pattern) are specific to the epilepsy syndrome, or absence
epilepsy where the seizure and EEG findings (3 per second spike and wave pattern) are
specific to the epilepsy syndrome). We decided to take all cases in which the clinician
review indicated a new seizure or new epilepsy case or questionable diagnosis, or if it
22
was a new case but the final diagnosis was questionable, and ask ORS to follow them
forward in time, looking for any additional diagnoses of 780.3 or 345.x. Below are the
numbers of new cases.
Inpatient/ED charts abstracted: 2001 N=2530, 2002 N=1453
• New onset cases, inpt/ED, epilepsy or seizure: 2001 n=307, 2002 n=124
• New onset cases, inpt/ED, questionable final dx: 2001 n=8, 2002 n=1
Physician office visit (POV) charts abstracted (2001 & 2002): N=302
• New onset cases, POV, inpt/ED: 2001 n=8, 2002 n=3
• New onset cases, POV, questionable final diagnosis: none
A total of 451 cases were identified as new onset cases. Seven of the POV cases were
Medicare, and ORS was unable to follow them forward since they do not have any other
years of data for Medicare. The other four cases would have involved enlisting two other
personnel (one from State Health Plan and one from Medicaid), and it was deemed that
the time and expense in tracking just these four would be prohibitive. However, it does
not seem unlikely to assume that most individuals with a new onset seizure would likely
be seen in an ED or as an inpatient, rather than in a physician’s office.
In the case of more than one diagnosis code after clinician review, we assigned a code
hierarchically: 345.x > 780.31 > 345.2, 345.3 > 780.3 > 780.2 > 293.0. The following
440 cases were considered new onset after clinician review:
Dx. After review
?
?
Epilepsy
Febrile
Febrile
Seizure
Seizure
Status
Status
Year
2001
2002
2001
2001
2002
2001
2002
2001
2002
Frequency
8
1
4
51
24
192
78
60
22
The above cases were sent to ORS to follow them forward in time for later 780.3 or
345.x diagnoses. Of note, there were an additional 298 cases in the database in which
new onset could not be determined. Most of these (66%) also had questionable final
diagnoses.
23
For the purposes of determining epilepsy incidence, a case was considered epilepsy if
they had two diagnoses of 780.39 and/or 345.x, with onset considered the initial seizure.
There were 4 cases in which the clinical reviewers had previously assigned or confirmed
a diagnosis of new onset epilepsy. Three of these four cases showed subsequent seizures.
The one without any subsequent seizures recorded at ORS was removed as a new onset
epilepsy case for this analysis. Febrile seizures (780.31) were not counted as seizures. If,
however, an individual with a 780.31 diagnosis had at least two subsequent non-febrile
seizure diagnoses, they were counted as a new onset case of epilepsy, with the onset as
the year of the first febrile seizure. There were six such cases.
The following analysis includes only inpatient and ED cases.
1. ALL INCIDENT CASES FROM SAMPLE
By diagnosis assigned after clinician review, and year:
Year=2001
ASSIGNED CODE
EPILEPSY
SEIZURE
STATUS
Frequency
4
83
31
Percent
3.39
70.34
26.27
Cumulative
Frequency
4
87
118
Cumulative
Percent
3.39
73.73
100.00
Frequency
2
37
15
Percent
3.70
68.52
27.78
Cumulative
Frequency
2
39
54
Cumulative
Percent
3.70
72.22
100.00
Year=2002
ASSIGNED CODE
FEBRILE
SEIZURE
STATUS
By original diagnosis and year:
Year=2001
ORIGINAL CODE
EPILEPSY
SEIZURE
STATUS
Frequency
12
97
9
Percent
10.17
82.20
7.63
Cumulative
Frequency
12
109
118
Cumulative
Percent
10.17
92.37
100.00
Frequency
10
38
6
Percent
18.52
70.37
11.11
Cumulative
Frequency
10
48
54
Cumulative
Percent
18.52
88.89
100.00
Year=2001
ORIGINAL CODE
EPILEPSY
SEIZURE
STATUS
24
2a. TOTAL EPILEPSY SAMPLE PER ABSTRACTION DATA
By original diagnosis and year:
Year=2001
ORIGINAL CODE
EPILEPSY
FEBRILE
SEIZURE
STATUS
Frequency
628
110
1656
136
Percent
24.82
4.35
65.45
5.38
Cumulative
Frequency
628
738
2394
2530
Cumulative
Percent
24.82
29.17
94.62
100.00
Frequency
331
37
989
96
Percent
22.78
2.55
68.07
6.61
Cumulative
Frequency
331
368
1357
1453
Cumulative
Percent
22.78
25.33
93.39
100.00
Year=2002
ORIGINAL CODE
EPILEPSY
FEBRILE
SEIZURE
STATUS
2b. TOTAL EPILEPSY SAMPLE PER ORS
(included status as epilepsy, and febrile as seizure)
By code and year: Year=2001
CODE
2930
345X
7802
7803
Frequency
12
762
66
1690
Cumulative
Frequency
12
774
840
2530
Percent
0.47
30.12
2.61
66.80
Cumulative
Percent
0.47
30.59
33.20
100.00
Year=2002
CODE
2930
345X
7802
7803
Frequency
5
488
47
913
Percent
0.34
33.59
3.23
62.84
Cumulative
Frequency
5
493
540
1453
Cumulative
Percent
0.34
33.93
37.16
100.00
3. TOTAL EPILEPSY POPULATION
(included status as epilepsy, and febrile as seizure)
By code and year: Year=2001
CODE
2930
345X
7802
7803
Frequency
1020
1723
16574
18749
Percent
2.68
4.53
43.54
49.25
Cumulative
Frequency
1020
2743
19317
38066
Cumulative
Percent
2.68
7.21
50.75
100.00
Percent
2.64
3.97
44.36
49.02
Cumulative
Frequency
1057
2646
20395
40007
Cumulative
Percent
2.64
6.61
50.98
100.00
Year=2002
CODE
2930
345X
7802
7803
Frequency
1057
1589
17749
19612
25
The original plan was to choose 35% of 345.x codes (epilepsy), 5% of 780.3 codes
(convulsions), 1% of 780.2 codes (syncope & collapse), and 5% of 293.0 codes (acute
delirium) for 2001. In 2002 we wanted to have a total abstraction of approximately 1500
charts, and inflated that number upward to adjust for expected 15% unlocated charts. As
seen further on, these percents were not exact, possibly due to what charts were able to be
located, change in personnel, as well as the need to determine final percents on one
diagnosis rather than the 2 or more that were sometimes present.
In pulling the sample, ORS allowed those with more than one seizure-related
diagnosis (ie, 780.3 and 780.2) to go into more than one group for pulling the sample.
When sending us the population from which the sample was pulled, we requested ORS
assign one diagnosis to each case, using the hierarchy 345.x>780.3>780.2>293.0, which
is the same one used in assigning diagnoses to the abstracted cases. I believe that this
most likely inflated the proportions of the ‘higher’ diagnoses (345.x and 780.3) since they
would have priority in labeling. In 2001, 2.1% of the cases had 2 seizure-related
diagnoses, and in 2002, 3.0% had 2 seizure-related diagnoses. While ORS was able to
match the individuals back to the appropriate individuals in each year, the personnel
putting together the population dataset was different from that which pulled the original
sample, and they had difficulty matching cases to the exact visit, resulting in some
variation in diagnoses and payers.
Also of note, in addition to the 11 physician office visits that could not be followed
forward, there were 7 HD/ED cases that ORS personnel could not match back to the
database so they was unable to follow them forward. Also, there were an additional 3
HD/ED cases in which the diagnoses from ORS did not match the original diagnoses sent
in the abstraction sample, so those were not followed forward. Together, that is a total of
21 cases which were new onset but were not able to be followed to determine whether
they had additional seizures. Finally, individuals may have moved out of SC or received
ED or inpatient care outside of SC between the year of the abstraction and 2005, and thus
additional episodes of seizure could have been missed. If any of these cases became
epilepsy, it would mean our estimate is an under estimate of the true incidence of
epilepsy.
26
Of the 10 HD/ED cases that could not be matched, all had original diagnoses of
780.31. Eight of them were considered after clinical review to be correct, and two were
reassigned codes of 780.39 since their ages were 10 and 74 years. Eight were 2001 cases
and 2 were 2002 cases. The incorrectly coded cases were both from 2001. Of the 11
physician office visit cases, there were 3 cases from 2001 all of which were originally
coded as seizure, and were considered to be correct after clinical review. The other eight
cases, five from 2001 and three from 2002, were all originally coded as epilepsy, but
were considered to be seizure cases after clinical review.
There were slightly fewer epilepsy diagnoses in 2002 than in 2001 (1589/1723=92%),
and there were slightly more seizure-related diagnoses in 2002 than in 2001
(19612/18749=105%).
Because the sample reflects the population of cases with epilepsy and seizure
diagnoses, we did not weight numbers when applying the sample incidence to the
population. Therefore, total new cases of epilepsy in 2001 are 47 with 345.x diagnoses,
and 1030 with 780.3 diagnoses. Total new cases of epilepsy in 2002 are 60 with 345.x
diagnoses, and 726 with 780.3 diagnoses. In 2001, 2.7% of 345.x cases and 5.5% of
780.3 cases became epilepsy within the next 4 years. In 2002, 3.8% of 345.x cases and
3.7% of 780.3 cases became epilepsy within the next 3 years. Population information
was acquired from SC Statistical Abstract (Table 23), 1990, 2000 and US Census Bureau,
State Population Estimates 2, 3.
Using 345.x (epilepsy & status) and 780.3 (seizures, including febrile) categories:
• Inpt/ED population, 2001: 345.x = 1723; 780.3 = 18,749
• Inpt/ED sample per abstraction, 2001: 345.x = 764; 780.3 = 1766
[Inpt/ED sample per ORS, 2001: 345.x = 762; 780.3 = 1690]
• Inpt/ED incident cases, 2001: 345.x = 21; 780.3 = 97
*2001 cases have at most 4 years of follow-up (through 2005)
• 2001 sample was 44% of 345.x cases & 9% of 780.3 cases.
Inflating incident cases to population results in 47 cases 345.x and 1030 cases
780.3.
• Inpt/ED population, 2002: 345.x = 1589; 780.3 = 19,612
• Inpt/ED sample per abstraction, 2002: 345.x = 427; 780.3 = 1026
2
3
http://www.ors2.state.sc.us/abstract/chapter14/pop23.asp
http://www.census.gov/popest/states/asrh/SC-EST2003-02.html
27
•
•
•
[Inpt/ED sample per ORS, 2002: 345.x = 488; 780.3 = 913]
Inpt/ED incident cases, 2002: 345.x = 16; 780.3 = 38
*2002 cases have at most 3 years of follow-up (through 2005)
2002 sample was 27% of 345.x cases & 5% of 780.3 cases.
Inflating incident cases to total population results in 60 cases of 345.x and 726
cases 780.3.
If NO adjustment for age, sex, or race, using the 2000 SC Census population, result
would be the following:
• 2001: 1077/4,012,000 = 0.00027 = 0.27 per 1000 people incident cases of
epilepsy
• 2002: 786/4,012,000 = 0.00020 = 0.20 per 1000 people incident cases of epilepsy
III. Causes (triggers) of seizures and etiologies of epilepsy
Aim—Determine the underlying causes and etiologies of epilepsy in South Carolina.
In abstracting the data from charts, we asked the abstractors to note any information
on what caused seizures (i.e., ‘triggers’) and the etiology of epilepsy. As part of the skill
building instruction to abstractors, differences between these two concepts were
presented, however we had to acknowledge that this distinction can be difficult for
someone without a clinical background in epilepsy, and that there can be an overlap, such
as the person who experiences a head injury and an immediate seizure, and then goes
onto develop epilepsy, or the person with alcoholism and epilepsy. As shown in
Appendices A&B, we had specific causes individually listed (injury, illness, fever, lack
of sleep, pregnancy, eclampsia, alcohol use, drug use, change in medication, weight gain
in children, noncompliance with medication) to try to prevent them from missing any that
might be mentioned in the chart. We provided a place for narrative for the abstractors to
write any information on causes and etiologies (ie, ‘Brief description of current
circumstances that might have contributed to this seizure or seizure-like episode (what
provoked this seizure?)’, and ‘Any past illness, condition, or injury in the patient’s
history that initially caused the seizure disorder/epilepsy’).
The initial results for cause and etiology had a high proportion of cases in which there
was no information. For instance, in the inpatient/ED abstracted data, only about 20% of
cases had an etiology listed under the actual ‘etiology’ variable. However, in reviewing
the results of the chart abstractions, we noted that there were occasions when the
28
abstractors appeared to mix up cause and etiology, and times when a cause or etiology
was noted among the text in other variables. In an attempt to use all abstracted
information, we have had our pediatric nurse practitioner (GS) who specializes in
epilepsy begin reviewing each case individually. If there are triggers that are mentioned
in the text but not checked off in the categorical variables, then that is corrected. In
addition, we developed a list of categories of etiologies, and she is categorizing text from
the etiology text variable, as well as any possible etiology mentioned elsewhere in the
abstraction. Since there are over 4,000 cases, this has involved a large time commitment.
At present writing, she has completed reviewing 2,000 (50.2%) of the inpatient/ED cases,
and intends to complete all cases as time allows, including physician office visit cases.
The following analyses on the inpatient/ED data are from the 2000 completed cases, and
are limited to those cases determined to be epilepsy after clinician review (n=1,476).
When characteristics of age group, sex, race, and primary payer are compared, the
records reviewed to date (nearly 50%) are reflective of the total group of epilepsy cases.
In reviewing the abstracted data, information that could be used to infer possible
etiologic/causal factors were noted to be in multiple areas. Diagnoses were used to assist
in understanding causes of the seizure for that visit as well as etiologies for epilepsy, but
it should be noted that not all diagnoses were always coded in that section. Instead,
diagnostic information could also be found in chart histories and exams that were quoted
by the abstractors as additional information deemed as important. The information given
often was not complete enough to note if a condition was the etiology or a co-morbid
condition of the epilepsy. (The etiologies list was modified and developed from the
Sander’s article on “The epidemiology of epilepsy revisited.” Please see Table 12
below.) If such information was present, it was taken into consideration. For example,
occasionally a chart would note pre-existing diagnosis of epilepsy but a new onset
cerebrovascular accident (CVA) occurring at the hospital visit being reviewed. If this
occurred, care was taken to avoid identifying the CVA as the etiology of the epilepsy.
However, if CVA was merely listed without any temporal description, an inclusive
approach was taken, and it was included under ‘CVA’. There are known reasons for the
development of secondary epilepsy like Alzheimer’s, substance abuse (although
debated), head trauma, brain tumors, AIDS, secondary metastasis to the brain, lupus, etc.
29
There are also diseases/disorders where the development of secondary epilepsy appears
to occur frequently whether as part of the disease process or treatment, for example,
diabetes, asthma, autoimmune disorders, other cancers, etc. There is also new research
proposed that may identify the increased occurrence of a co-morbid condition, like
depression or anxiety, with epilepsy due to similar pathophysiology. Therefore, all of
these conditions were noted as possible etiologies to be considered. If not specifically
noted as a separate etiology, they were coded as ‘other disease processes’.
Table 12. Potential Etiologies of Epilepsy per Sander†.
A.
Childhood, adolescence and early adulthood
1. Congenital
2. Developmental
3. Genetic
4. Prenatal/perinatal/postnatal factors
5. Febrile seizures
6. Neonatal seizures (not assigned as data do not identify age <12 months)
B.
At any time
7. Head trauma
8. Central nervous system infections
9. Tumors (brain)
10. Substance abuse
11. Other disease process (Alzheimer’s, AIDS, autoimmune, other cancer,
cancer metastases, diabetes, asthma, depression/anxiety renal, etc.)
C.
Elderly
12. CVA
D.
Certain environments
13. Endemic infections (malaria, neurocysticerocosis, paragonomiasis &
toxicariasis)
E.
Family
14. Relative with epilepsy
F.
Unknown/not applicable
15. Unknown etiology
16. No identified epilepsy
†
Based upon Sander, JW. (2003). The epidemiology of epilepsy revisited. Current Opinion in
Neurology. 16, 165-70.
30
Other concerns in using the modified epilepsy etiologies list from Sander include
identifying neonatal seizures and febrile seizures. The data from ORS did not identify the
specific age of an infant between 0 and 11 months. This meant neonatal seizures could
not be identified. Also, this may skew the febrile seizure data, as per our protocol all
children under 6 years of age were considered to have febrile seizure disorder unless
other data was presented which identified another disorder that would rule out febrile
seizures, such as cerebral palsy, infantile spasms, etc. Those children younger 6 months
were not identified so all children listed as 0 years were given a febrile seizure diagnosis
unless other information is included that disputed otherwise.
Based on our chart review, 1,430 unduplicated individuals that were determined to
have epilepsy had been assessed to identify the etiology of epilepsy. In some cases more
than one etiology may be listed for an individual making the total over 100%. Most
commonly, the etiology is either unknown, or is not stated in the chart (see Figure 3
below). The next most common, is ‘other disease processes’. As mentioned above,
etiology is loosely defined, allowing what could be comorbid conditions to be stated as
etiology.
UNKNOWN/NOT STATED
37.5%
OTHER DISEASE PROCESS
28.5%
13.9%
SUBSTANCE ABUSE
CVA
7.6%
HEAD TRAUMA
6.7%
DEVELOPMENTAL
4.8%
NATAL FACTORS
3.8%
2.8%
RELATIVE W/EPILPESY
CONGENITAL
2.4%
TUMORS(BRAIN)
2.2%
CNS INFECTIONS
GENETIC
0.8%
0.8%
FEBRILE SEIZURES
0.6%
0.0%
5.0%
10.0% 15.0% 20.0% 25.0% 30.0% 35.0% 40.0%
Figure 3. Etiology categories of inpatient/ED epilepsy cases
Any possible causes of seizures for a visit were identified from the narrative,
diagnoses, and other variables listed as possible causes. If a person presented with a new
31
onset seizure after head injury, both the new onset seizure and head injury were listed to
increase the information gleaned from the chart review. In addition, if a person with
known epilepsy had no identified cause, the variable of “breakthrough seizure” was used.
The various causes of seizure included in our chart reviews are shown in Table 13.
Table 13. Complete list of cause of seizure
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
AED above therapeutic level
Accidental near drowning
Accidental poisoning
Anorexia
Anxiety
Breakthrough seizure
CVA
Dehydration
Drug overdose
Electrolyte imbalance
Fever
Head injury
Herbal ingestion
Illness
Injury
Job injury
Medication changes
Medication reaction
Menses
MVA
N/A (no seizure related to visit)
New onset seizure
Noncompliance
Postpartum < 1 month
Pregnancy
Respiratory distress
Seizure versus pseudoseizure
Shunt failure
Sleep deprivation
Stress
Structural brain issue
Substance abuse versus using alcohol and/or drugs
Subtherapeutic AED level
Suicide attempt
TIA
Unknown
VEEG admit
VNS (vagal nerve stimulator) placement
VNS replacement
32
In analyzing the immediate seizure causes, cases that were abstracted in both
2001 and 2002 were retained, since seizures may be triggered by different factors at
different times. In this subset, there were 44 cases with data from both years. 542 of the
visits did not involve a seizure, so these were removed, leaving analysis on 952 seizures
that occurred in 928 individuals. More than one cause was allowed making the total
more than 100 percent. The top causes (those >1% in frequency) are listed below in
Figure 4. The most common cause is a “breakthrough seizure”, which indicates the cause
is unknown. That is followed by illness, which indicates a current or recent illness. The
next three causes could be considered preventable: noncompliance, subtherapeutic
antiepileptic medication level, and substance abuse. They could be prevented with
intervention. There are other causes on the list that could be affected by intervention, and
include antiepileptic levels above a therapeutic level, sleep deprivation, and injury.
Counting just the six causes mentioned, over 50% of these epileptic seizures could
possibly be prevented with appropriate treatment, monitoring, and counseling.
Medication changes included only changes to antiepileptic medications, and a video
electroencephalogram admission (VEEG admit) indicated someone admitted for a VEEG
who may have had seizures during the course of the procedure.
28.2%
BREAKTHROUGH SEIZURE
20.6%
ILLNESS
19.7%
NONCOMPLIANCE
15.8%
SUBTHERAPEUTIC AED
13.7%
SUBSTANCE ABUSE
6.2%
MEDICATION CHANGES
4.0%
FEVER
2.8%
AED ABOVE THERAPEUTIC
ELECTROLYTE IMBALANCE
1.8%
VEEG ADMIT
1.6%
SLEEP DEPRIVATION
1.3%
INJURY
1.3%
PREGNANCY
1.2%
0.0%
5.0%
10.0%
Figure 4. Causes of seizure
33
15.0%
20.0%
25.0%
30.0%
We performed similar analysis on the physician office data. This work is still in
progress and results presented in this report reflects only those with a final clinicianreviewed diagnosis of epilepsy (n=276). In looking at etiology, only items listed under
the variables ‘etiology’ and ‘family history’ were considered, with the project
epidemiologist categorizing the etiologies according to the same categories as used for
the HD/ED data. There should be additional information after clinician review. More
than one etiology is allowed making the total is greater than 100%. As with the
inpatient/ED data, the most common category is unknown/not stated. There are
differences between the etiologies of the HD/ED and the POV patients, which could be
due to the differences in both patients and physicians (see Figure 5). For instance, the
increase in known relatives with epilepsy may reflect the more in-depth history taken in a
physician’s office, and the decrease in substance abuse as an etiology may reflect a
difference in where health care is accessed.
UNKNOWN/NOT STATED
62.7%
RELATIVE W/EPILPESY
17.0%
HEAD TRAUMA
CVA
6.9%
5.4%
CNS INFECTIONS
3.6%
NATAL FACTORS
2.9%
CONGENITAL
OTHER DISEASE PROCESS
2.5%
2.2%
SUBSTANCE ABUSE
1.1%
FEBRILE SEIZURES
1.1%
TUMORS(BRAIN)
0.7%
DEVELOPMENTAL
0.7%
GENETIC
0.4%
0.0% 10.0% 20.0% 30.0% 40.0% 50.0% 60.0% 70.0%
Figure 5. Etiology categories of physician office epilepsy cases
The categorized causes are shown below in Figure 6. Only information already
categorized in the data by the abstractors is included. This work is in progress and there
34
will be an update after clinician review of all information. More than one cause is
allowed and the total percent exceeds 100. More than half of the records had no cause
listed for the most recent seizure. The second most common cause was a change in
antiepileptic medication, followed by injury (other than head) and illness.
Noncompliance and substance abuse are not as common among the POV patients as the
HD/ED patients. AED level in these patients was the most recent level done, which may
or may not have been connected to the most recent seizure, so it was examined
separately. In 20% of patients, the AED levels were subtherapeutic, and 17% were above
the therapeutic range.
58.7%
NONE OF THESE LISTED
MEDICATION CHANGES
14.5%
OTHER INJURY
11.6%
10.1%
FEVER
ILLNESS
9.4%
6.2%
NONCOMPLIANCE
HEAD INJURY
5.1%
SUBSTANCE USE/ABUSE
1.8%
SLEEP DEPRIVATION
1.8%
WEIGHT GAIN (PED)
0.7%
PREGNANCY
0.4%
0.0%
10.0% 20.0% 30.0% 40.0% 50.0% 60.0% 70.0%
Figure 6. Causes of seizures among POV patients with epilepsy
IV. Target populations for intervention
A. Medication use - HD/ED data
In abstracting patient charts, we asked the abstractors to note any antiepileptic
medication that the patient was taking at the onset of the visit. To examine medication
use, we looked only at those with epilepsy that is not new onset. If they were abstracted
in both 2001 and 2002 we used the data from 2002. Of 2,950 such cases, 2226 (75.5%)
had their current AEDs listed on the chart. We classified drugs approved by the Federal
35
Drug Administration since 1990 for use in epilepsy as ‘new’, based on their recognition
by the American Academy of Neurology and the American Epilepsy Society as new
generation AEDs. Drugs released prior to this we classified as ‘old’. Table 14 below
shows the percent of patients taking each drug, and its classification. Patients often took
more than one drug making total percent greater than 100. More than half of the patients
were taking phenytoin, an older drug with a fairly significant profile of side effects and
difficult pharmacokinetics. Of the 263 women between the ages of 15 and 44 years, 263
(60%) were taking either phenytoin, carbamazepine, lamotrigine, or valproate, all of
which have recently been shown to be connected to an increased rate of miscarriage and
birth defects.
Table 14. AEDs being taken by inpatient and ED patients (N=2,226).
Trade name
Dilantin, Phenytek
Generic name
Phenytoin
% taking
55%
Type
Old
Depakote/Depakene
Divalproex sodium/Valproic acid
19%
Old
Carbatrol, Tegretol
Carbamazepine
18%
New
Luminal
Phenobarbital
13%
Old
Neurontin
Gabapentin
6%
New
Keppra
Levetiracetam
5%
New
Ativan
Lorazepam
4%
Old
Lamictal
Lamotrigine
4%
New
Topamax
Topiramate
3%
New
Klonopin
Clonazepam
3%
Old
Trileptal
Oxcarbazepine
2%
New
Valium
Diazepam
2%
Old
Zonegran
Zonisamide
1%
New
Gabitril
Tiagabine
1%
New
Mysoline
Primidone
1%
Old
Felbatrol
Felbamate
<1%
New
Zarontin
Ethosuximide
<1%
Old
Tranxene
Clorazepate
<1%
Old
Celontin
Methsuximide
<1%
Old
Depacon
Valproate sodium
<1%
New
36
Patients were grouped according to the number of AEDs they had been prescribed prior
to admission. 70.5% took only one AED, 24.2% took two AEDs, and 5.3% took three or more
AEDs. A logistic regression model was built utilizing the independent variables listed in Table
15. Among individuals who had no insurance were included individuals who were listed as
indigent, or who whose visit was covered under charity. Substance use/abuse could indicate
either past or present, and included alcohol or illicit drugs. Abstractors could mark either ‘yes’
to questions concerning past and present use or abuse if such information was charted, could
mark ‘no’ if past and present use or abuse was specifically denied in the chart, or ‘unknown’ if
use or abuse was not mentioned. The outcome was monotherapy versus polytherapy.
Table 15. Odds of taking more than one antiepileptic drug.
Independent variable
Adjusted odds ratio (95% CI)
Age group
0-21
1.74 (1.14, 2.65)
22-44
2.78 (2.01, 3.84)
45-64
2.15 (1.58, 2.93)
65+
Reference
Gender
Female
0.99 (0.82, 1.20)
Male
Reference
Race
Nonwhite
0.73 (0.60, 0.89)
White
Reference
Insurance
None (plus indigent/charity)
0.50 (0.35, 0.73)
Medicaid
1.30 (0.98, 1.72)
Medicare
1.72 (1.29, 2.30)
Private
Reference
Substance use/abuse
Yes
0.24 (0.14, 0.42)
Unknown
0.42 (0.26, 0.68)
No
Reference
Seizure-related visit
Yes
1.36 (1.12, 1.67)
No
Reference
Individuals under age 65, whites, individuals on Medicare, individuals without substance
abuse or use, and individuals whose visit was seizure-related were more likely to be taking more
than one antiepileptic drug. Gender did not appear to affect whether an individual was on
37
monotherapy or polytherapy. It was also noted that individuals without insurance were more
likely to be on monotherapy than individuals with commercial insurance.
Patients were also grouped according to whether they took only newer AEDS, only older
AEDs, or took a mix of older and newer AEDs. 79.6% took only older medications, 9.5% took
only newer medications, and 10.9% took a mix of the two. Another logistic regression model
was built using the same variables as above, but with an outcome of taking either only a new
AED(s) or a mix of old & new AEDs versus taking only an older AED(s). Individuals were
more likely to be recorded as taking only an older AED(s) if they were over age 65 years, male,
nonwhite, had no insurance, were noted to have substance use/abuse or if that knowledge was
unknown, and if their visit was not seizure-related (Table 16).
Table 16. Odds of taking only ‘older’ antiepileptic drugs.
Independent variable Adjusted odds ratio (95% CI)
Age group
0-21
0.24 (0.15, 0.39)
22-44
0.27 (0.18, 0.40)
45-64
0.65 (0.43, 0.97)
65+
Reference
Gender
Female
0.67 (0.53, 0.84)
Male
Reference
Race
Nonwhite
1.94 (1.54, 2.45)
White
Reference
Insurance
None/indigent
4.82 (2.94, 7.90)
Medicaid
0.99 (0.74, 1.34)
Medicare
1.06 (0.77, 1.48)
Private
Reference
Substance use/abuse
Yes
3.29 (1.79, 6.04)
Unknown
2.34 (1.42, 3.87)
No
Reference
Seizure-related visit
Yes
0.67 (0.53, 0.86)
No
Reference
38
B. Medication use - POV data
As stated earlier, we asked the abstractors to note what AEDs the patient was listed as
taking at the onset of the most recent visit. As a reminder, these are individuals receiving
Medicare, Medicaid, or State Health Plan, and who did not have an inpatient or ED visit
during 2001 and 2002. To examine medication use, we looked only at those with
epilepsy that is not new onset. Patients may be taking more than one AED. Table 17
below shows the percent taking each type. Of 276 such patients, 270 (97.8%) had
Table 17. AEDs being taken by patients attending POV (n=270).
Trade name
Generic name
Carbatrol, Tegretol
Carbamazepine
32%
New
Dilantin, Phenytek
Phenytoin
30%
Old
Depakote/Depakene Divalproex sodium/Valproic acid
18%
Old
Keppra
Levetiracetam
14%
New
Lamictal
Lamotrigine
11%
New
Topamax
Topiramate
11%
New
Neurontin
Gabapentin
9%
New
Luminal
Phenobarbital
8%
Old
Klonopin
Clonazepam
4%
Old
Mysoline
Primidone
3%
Old
Zonegran
Zonisamide
3%
New
Trileptal
Oxcarbazepine
3%
New
Ativan
Lorazepam
2%
Old
Gabitril
Tiagabine
1%
New
Felbatrol
Felbamate
1%
New
Zarontin
Ethosuximide
1%
Old
Tranxene
Clorazepate
1%
Old
Valium
Diazepam
<1%
Old
Celontin
Methsuximide
<1%
Old
Depacon
Valproate sodium
<1%
New
39
% taking Type
medications listed. 93.7% were seen by a neurologist or epileptologist. While the three
most common AEDs are the same, only 30% are taking phenytoin, compared to 55% of
the HD/ED patients. Also, 8% are taking Phenobarbital, compared to 13% of the HD/ED
patients. Newer AEDs are being used among these patients than among the HD/ED
patients. 60.0% took only one AED, 27.8% took two AEDs, and 12.2% took three or
more AEDs. 52.2% took only older medications, 23.7% took only newer medications,
and 24.1% took a mix of the two.
C. Posttraumatic epilepsy
A possible target for intervention in preventing epilepsy could be individuals who
sustain TBI. It was noted in an earlier section of the report that individuals who
developed posttraumatic epilepsy within the first three years of discharge from
hospitalization were more likely to have certain characteristics. Individuals who
experienced early posttraumatic seizures, with more severe head injury, with a history of
depression, with three or more comorbid conditions, and under Medicaid, were more
likely to develop posttraumatic epilepsy. While some of these characteristics are markers
of risk, some of them are amenable to early intervention to allay posttraumatic epilepsy.
Depression as a predisposing factor for epilepsy is fairly new in the literature, but offers
an intriguing avenue for further exploration to determine whether treatment of depression
could affect the incidence of posttraumatic epilepsy.
D. Behavioral Risk Factor Surveillance System data
The BRFSS questions on epilepsy include a question on whether an individual
reporting having been told they have epilepsy have experienced a seizure within the past
three months. Of those individuals reporting one or more seizures within the previous
three months, only 74.0% (95% CI 58.6-89.4) are currently taking a medication to control
epilepsy. While these cases could involve issues of personal choice, nonepileptic
seizures, etc., an important area to explore further would be why over a quarter of
individuals reporting seizures are not taking medication. The BRFSS also included a
question on multivitamin use. Whereas 85% of the general population reported taking a
multivitamin, only 69% of individuals who had been told they had epilepsy reported
taking a multivitamin. This may be an important area of intervention due to the potential
40
effects of antiepileptic drugs. Levels of heavy drinking and obesity were not significantly
different between those reporting epilepsy and the general population. However,
significantly more individuals with active epilepsy (i.e., those taking medication and/or
reporting a recent seizure) were current smokers (36.8%, 95% CI 32.5-45.7) than those in
the general population (22.5%, 95% CI 21.4-23.7). This is another important area for
intervention, considering the cardiovascular effects of smoking on the brain, plus the
interplay of untreated mood disorders and smoking.
E. Focus group data
Six focus groups were held in four different geographic locations throughout SC. The
topic to be explored was to learn what problems and barriers people with epilepsy in SC
face. The specific questions are in Table 18 below. There were 41 individuals who
Table 18. Focus group questions.
1) Please tell the group:
a) Your first name, when you were diagnosed with epilepsy and how controlled your
seizures are now.
b) If you are a parent of someone with epilepsy, please tell us the age of your child at
diagnosis and how controlled their seizures are now.
2) What services, help, information or care exists to help people with their epilepsy needs or
issues? Probes:
a) Have you used any of these services you listed over time? If yes, what was your
experience in using these services?
b) Are there any services you wanted but could not get? If yes, what was the problem?
c) What services or help are missing that you need/needed?
3) How does a person find out about services or help for epilepsy? How did you find out?
a) How might finding out about services be improved?
4) What challenges or problems has epilepsy created in your life over time? Probes:
a) How have these challenges changed throughout your life?
b) What types of things have you found helpful in dealing with these challenges and
managing your condition?
c) What are your thoughts about your future, in relation to epilepsy?
5) In closing, I have one last question that allows you to use your imagination:
a) If you could tell health care providers and policy makers about what it’s like to live
with epilepsy, and what you think they should know, what are some things you would
say?
41
participated, who together represented 31 persons with epilepsy, either themselves or a
family member. While gender and race reflected the population quite well, there were no
individuals over the age of 65 years. All categories of education, employment, insurance,
and marital status were represented. A manuscript detailing the results of the focus
groups has been published (Sample PL. Ferguson PF. Wagner JL. Pickelsimer EE.
Selassie AW. Experiences of persons with epilepsy and their families as they look for
medical and community care: A focus group study from South Carolina. Epilepsy &
Behavior. 9:649-662, 2006.).
The groups identified numerous areas where intervention is warranted among people
with epilepsy. Clinical issues will be addressed later in the report. Other areas they
identified were social isolation, difficulty finding information, difficulty finding and
keeping employment, lack of transportation, the perception and/or reality of epilepsy not
being considered a disability despite the limitations it can carry, and the stigma that
epilepsy continues to carry. They painted a picture of individuals living on the edge of
life, apart from the mainstream, stymied in following their dreams, considered by much
of the population to be disabled yet unable to obtain disability assistance. These are areas
in which intervention is not held back by the need for new clinical developments. Public
education and government action could greatly impact on these outcomes.
V. Severity and subtypes of epilepsy
Aim—Describe the specific categories, subtypes, and severity of epilepsy and seizure disorder
A. HD/ED data—Determining severity of seizures is a difficult task under the best of
circumstances. There is no universally agreed upon scale to measure seizure severity.
While there are some seizure characteristics that can be used, such as frequency of
seizures or type of seizures, it can be argued that severity should be decided by the
individual him- or herself. In addition, severity could include medication side effects, as
was noted by the focus groups. While this information was not collected from the chart
abstractions, information was collected on the number of people with epilepsy on
polytherapy, which increases the likelihood of side effects occurring (see earlier section
on target populations for intervention). We included several variables in the data
abstraction to attempt to get a picture of severity. Unfortunately, there was limited
42
information in the patient charts concerning seizure lengths, types of seizures, etc. The
following is the information that was obtained from the HD/ED charts. The subset
analyzed consists of those cases with a diagnosis of epilepsy after clinician review. Since
information was scarce in many charts, individuals whose charts were abstracted in 2001
and 2002 had information retained in both years.
If the hospital visit involved a seizure (ie, person went to ED because of a seizure,
was admitted because of a seizure, the person had a seizure while at the hospital, etc.)
then the abstractor had to attempt to record the number of seizure episodes, the time of
onset of the seizure(s), and the length of the seizures(s). There were 1701 cases of
epilepsy with a seizure-related hospital visit, which included 48 duplicates.
•
Of the 1,701, 1,281 (75%) had information on number of seizure episodes. Of
those with information, 64.4% had one seizure, 14.1% had two seizures, and
21.5% had more than two seizures.
•
714 cases (42.0%) had information on time of onset of the seizure(s). Of those
with information, 33.8% had a morning seizure event, 28.0% had an afternoon
seizure event, 15.4% had an evening seizure event, and 22.8% had a seizure event
during the night.
•
510 cases (30.0%) had information on the length of the seizure event. Of those
with information, 9.0% had a seizure event lasting less than 30 seconds, 23.5%
had an event lasting up to 2 minutes, 31.2% had an event lasting up to 5 minutes,
and 36.3% had a seizure event lasting greater than 5 minutes.
If there was information in the chart concerning a history of seizures, the abstractor
was to collect information on the number of types of seizures and the frequency of
seizures. There were 2,751 cases of epilepsy with a noted history of seizures, which
included 78 duplicates.
•
Of the 2,751, 300 (10.9%) had information on number of types of seizures. Of
those with information, 68.0% had one type of seizure, 17.3% had two types of
seizures, and 14.7% had more than two types of seizures.
•
Only 172 cases (6.3%) had information on the frequency of their seizure events.
Of those with information, 18.6% had seizures less than once a year, 30.8% had
seizures more than once a year, 11.0% had seizures more than once a month,
43
21.5% had seizures more than once a week, and 18.0% had seizures more than
once a day.
There were 959 charts (including 44 patients abstracted both in 2001 and 2002) with
an epilepsy diagnosis originally in our sample. Four of these charts had two epilepsy
diagnoses recorded. Status epilepticus codes were excluded since they do not necessarily
indicate epilepsy. Figure 7 shows the frequency of each diagnosis. The following are the
definitions of the ICD-9-CM epilepsy codes: 345.0 = generalized nonconvulsive
epilepsy, 345.1 = generalized convulsive epilepsy, 345.2 = petit mal status (epileptic
absence status), 345.3 = grand mal status (status epilepticus, not otherwise specified),
345.4 = partial epilepsy, with impairment of consciousness, 345.5 = partial epilepsy,
without mention of impairment of consciousness, 345.6 = infantile spasms, 345.7 =
epilepsia partialis continua (Kojevnikov’s epilepsy), 345.8 = other forms of epilepsy,
345.9 = epilepsy, unspecified.
70.0%
65.4%
60.0%
50.0%
40.0%
30.0%
20.0%
10.0%
14.0%
3.6%
2.7%
7.4%
1.0%
2.3%
4.0%
345.6
345.7
345.8
0.0%
345.0
345.1
345.4
345.5
345.9
Figure 7. Original epilepsy diagnoses recorded on the HD/ED charts (n=959).
After clinician review of the abstracted information and the previous diagnoses of
seizures and/or epilepsy, there were 3,056 patients with epilepsy diagnoses, with 88 of
the records of these patients abstracted in both 2001 and 2002. Fourteen percent had
more than one epilepsy diagnosis listed. Figure 8 shows the frequencies of epilepsy
diagnoses after clinical review of the abstracted information. These cases include status
codes, as an indication of severity. Furthermore, post-chart review evaluation indicated
44
that 13.1% of those with epilepsy diagnoses were being seen for a status seizure (there
was only one case with a 345.2 diagnosis, representing less than 0.1%). The large
percent of cases with 345.9 is an indication of the scarcity of specific information on the
charts with regard to seizure characteristics. Perhaps, the assignment of this code may
also suggest the lack of continuity of care by a neurologist/epileptologist. It should be
noted that large proportions of epilepsy patients who receive their cares through the ED
are uninsured or underinsured to get the appropriate evaluation.
90.0%
83.7%
80.0%
70.0%
60.0%
50.0%
40.0%
30.0%
20.0%
10.0%
0.0%
7.9%
0.5%
13.1%
4.5% 2.9%
0.2% 0.9% 0.6%
345.0 345.1 345.4 345.5 345.6 345.7 345.8 345.9
0.0%
345.2 345.3
Figure 8. Epilepsy diagnoses after clinician review of the HD/ED charts (n=3,056).
B. Physician Office Visit (POV) data
Data from the 302 patients from POV reflect visits in either 2001 or 2002 and not
seen in an ED or HD during the period of surveillance. Further, these are patients whose
insurance provider is Medicare, Medicaid, or State Health Plan. After clinician review,
276 of the cases were determined to be epilepsy. Salient findings of this evaluation
indicate the following key points.
•
Of the 276 epilepsy cases, 182 (65.9%) had information concerning number of
seizures experienced during their most recent episode of seizure(s). Of those with
information, 75.8% had had one seizure, 15.4% had had two seizures, and 8.8% had
had more than two seizures.
45
•
Only 21 (7.6%) had information recorded concerning the time of the most recent
seizure event. Of those with information, 28.6% had a morning seizure, 14.3% had
an afternoon seizure, 4.8% had an evening seizure, and 52.4% had had a seizure
during the night.
•
102 cases (37.0%) had information about the length of the most recent seizure
event. Of those with information, 30.4% had a seizure lasting 30 seconds or less,
36.3% had a seizure lasting 2 minutes or less, 20.6% had a seizure lasting 5
minutes or less, and 12.7% had a seizure lasting more than 5 minutes.
•
229 cases (83.0%) had information about how many types of seizures the patient
experiences. Of those with information, 83.0% had one type of seizure, 10.9% had
two types of seizures, and 6.1% had more than two types of seizures.
•
In 275 of the charts, there was no indication that this was a visit for a first seizure.
In these cases, the abstractor was asked to collect information on the frequency of
the seizures in the past year. 181 (65.8%) had information on seizure frequency.
Of those with information, 24.3% had seizures less than once a year, 29.3% had
seizure more than once a year, 26.0% had seizures more than once a month, 12.7%
had seizures more than once a week, and 7.7% had seizures more than once a day.
Of the entire sample of 302 physician office visit cases, there were 221 cases with an
original diagnosis of epilepsy. Only one diagnosis for each case was sent to us from the
Office of Research and Statistics (ORS). Figure 9 shows the frequency of the epilepsy
diagnoses. After clinician review, there were 276 cases of epilepsy (see Figure 10). Ten
percent were given two epilepsy diagnoses. There were no cases of status, as would be
expected in an office setting. There are far fewer cases of 345.9 (epilepsy, unspecified)
in the office charts, both among the original diagnoses and after review, due to the
increased information available on seizure specifics in these charts compared to the HD
and ED charts. The most common diagnoses originally on these charts were 345.0,
345.4, and 345.1. After review, the three most common diagnoses were 345.4, 345.1,
and 345.9. We questioned if perhaps the original 345.0 diagnoses were actually recorded
as 345, without the fourth digit, but ORS confirmed that they were actually listed as
345.0.
46
Taken together, information gleaned from HD/ED is less informative than
information gleaned from POV with regard to determination of seizure type and severity.
The limited information on HD/ED data is yet additional evidence about the type and
continuity of care provided to epilepsy patients. Furthermore, the distinct difference is
the large number of patients with epilepsy attending physician offices have insurance
while the large proportion of patients (14.3%) evaluated in HD/ED have no insurance.
45.0%
40.3%
40.0%
35.0%
30.3%
30.0%
25.0%
20.4%
20.0%
15.0%
10.0%
5.9%
5.0%
0.0%
345.0
345.1
345.4
345.5
3.2%
0.0%
0.0%
0.0%
345.6
345.7
345.8
345.9
Figure 9. Original epilepsy diagnoses recorded on the POV charts (n=221).
70.0%
59.1%
60.0%
50.0%
40.0%
30.0%
25.0%
19.2%
20.0%
10.0%
6.2%
0.7%
0.0%
345.0
345.1
345.4
345.5
0.0%
0.0%
0.0%
345.6
345.7
345.8
345.9
Figure 10. Epilepsy diagnoses after clinician review of POV charts (n=276).
47
C. Behavioral Risk Factor Surveillance System (BRFSS) data
The BRFSS collects information on the number of mentally unhealthy, physically
unhealthy, overall unhealthy, and activity-limited days individuals report for the
preceding 30 days. In addition, they ask about disability with the question, ‘Are you
limited in any way in any activities because of physical, mental, or emotional problems?’.
After receipt of the first two years of BRFSS data (2003 and 2004), we analyzed the
epilepsy responses in conjunction with these five variables, which may be considered a
reflection of the severity of epilepsy when compared to the general population results.
The results were published in an MMWR article entitled, Prevalence of epilepsy and
health-related quality of life and disability among adults with epilepsy - South Carolina,
2003 and 2004. (MMWR, October 28, 2005 / 54(42);1080-1082; Centers for Disease
Control and Prevention). We found that individuals with active epilepsy (i.e., taking
medication for epilepsy and/or reported seizure activity in the previous three months) had
more than twice as many mentally unhealthy days, physically unhealthy days, overall
unhealthy days, and activity-limited days than the general population. 17.9% (95% CI
17.1-18.8) reported having disability, compared to 63.5% (95% CI 52.8-73.1) of
individuals with active epilepsy. Even individuals with inactive epilepsy (not currently
taking antiepileptic medications, and no seizure activity in the preceding three months)
had a significantly higher percentage reporting disability (28.2%, 95% CI 19.6-38.7) than
the general population.
VI. Venues and Levels of Care
Aim—Document the venues and levels of care provided to persons with epilepsy
A. Behavioral Risk Factor Surveillance System data—In the final two years of the
epilepsy module for SC BRFSS (2004 and 2005) we asked a fifth question, ‘In the past
year have you seen a neurologist or epilepsy specialist for you epilepsy or seizure
disorder?’. Of individuals who responded that they had ever been told by a doctor that
they had epilepsy, 37.8% (95% CI: 29.4-46.3) responded affirmatively. Of those with
active epilepsy (i.e., currently taking medicine for epilepsy and/or had seizure activity
within the previous three months), 65.9% (95% CI: 56.4-75.5) reported they had seen a
48
neurologist within the past year. Unfortunately, numbers are too small to report by
specific characteristics.
82.6% (95% CI 73.6-91.6) of individuals with active epilepsy reported they had a
personal doctor or health care provider, and 72.9% (95% CI 61.9-84.0) had had a routine
check-up in the past twelve months. Far fewer, however, reported seeing a dentist within
the past twelve months—only 53.5% (95% CI 41.4-65.5) of individuals with active
epilepsy. Since some AEDs can affect oral health, this can be considered an important
part of routine health care for individuals with epilepsy.
A large percentage of individuals with active epilepsy reported there was a time in
the past 12 months when they needed to see a doctor but could not because of cost 38.2% (95% CI 29.0-47.3). In the general population, only 15.6% (95% CI 15.0-16.3)
reported not being able to see a doctor because of the cost. 77.5% (95% CI 68.3-86.7) of
individuals with active epilepsy reported having health care coverage. Although the
confidence intervals do not indicate a statistically significant difference, 86.5% of
individuals with active epilepsy who did not have a seizure within the past three months
had health care coverage, whereas only 68.5% of individuals with a recent seizure had
health care coverage.
B. Physician office visit data—Information gleaned from the SC ORS, for 2001 and
2002 Medicaid and State Health Plan participants suggests gaps in the receipts of care
among those individuals with seizure unspecified diagnosis. Comparison between
persons coded with 345.x and 780.3 indicate differences in the type of care received.
When analyzing only individuals with a 345.x or 780.3 diagnoses, and who had not gone
to an ED or been an inpatient during that time, 75% of those with a 345.x diagnosis had
seen a neurologist, versus 35% of those with a 780.3 diagnosis. This suggests that
diagnosis of 345.x is more likely to be assigned among patients evaluated by neurologists
compared to other physicians. This may have numerous implications on the type of care
received by these patients. First, without specific diagnosis, appropriate medical care,
particularly medication, is less likely to be effective. Second, this may also suggest lack
of neurologists/epileptologists in the state, limiting access to specialty care particularly
for those without good insurance. Third, although blacks account for 30% of the state
49
residents, they represent 38% of the patients who received care through HD/ED in 2001
and 2002, suggesting limited access to specialty care in private practices. Further, among
blacks16.3% and 25.2% are uninsured and Medicaid insured respectively while among
whites 12.5% and 11.6% are respectively uninsured and Medicaid insured. This might
also have implications in access to specialty care since the case mix of uninsured and
Medicaid is very low in POV settings.
C. Focus group data—Barriers to care and accessing epilepsy-related services, and what
life with epilepsy is like were discussed among the focus groups held throughout South
Carolina. Participants reported problems in obtaining an epilepsy diagnosis, with delays
in diagnosis consisting of years. Other findings include the difficulty of life with
epilepsy and the permanency of these difficulties, life-long searches for help with
epilepsy, and how those searches are seldom easy or successful. Also highlighted are
several services that have provided helpful support, and recommendations for potential
improvements in public education, professional training, and helpful interventions.
Participants mentioned difficulty in obtaining clinical information from physicians, and
turning to other sources for information, such as the internet. In addition, there was a
need for information on assistance with low-cost health care providers, and financial
assistance with medication. Additional details on barriers to care are described in detail
in the published manuscript (Sample PL. Ferguson PF. Wagner JL. Pickelsimer EE.
Selassie AW. Experiences of persons with epilepsy and their families as they look for
medical and community care: A focus group study from South Carolina. Epilepsy &
Behavior. 9:649-662, 2006.).
VII.
TBI Among Persons with Seizure Disorder
Aim—Determine the burden of TBI among persons with seizure disorders
A. Pre-existing seizure disorders and TBI—This evaluation utilized surveillance data
collected from statewide HD and ED from1996 through 2005. Pre-existing epilepsy
and/or seizure disorders (ESD) were identified using a comorbid diagnosis of ICD-9-CM
codes 345.xx and 780.39 from either primary or secondary diagnosis fields among
persons with TBI. The underlying assumption for this analysis is that these conditions,
50
by virtue of being chronic in nature, are temporally antecedent to the TBI. Further, the
coding conventions of ICD-9-CM clearly indicate neither 345.x nor 780.39 should be
used for convulsions precipitated by head trauma either immediately or within the first
week of head injury. The corollary of that convention assumes that the higher rate of TBI
among persons with ESD, compared to those without, may suggest the excess burden of
TBI is attributable to pre-existing ESD.
In this evaluation, we systematically analyzed surveillance data on a total of 128,882
unduplicated persons with a diagnosis of TBI. Of these, 4,043 (2.7%) had a comorbid
diagnosis of 345.xx (epilepsy) and/or 780.39 (seizures not otherwise specified). Among
the 4,043 individuals with a comorbid diagnosis of ESD, a subset of records identified
through 2001 (N=2,170), were stratified by diagnosis and a random sample of 100% of
the persons with 345.xx and 50% of the 780.3x diagnoses were selected resulting in
1,145 cases. Of these, the SC Department of Health and Environmental Control
abstractors were able to find and abstract the records of 872 (76.2%) cases. A total of
528 (60.6%) satisfied the case definition of pre-existing ESD, which is defined as
evidence of epilepsy or seizures prior to the onset of TBI validated by: 1) eyewitness
history indicating that the seizure triggered the fall that lead to the TBI, 2) a seizure
related visit at least one month prior to the TBI, or 3) use of antiepileptic drugs prior to
the TBI. There was no significant difference between persons whose records were found
and those whose records were missing regarding demographic and clinical characteristics
(p>0.10). Thus, the data analyzed are at least 61% true ESD patients.
Data analysis included descriptive and analytical comparisons of demographic and
clinical characteristics between those with and without pre-existing ESD. Bivariate and
multivariable logistic regression analyses indicated that all variables retained in the final
model showed association with pre-existing ESD (Table 19). Comparison of crude
proportions and odds ratios showed significant differences between persons with ESD
and those without regarding age, race, severity, payer type, type of injury, other
comorbidities, and repetitiveness of the trauma. Persons with ESD tend to be older,
black, with more than 2 TBI during the time interval, more likely to be injured due to fall
or adverse effects of drugs, and to be insured by Medicaid and/or Medicare then those
without pre-existing TBI. Table 20 shows multivariable adjusted odds ratios. All the
51
variables noted earlier retained statistical significance with the exception of the 65 and
older age group. This effect is due to collinearity with Medicare payer status, which
retained the comparable degree of association with presence of ESD. The observed
associations suggest the implications of ESD in contributing to the cycle of seizure and
the repetitiveness of these injuries. The risk of repetitive TBI is 3-fold among persons
with ESD compared to those without.
To further elucidate the burden of other comorbid conditions associated with persons
with ESD and TBI, we used the comorbidity index developed by Elixhasuer et al. (1) and
evaluated the odds of having the conditions listed in Table 21 as a function of preexisting ESD. Accordingly, age-sex-race adjusted odds ratios indicate significant
association (P<0.05) for six conditions (AIDS, alcohol abuse, paralysis, neurological
disorders, fluid & electrolyte disorders, and coagulopathies).
In conclusion, our findings suggest that persons with ESD carry a disproportionate
burden of TBI. The standardized morbidity ratio of TBI is at least 1.6 to 2.0 times greater
among persons with ESD than what is noted in the general population of the state even
when we assumed the lifetime prevalence rate of epilepsy (2.0%). When the prevalence is
defined as 1.0%, which is the case based on our prevalence report, the morbidity ratio is 3
to 4 times greater that the rate in the general population of the state. Furthermore, the
increased risk of repetitiveness of TBI among persons with ESD is a profound concern
since more head trauma has the potential to aggravate the intensity and severity of
seizure.
52
Table 19. Characteristics of TBI patients by ESD, SC, 1996-2006 (N=128,882).
Characteristics
Age
65+
45-64
35-44
20-34
10-19
0 -9
Mean (SD)
Race/Sex
Black Female
Black Male
White Female
White Male
TBI Severity
Severe
Moderate
Mild
Cause of Injury
Drug adverse/Poison
All Others
Fall
Transport
Struck by/against
Violence
Payer
Medicare
Medicaid
Other government
Uninsured
Commercial
Care Type
Inpatients
Outpatients
TBI Injury Type
Intracranial
Skull fracture
Concussions
Unspecified injury
Comorbidity
3+
2
1
0
Concomitant Injury
No
Yes
Repetitive TBI
2+
1
0
Pre-existing ESD
Yes %
No %
(N=4,043)
(N=124,839)
Crude Odds
Ratio
95% Confidence
Interval
20.2
23.4
16.2
16.8
11.9
11.5
41.2 (24.5)
12.9
13.0
12.1
23.5
19.6
19.0
31.5 (24.0)
2.59
2.97
2.21
1.18
1.00
1.00
2.31-2.91
2.66-3.33
1.96-2.50
1.15-1.33
0.88-1.14
Reference
10.9
26.5
25.8
36.8
12.0
20.5
28.5
39.1
0.97
1.37
0.96
1.00
0.87-1.08
1.27-1.49
0.89-1.04
Reference
39.6
8.3
52.1
11.9
5.8
82.3
5.26
2.26
1.00
4.91-5.62
2.01-2.54
Reference
1.3
28.8
36.8
20.0
5.2
8.0
0.6
14.7
28.4
31.9
13.7
10.8
2.90
2.64
1.75
0.85
0.52
1.00
2.14-3.92
2.33-3.00
1.55-1.98
0.74-0.96
0.43-0.61
Reference
28.5
18.4
2.5
23.2
27.5
13.1
14.8
3.1
30.9
38.1
3.02
1.72
1.12
1.04
1.00
2.77-3.28
1.57-1.89
0.91-1.38
0.95-1.14
Reference
63.6
36.4
23.5
76.5
5.69
1.00
5.33-6.08
Reference
44.4
4.5
23.2
28.0
13.7
4.8
38.2
43.3
5.01
1.45
0.94
1.00
4.64-5.41
1.24-1.70
0.86-1.03
Reference
10.9
14.4
23.6
51.2
2.2
4.3
11.1
82.4
7.99
5.39
3.42
1.00
7.16-8.91
4.90-5.94
3.16-3.70
Reference
57.4
42.6
44.3
55.7
1.70
1.00
1.59-1.81
Reference
6.9
20.3
72.8
2.0
11.9
86.1
4.00
2.02
1.00
3.51-4.55
1.86-2.18
Reference
53
Table 20. Adjusted odds ratios comparing TBI patients with ESD and without (N=128,882).
Characteristic
Age
65+
45-64
35-44
20-34
10-19
0 -9
Race/Sex
Black Female
Black Male
White Female
White Male
TBI Severity
Severe
Moderate
Mild
Cause of Injury
Drug adverse/Poison
All Others
Fall
Transport
Struck by/against
Violence
Payer
Medicare
Medicaid
Other government
Uninsured
Commercial
Care Type
Inpatient
Outpatient
Comorbidity
3+
2
1
0
Concomitant Injury
No
Yes
Repetitive TBI
2+
1
0
Adjusted Odds Ratio
95% Confidence Interval
0.51
1.81
2.15
1.42
1.32
1.00
0.43-0.62
1.58-2.08
1.87-2.47
1.24-1.63
1.15-1.52
Reference
1.20
1.48
0.98
1.00
1.07-1.35
1.36-1.61
0.90-1.06
Reference
1.58
1.09
1.00
1.45-1.73
0.96-1.24
Reference
2.53
2.68
2.02
0.96
0.99
1.00
1.84-3.48
2.35-3.06
1.77-2.31
0.83-1.10
0.82-1.19
Reference
2.50
1.93
1.19
1.17
1.00
2.19-2.85
1.74-2.14
0.96-1.47
1.06-1.28
Reference
3.40
1.00
3.11-3.72
Reference
2.19
2.14
1.83
1.00
1.91-2.51
1.90-2.40
1.67-2.00
Reference
1.65
1.00
1.54-1.77
Reference
2.33
1.33
1.00
2.03-2.68
1.22-1.44
Reference
54
Table 21. Odds of comorbid conditions among persons with TBI by pre-existing ESD
Congestive heart failure
Pre-existing ESD
Yes
No
Freq. (%)
Freq. (%)
117 (2.89) 1235 (0.99)
Cardiac arrhythmias
165 (4.08)
Comorbid Condition
Unadjusted OR
(95%CI)
Adjusted† OR
(95%CI)
2.98 (2.46-3.62)
0.78 (0.63-0.96)
1932 (1.55)
2.71 (2.30-3.18)
0.83 (0.70-0.995)
49 (1.21)
517 (0.41)
2.95 (2.20-3.96)
0.79 (0.58-1.08)
3 (0.07)
63 (0.05)
1.46 (0.46-4.69)
0.37 (0.11-1.21)
32 (0.79)
329 (0.26)
3.02 (2.10-4.35)
0.75 (0.51-1.10)
662 (16.37)
9050 (7.25)
2.51(2.30-2.73)
0.77 (0.69-0.86)
Paralysis
126 (3.12)
518 (0.41)
7.72 (6.34-9.40)
1.77 (1.43-2.19)
Neurological disorders
142 (3.51)
921 (0.74)
4.90 (4.09-5.86)
1.39 (1.14-1.69)
COPD/Asthma
243 (6.01)
2748 (2.20)
2.84 (2.48-3.25)
1.02 (0.88-1.19)
Diabetes
245 (6.06)
3817 (3.06)
2.05 (1.79-2.34)
0.64 (0.55-0.74)
Renal failure
74 (1.83)
454 (0.36)
5.11 (3.99-6.55)
0.99 (0.75-1.30)
Liver disease
50 (1.24)
221 (0.18)
7.07 (5.19-9.62)
1.13 (0.81-1.60)
9 (0.22)
155 (0.12)
1.80 (0.92-3.52)
0.48 (0.24-0.96)
21 (0.52)
45 (0.04)
14.48 (8.62-24.3)
2.18 (1.22-3.92)
8 (0.20)
72 (0.06)
3.44 (1.65-7.14)
0.79 (0.37-1.69)
16 (0.40)
143 (0.11)
3.47(2.07-5.81)
0.81 (0.48-1.39)
76 (1.88)
1000 (0.80)
2.37 (1.88-3.00)
0.70 (0.55-0.90)
22 (0.54)
222 (0.18)
3.07 (1.98-4.77)
0.93 (0.58-1.47)
214 (5.29)
1176 (0.94)
5.88 (5.06-6.82)
1.36 (1.15-1.61)
76 (1.88)
487 (0.39)
4.90 (3.84-6.25)
1.13 (0.87-1.46)
499 (12.34)
3210 (2.57)
5.34 (4.83-5.90)
1.33 (1.18-1.49)
23 (0.57)
227 (0.18)
3.14 (2.04-4.83)
0.91 (0.58-1.43)
Alcohol abuse
253 (6.26)
897 (0.72)
9.23 (8.00-10.65)
2.20 (1.86-2.59)
Drug abuse
145 (3.59)
1637 (1.31)
2.80 (2.36-3.33)
0.94 (0.77-1.13)
Psychoses
92 (2.28)
844 (0.68)
3.42 (2.75-4.25)
0.95 (0.75-1.20)
Depression
105 (2.60)
1144 (0.92)
2.88 (2.36-3.53)
0.88 (0.71-1.09)
Stroke
97(2.40)
590 (0.47)
5.18 (4.17-6.43)
1.13 (0.89-1.42)
Hypotension
69 (1.71)
951 (0.76)
2.27 (1.77-2.90)
0.67 (0.52-0.88)
Valvular disease
Pulmonary circulation
disorders
Peripheral vascular disorders
Hypertension
Peptic ulcer disease
AIDS
Lymphoma
Metastatic cancer
Solid tumor without
metastasis
Rheumatoid arthritis
Coagulopathy
Weight loss
Fluid and electrolyte
disorders
Blood loss anemia
†
Adjusted for age, sex, and race
55
VIII. Data quality
Aim—Evaluate quality of the data and accuracy of the estimates
A. Population and sample information—the sources of the data and the methods of
sampling play a significant role in the determination of data quality. These concepts are
tied to coverage of the data sources and the representativeness of the sample, each of
which determine the external validity of the findings. Coverage refers to the extent to
which all persons in the geopolitical jurisdiction are included in the numerator and such
numerator is reflective of the pool of individuals in the referent population. Sample
representativeness indicates the extent to which every single unit in the frame has an
equal probability of inclusion in the sample such that the aggregate nature of the sample
is truly reflective of the population in the frame. In our surveillance of epilepsy, we made
every effort to insure that the information collected is inclusive and selection is unbiased.
To further elucidate these points, we present key information about the data sources.
1. Hospital Discharge and Emergency Department—the South Carolina Office of
Research and Statistics (SC ORS) houses an administrative billing dataset with
information from all non-Federal acute care hospital discharges and ED visits in SC.
Among the various variables included billing abstracted data are personal identifiers
and up to ten diagnosis codes. As a major partner to the project and a stakeholder in
statewide health and demography data collection, ORS identified a sample of
individuals from 2001 and 2002 with epilepsy (345.x), convulsions (780.3), syncope
and collapse (780.2), and acute delirium (293.0). The latter two codes were included
on the chance that some seizures might be miscoded as syncope or delirium. The
initial plan was to choose 35% of 345.x codes, 5% of 780.3 codes, 1% of 780.2 codes,
and 5% of 293.0 codes for 2001 for a total of approximately 3,000 charts. From the
2002 population we wanted to have a total abstraction of approximately 1,500 charts,
and based on our experience with the 2001 data, inflated that number upward to
adjust for expected rate of 15% unlocated charts. See Appendix G for the HD/ED
sampling plan. Accordingly, ORS identified 3,000 and 1,742 charts from 2001 and
2002 encounters respectively for abstraction. When drawing the 2002 sample, we
decided to allow cases from 2001 to be included in the population. Of the final 2002
56
chart abstractions, 102 (7.0%) of the cases had also been abstracted in the 2001
sample.
ORS sent information from these records to SC Department of Health and
Environmental Control (SC DHEC). DHEC abstractors went to the hospitals and
abstracted information from those records based on the abstraction tool we had
developed. DHEC then sent the abstracted information to ORS, where all identifying
information was removed. The de-identified data was then sent to MUSC. To assist
MUSC in determining history of seizures, ORS also sent a database consisting of the
unique IDs they had assigned each case, along with the diagnosis codes from any
earlier hospital or ED visits with a seizure-related code. MUSC received 3,998
abstractions from ORS (2001 N=2538, 2002 N=1460). This included 5 duplicates
(same chart abstracted twice) and 5 blank abstractions, plus 2 abstractions done that
appeared not to have been part of original sample. Thus, there was a total of 3988
unique abstractions completed (2001 N=2535, 2002 N=1453). We further found that
3 of the charts appeared to have been erroneously coded with 780.39 or 345.x, so we
removed them from analysis, reducing the total to 3985 charts (2001 N=2532, 2002
N=1453). After matching the charts back to the original population, there were two
charts abstracted that were never in original sample. These were excluded from
analysis yielding a total of 3,983 charts with seizure-related (ie, epilepsy,
convulsion/seizure, syncope & collapse, and/or acute delirium) diagnoses (2001
N=2530, 2002 N=1453).
In order to evaluate the representativeness of our sample to the population, we
requested from ORS a dataset with the entire population of unduplicated cases with a
seizure-related diagnosis code in 2001 and 2002, with age group, sex, race, payer, and
diagnosis code grouping (if more than one seizure-related code, grouping assigned
with the following hierarchy: 345.x > 780.3 > 780.2 > 293.0), with abstracted cases
marked. Below is a summary of how well the data for those marked cases matched
with our abstracted data. See Appendix C for a comparison of the proportions of sex,
race, age group, and payer for 780.3 and 345.x diagnoses and year in cases marked as
abstracted versus the population. The following is a brief summary of the finding
regarding comparability of the records abstracted to the information in the frame.
57
1. Age and gender have accuracy of 99.8%
2. Race has a match rate of 99.4%.
3. Payer is 98.1% accurate.
4. Diagnosis from chart review is accurate in 95.2 % of the cases with the
diagnosis listed in UB-92 when arranged hierarchically as 345.x > 780.3 >
780.2 > 293.0.
2. Physician Office Visits—captures individuals not seen in HD/ED setting. ORS is
the repository of the data from physician offices when primary payer is Medicare,
Medicaid, or State Health Plan—an insurance plan for state employees, their
dependents, and retirees. The data format for reporting is based on CMS-1500, a
billing form that includes all variables but inpatient care and related procedures. The
POV report does not include “out-of pocket” payers (self-pay) and these are expected
to be <5% of the patient pool in physician offices. The proportion of self-pay in POV
setting is even expected to be much lower when it comes to persons with chronic
conditions like seizure disorders. We sampled from 2001 and 2002, except for
Medicare, for which we only had 2001 data available at the time of the sampling in
2003. Data abstraction from physician offices was entirely voluntary on their part.
Due to this, the practice from which the sample of charts abstracted from participating
practices was neither random nor representative of all such practices in the state. The
practices that volunteered for chart abstraction were identified and contacted by the
project epileptologist and investigator (BW), asking them whether they would be
willing to have their records abstracted by SC DHEC personnel. He strove to include
a variety of specialties. Overall 90 practitioners agreed to participate, representing 32
family practice, 8 internal medicine, 29 neurology, 8 obstetrics/gynecology, and 13
pediatric specialties. However, some practitioners had no cases represented in the
sample, and some offices could not find the requested records. The final abstracted
sample included data from 46 practices, representing 8 family practice, 6 internal
medicine, 26 neurology, 2 obstetrics/gynecology, and 4 pediatric specialties, however
most of the population was from neurology offices. We asked the abstractors to note
the type of specialty visit for each case. They recorded the following distribution: 9
from primary care, 199 from neurology, 83 from epileptology, and 11 unknown.
58
Cases were restricted to those individuals who had no encounter in either HD or ED
in SC during 2001 or 2002. The rationale for this was to have two exclusive
groups—those seen in HD/ED setting, and those seen in a POV setting. ORS
estimates that during the surveillance period, Medicare, Medicaid, and SHP covered
approximately 39% of the population of SC. We initially attempted to abstract 400
charts. Due to difficulty finding the charts, a series of four samples were eventually
drawn to reach a revised target of 300. Out of a total drawn sample of 581 charts, 302
(52.0%) were found and abstracted. We initially planned on pulling a ratio of 8:2,
epilepsy to seizure codes. However, as the sampling progressed, more seizure codes
were included as necessary to reach our target goal. Due to limited information at
ORS, Medicare charts were the most difficult to find, and could only be sampled from
2001. (Please see Appendix H for the physician office visit sampling plan.)
The HD/ED sample showed that all cases pulled with a 293.0 or 780.2 code also
had either a 345.x or 780.3 codes. The sampling strategy for the office charts was
restricted to only 345.x and 780.3 diagnoses. Rather than allowing cases with more
than one seizure-related diagnosis to be pulled under either diagnosis, this sample was
pulled using only one diagnosis for each case, and it is unknown whether the cases
had a second seizure-related diagnosis. However, we feel second diagnoses were
likely rare, since in examining the HD/ED data, and looking only at 780.3 and 345.x
codes on the charts, there were only 16 (0.8%) cases in 2001 that had more than one
of those diagnoses, and there were only 12 (0.6%) cases in 2002 that had more than
one of those diagnoses. Assuming that more than one epilepsy or seizure code per
chart is equally as rare in the POV charts, there should be minimal effect from
limiting to one seizure-related code. As mentioned above, to compare our sample
with the population, we requested from ORS a dataset with the entire population of
unduplicated cases with a seizure-related diagnosis code in 2001 and 2002 (only 2001
available for Medicare), with age group, sex, race, payer, and diagnosis, with
abstracted cases marked, for each of the three payer groups. Below is a summary of
how well information acquired through chart review correctly matched with the POV
data from ORS. Due to initial matching error of the unique identifiers, this analysis is
restricted to 246 (81.5%) of the records. Please see Appendix D for a comparison of
59
the proportions of the characteristics seen below in cases marked as abstracted versus
the population. The following is a brief summary of the finding regarding
comparability of the records abstracted to the information in the frame.
1.
Age and gender have accuracy of 98.8%
2.
Race has a match rate of 99.6%.
3.
Payer is 75.6% accurate.
4.
Diagnosis from chart review is accurate in 92.3 % of the cases with the
diagnosis listed in CMS-1500 when arranged hierarchically as 345.x >
780.3.
B. Predictive Value Positive (PVP) and Sensitivity of seizure and epilepsy codes—PVP
reflects the ability of the ICD-9-CM codes assigned in administrative datasets to correctly
identify epilepsy cases. Conversely, sensitivity implies the extent to which true cases and
true non-cases of epilepsy from medical records are correctly differentiated by the codes
in the administrative datasets. While sampling is often driven by the codes assigned in
the administrative datasets, the prospect of correctly conducting sensitivity is likely to be
biased since a priori case selection from medical charts is difficult at best and impossible
at worst. Thus, emphasis of this evaluation is on PVP while Sensitivity will be
interpreted with caution.
1. HD and ED Data—to determine PVP and Sensitivity, codes were arranged in
hierarchical manner: epilepsy (345, 345.0, 345.1, 345.4, 345.5, 345.6, 345.7, 345.8,
345.9) > status (345.2, 345.3) > seizure (780.3, 780.31, or 780.39.) > syncope (780.2)
> delirium (293.0). In our sample it happened that any original 780.2 and 293.0
codes were always accompanied by either a 780.3 or a 345.x. In some cases, some
of the charts have more than one seizure-related codes and any one of these codes
were used to validate PVP and sensitivity. Table 22 summarizes the diagnosis codes.
60
Table 22. Inpatient/ED diagnoses before and after abstraction review.
Diagnosis after Clinician Review
Original
Diagnosis
Epilepsy
2001
2002
Seizure
2001
2002
Status
2001
2002
All
•
Total
Epilepsy
Seizure
Status
Syncope
Unknown
545 (86.8%)
296 (89.4%)
24 (3.8%)
15 (4.5%)
3 (0.5%)
3 (0.9%)
0
0
56 (8.9%)
17 (5.1%)
628 (15.8%)
331 (8.3%)
1231 (69.8%)
809 (78.9%)
303 (17.2%)
127 (12.4%)
74 (4.2%)
20 (2.0%)
2 (0.1%)
1 (0.1%)
155 (8.8%)
69 (6.7%)
1765 (44.3%)
1026 (25.8%)
99 (72.3%)
76 (79.2%)
1 (0.7%)
1 (1.0%)
36 (26.3%)
19 (19.8%)
0
0
1 (0.7%)
0
137 (3.4%)
96 (2.4%)
3056 (76.7%)
471 (11.8%)
155 (3.9%)
3 (0.1%)
298 (7.5%)
3983 (100%)
Epilepsy—there were 959 cases coded as epilepsy in the HD/ED coding
scheme. After clinician review, 841 (87.7%) of these were considered correct
as epilepsy codes. 39 (4.1%) of them were considered to be a 780.3 code, 6
(1%) were considered to be status epilepticus (345.2, 345.3), and 73 (7.6%)
were considered to not have enough information to assign a diagnosis.
•
Seizures—there were 2,791 cases with seizure codes. After clinician review,
430 (15.4%) were considered correct as a seizure code. 2,040 (73.1%) were
considered to have a history of epilepsy, 94 (3.4%) were considered to be
status epilepticus, 3 (<1%) were considered to be syncope (780.2), and 224
(8.0%) did not have enough information to assign a diagnosis.
•
Status—there were 233 cases with status epilepticus codes (345.2, 345.3).
After clinician review, 55 (23.6%) were considered to be correct as status
epilepticus. 175 (75.1%) were considered to have a history of epilepsy, 2
(<1%) were considered to be 780.3, and 1 (<1%) was considered to not have
enough information to assign a diagnosis.
•
Febrile Seizure—there were 110 patients coded as febrile seizure, of which 96
(87.3%) were correct. 8 (7.3%) were determined to have epilepsy after
clinician review.
2. POV Data—determination of PVP and Sensitivity from POV generally followed
the same principle with codes were arranged in hierarchical manner but only for
61
epilepsy and seizure codes: epilepsy (345, 345.0, 345.1, 345.4, 345.5, 345.6, 345.7,
345.8, 345.9) > status (345.2, 345.3) > seizure (780.3, 780.31, or 780.39.). There
were no other codes sampled from the POV dataset. As mentioned earlier, while the
sampled observations were randomly selected, the offices from which the sample of
charts was pulled were a convenience sample. However, there appears to be
comparability between the samples drawn and the frame regarding some of the
characteristics. After removing the 11 cases in which there was not enough
information to determine a diagnosis after review, there were 165 and 126 records
sampled for 2001 and 2002 respectively. Seventy-three percent (213) of the records
had an original diagnosis code of epilepsy while 27% (78) records had seizure as the
original diagnosis.
3. Estimates of PVP and Sensitivity for HD/ED data—using the clinical reviewers’
evaluation as the “correct” classification, we generated the following estimate for the
sources. While the PVP of epilepsy codes range between 95% and 96%, the
corresponding value for seizure codes remain very low (20% and 14% for 2001 and
2002 respectively). This suggests that 80-86% of the cases coded as seizure are
epilepsy codes, while 95% of the cases coded as epilepsy are true epilepsy cases.
Unfortunately, 780.3x is the most prolific code in the seizure category and the ratio of
345.x to 780.3x is 1:11. It should be noted that until proven otherwise, 780.3 codes
should be presumed as epilepsy cases for surveillance purposes. With the constraint
of the sampling scheme in mind, 780.3x codes have high sensitivity due to the large
proportion false positive cases they capture. Conversely, the sensitivity of 345.x
codes is very low due to the small number of false positive cases they capture (please
see the calculation in the prototype tables shown by year).
Code assigned after clinician review
Epilepsy Seizure Total
HD/ED Epilepsy
545
24
569
UB-92
Seizure
1236
304
1540
code
Total
1781
328
2109
PVP of 345.x = 545/569 = 96%
PVP of 780.3 = 304/1540 = 20%
Sensitivity of 345.x = 545/1781 = 31%
Sensitivity of 780.3 = 304/328 = 93%
Code assigned after clinician review
Epilepsy Seizure Total
HD/ED
Epilepsy
296
15
311
UB-92
Seizure
811
127
938
code
Total
1107
142
1249
PVP of 345.x = 296/311 = 95%
PVP of 780.3 = 127/938 = 14%
Sensitivity of 345.x = 296/1107 = 27%
Sensitivity of 780.3 = 127/142 = 89%
2001
2002
62
4. Estimates of PVP and Sensitivity for POV data—as indicated in the
aforementioned description, all procedures for estimating PVP and sensitivity
remained the same. The estimated PVP for POV is even higher than what was noted
in the HD/ED dataset. Estimate range between 94% and 97%, the corresponding
value for seizure codes remain much lower at 4% and 6% for 2001 and 2002
respectively. This lower rate for seizure codes is mainly accounted by the very small
number of patients coded with 780.3x in POVs. Perhaps the large part of this might
be the client pool of patients in physician offices who already have well-established
diagnoses. The tables below show the calculated values for the two measures for
2001 and 2002
Code assigned after clinician review
Epilepsy Seizure
Total
POV
Epilepsy
108
7
115
code
Seizure
47
3
50
Total
155
10
165
PVP of 345.x = 108/115 = 94%
PVP of 780.3 = 3/50 = 6%
Sensitivity of 345.x = 108/155 = 70%
Sensitivity of 780.3 = 3/10 = 30%
2001
2002
POV
code
Code assigned after clinician review
Epilepsy Seizure Total
Epilepsy
95
3
98
Seizure
27
1
28
Total
122
4
126
PVP of 345.x = 95/98 = 97%
PVP of 780.3 = 1/28 = 4%
Sensitivity of 345.x = 95/122 = 78%
Sensitivity of 780.3 = 1/4 = 25%
As a summary, the PVP of 345.x codes is very high across the two data sources.
Persons coded with 345.x are about 95% of the time true epilepsy cases. However,
70-80% the persons coded with780.3x are misclassified as seizure. Sensitivity as a
measure of data validity is not reliable due to the difficulty of the sampling scheme.
C. Algorithm to identify epilepsy patients from administrative datasets—among the
major achievements of our project is the lessons learned and the experience amassed on
identifying critical components of the clinical decision making process. The two
epileptologists (BW and RT) and the neurology nurse practitioner (GS) have a
cumulative total of 65 years of clinical experience in neurology and epileptology. The
extensive and elaborate data abstraction tool along with the 3,983 charts that have been
reviewed provided very useful information to develop an algorithm among commonly
miscoded differential diagnoses of seizure disorders. Hence, we developed four sets of
algorithms regarding persons coded as Syncope (780.2), Febrile Seizure (780.31), Seizure
NOS (780.39), and Epilepsy (345.xx), each of which are described below.
63
1. For cases coded as 780.2: Syncope--If a visit is coded as 780.2 but previous visits
are noted as coded for 780.39 or 345, then the diagnosis is less likely to be 780.2 and
it is important to consider 780.39 or 345. If antiepileptic medications (AEDs) are
listed or an AED drug level was done, then it is less likely to be 780.2 and 345 should
be more strongly considered. If there is presence of a vagal nerve stimulator (VNS),
VNS interrogation/parameters adjusted (CPT codes 95970 or 95974) or VNS
implanted, the code 345 must be considered. If there is a diagnosis for a genetic,
neurologic, developmental or metabolic disorder, it is less likely to be 780.2 and more
likely to be 345. If there is a code for epilepsy surgery, then the code is a 345 and
780.2 should not be coded. Figure 11 depicts the decision path for 780.2.
2. For visit coded as 780.31: Febrile seizure disorder—if a person is less than 6
months or greater than 6 years and has been coded as a febrile seizure disorder, then
that code is incorrect due to the diagnostic criteria and should be changed to a 780.39
or 345 code. If there is a concurrent illness that could cause fever and/or fever is
coded, then 780.31 is the likely code. If a visit is coded as 780.31 but previous visits
are noted as coded for 780.39 or 345, then the diagnosis is less likely to be 780.31 and
it is important to consider 780.39 or 345. If antiepileptic medications (AEDs) are
listed or an AED drug level was done, then it is less likely to be 780.31 and 345
should be more strongly considered. If there is presence of a vagal nerve stimulator
(VNS), VNS interrogation/parameters adjusted (CPT codes 95970 or 95974) or VNS
implanted, the code 345 must be considered. If there is a diagnosis for a genetic,
neurologic, developmental or metabolic disorder, it is less likely to be 780.31 and
more likely to be 345. If there is a code for epilepsy surgery, then the code is a 345
and 780.31 should not be coded. Figure 12 is a graphic depiction of the decision rules
for 780.31.
64
Figure 11 Decision algorithm for 780.2 code
3. For visits coded as 780.39: Seizure, NOS—if a visit is coded as 780.39 but
previous visits are noted as coded for 780.39 or 345, then the diagnosis is less likely
to be 780.39 and it is important to consider 345. If antiepileptic medications (AEDs)
are listed or an AED drug level was done, then it is less likely to be 780.39 and 345
should be more strongly considered. If there is presence of a vagal nerve stimulator
(VNS), VNS interrogation/parameters adjusted (CPT codes 95970 or 95974) or VNS
implanted, the code 345 must be considered. If there is a diagnosis for a genetic,
neurologic, developmental or metabolic disorder, it is less likely to be 780.39 and
more likely to be 345. If there is a code for epilepsy surgery, then the code is a 345
65
and 780.39 should not be coded. Figure 13 is a graphic depiction of the decision rules
for 780.39.
Figure 12. Decision algorithm for 780.31 code
4. For visits coded as 345.xx: Epilepsy disorders—if a visit is coded as 345 but
previous visits are noted as coded for 780.39 or 345, then the diagnosis is less likely
to be 780.39 and it is important to consider 345. If antiepileptic medications (AEDs)
are listed or an AED drug level was done, then 345 should be more strongly
considered. If there is presence of a vagal nerve stimulator (VNS), VNS
interrogation/parameters adjusted (codes 95970 or 95974) or VNS implanted, the
code 345 must be considered. If there is a diagnosis for a genetic, neurologic,
66
developmental or metabolic disorder, it is more likely to be 345. If there is a code for
epilepsy surgery, then the code is a 345. Figure 14 is illustrative chart of the decision
procedures to establish or rule out the diagnosis of epilepsy.
Figure 13. Decision algorithm for 780.39 code
67
Figure 14. Decision algorithm for 345.xx code
D. Data quality measures—we implemented various measures to ensure the quality of
the data collected and to improve the process by which medical charts are abstracted.
The following are the processes and activities involved to asses the quality of the data
collected.
1. Abstraction tool—the tool for collecting standardized data from HD/ED medical
charts was developed by the epidemiologists and clinicians. It was piloted by the
abstractors, and changes were made accordingly. After the 2001 charts had been
abstracted, improvements were made in the abstraction tool based on the data
collection experience, including the removal of some variables with low yield, prior
68
to collection of data from the 2002 charts. In addition, as needed, the tool was
modified to collect information from physician office charts, and to collect
information from charts of individuals with TBI with a diagnosis or self-report of
seizures or epilepsy.
2. Training workshops for data abstractors. An initial 2 ½ day training workshop
was held for the abstractors. It presented information on epilepsy and data quality,
and introduced the data abstraction tool. It included group practice with practice
charts and the abstraction tool, and then individual chart abstractions in a group
setting, allowing for questions and discussion on the abstraction tool. Feedback
collected was then incorporated into the abstraction tool. Subsequent annual
workshops were held to review key information, provide feedback, introduce changes
in the abstraction tool, and allow for discussion and practice abstraction.
3. Training for abstraction reviewers assigning diagnosis codes. Initially, one
clinician—a pediatric nurse practitioner specializing in epilepsy (GS)—reviewed each
abstraction to determine, based on the available information, whether the originally
assigned code was correct, and if not, to assign the most appropriate code. An
epileptologist agreed to act as our ‘gold standard’ for the review. Due to the volume
of cases, two additional clinicians were hired to review cases (one adult epilepsy
nurse, and one pediatric epilepsy nurse). They were given information on the project
and the protocol, as well as 40 practice cases to review. After review, all four
clinicians met to discuss the practice cases prior to beginning reviews. After official
reviews began, the three reviewers plus the epileptologist were twice given the same
set of cases to review individually, and then the group would meet to discuss any
discrepancies or other issues. 20 of the 2001 cases were reviewed like this, with 80%
agreement. 26 of the 2002 cases were also reviewed. In this group, there was low
agreement when looking for agreement to fourth place (345.x). However, if looking
at whether seizure/status epilepticus (780.3 or 345.3) versus epilepsy (all other 345),
then the proportion of agreement improved. There were a number of cases in which 1
or 2 reviewers noted ‘not enough information’ rather than putting a diagnosis but the
rest of the reviewers agreed on the diagnosis. In addition, there were 100 cases
69
reviewed by two of the reviewers, with agreement between these reviewers ranging
between 86-89%.
4. Protocol for assigning diagnosis codes. A protocol, based on International
League Against Epilepsy guidelines, was developed (see Table 23) for use in
assigning ICD-9 epilepsy and/or seizure diagnoses to cases after abstraction review.
This was created with input from our CDC technical advisor and consultant
epileptologists. As work progressed the protocol was added to or changed as needed.
If changes were instituted that might affect previous abstraction reviews, those cases
were pulled and reviewed again to maintain consistency in assignment of diagnoses.
5. Additional information on previous epilepsy/seizure diagnoses. To assist the
clinicians in assigning diagnosis codes and to collect incidence information, ORS
provided a database containing the assigned unique IDs of the cases, and any
instances of previous inpatient or emergency department diagnoses of seizure or
epilepsy.
6. Re-abstractions of medical charts. Approximately a 5% sample of the 2001 charts
was drawn (n=126), and were re-abstracted by one of the abstractors. These reabstractions were then compared to the original abstractions of the same charts
(n=122; 4 charts did not match back), using McNemar's test for 2 ×2 tables and
Bowker's test of symmetry for tables with more than two response categories. Kappa
statistics were calculated on categorical variables to determine consistency in
abstraction. Kappa values (simple, weighted, and exact, as appropriate) ranged from
negative numbers through 1.0. Weighted kappas could not be done on some ordered
values, however, due to inclusion of a missing category. Most 100% agreements
were in variables in which no data was found in the chart. Excluding the variables
discussed below, of the 42 categorical variables compared, the test of H0:kappa=0
resulted in 30 comparisons (71%) with p-values <0.05, and the remaining 12 (29%)
with p-values >= 0.05. In two areas of abstraction, there was the chance to record
information in text form
70
Table 23. Protocol for reviewing ICD-9-CM codes of abstracted cases.
A. Definition of correct coding entries:
1. Yes – correct code noted
2. No – incorrect code noted
3. No* - correctly identified seizure diagnosis but this is an unknown type of epilepsy disorder due to
history of seizures
4. ? – not enough information to know correct diagnosis code to assign
If there are two seizure-related codes assigned, and both are correct, then Correct Code = ‘yes’.
If there are two seizure-related codes assigned, and both are incorrect, then Correct Code=’no’, and the
correct codes are filled into the Primary Diagnosis and Secondary Diagnosis boxes.
If there are two seizure-related codes assigned, and one is correct and one is incorrect, then Correct
Code=’no’, and the correct codes are filled into the Primary Diagnosis and Secondary Diagnosis boxes,
meaning one of the codes (the correct one) will remain the same.
B. Reviewers will use an Epi Info program to enter information to ease both entry and retrieval.
C. Coding review protocol
1. Clinical definition: A case of epilepsy is a person who has ever experienced episodic, sudden, and
usually unprovoked attacks of subjective experiential phenomena, altered awareness, involuntary
movements, or convulsions due to a chronic, underlying CNS process (Pedley, 1996).
2. Operational definition: A case of epilepsy is a person who experienced ≥ 2 usually unprovoked seizures.
D. Rules agreed to:
1. An alcohol-provoked seizure with a history of seizures (even if also most likely all alcohol provoked)
should be coded as epilepsy (345.9).
2. A first seizure with an abnormal EEG is still coded as seizure (780.39) unless there is information noting
a defined epilepsy syndrome on EEG.
3. If there is a history of epilepsy, even if remote, and a seizure (provoked or unprovoked) occurs, it should
be coded as epilepsy.
4. If the child has a new onset seizure with fever and is less than or equal to 6 years old, it is coded as
febrile seizure (780.31). If verified as 780.31, but h/o seizures, include 345.x code only if other
seizures not febrile seizures (see #3 above).
5. If there is incomplete information about the seizure, and there are no contradictions to the assigned
diagnosis, defer to the MD’s diagnosis.
6. If a case is coded as 780.39, and there is a history of seizures, but not enough information provided to
determine type of epilepsy, it should be coded as 345.9 and noted as No* to capture the under
diagnosis of epilepsy cases.
7. If a child has an extended febrile seizure (>5 minutes), code for both 780.31 and status (best to use both
for all status, for purposes of billing, would probably use status code which explains higher costs –
unsure what coding rule is).
8. Except in the case of febrile seizure, a first seizure that is prolonged is coded as status rather than as
780.39.
9. If there is a history of non epileptic seizures, but there is other evidence that there is also a history of
seizures (ie, taking multiple AEDs, h/o etiologic event such as CHI, etc.) then must code as epilepsy,
and include 780.39 if pseudoseizure involved.
10. What about an individual with h/o seizures, who comes in with a seizure, and is coded with 780.39 as a
primary diagnosis, and a 345.x as a secondary diagnosis? Should both codes be used? No, use 345.x.
11. If individual has 345.7, but does not have epilepsia partialis continua, then change to 345.3, and 345.4
or 345.5. Nonstop partial seizure activity required for a diagnosis of 345.7.
12. If individual has status epilepticus diagnosis is given, and rescue medications are used, then status
diagnosis is kept regardless of time noted for seizure. If diagnosis of status epilepticus is given, but no
seizure time or medication intervention is noted, keep status code as all information may not be
available in chart, and defer to physician coding.
71
(narrative of seizure, narrative of cause of seizure) and categorical form (list of
seizure characteristics, list of possible seizure causes). The categorical variables
usually formed 2x2 tables, with most values clustering in one cell, causing difficulty
in interpreting the Kappa value. In addition, the abstractors might record the
information in only text or category form, rather than recording in both places.
Text variables were compared on percent agreement in meaning. Of the 13
analyzed, 1 was in the 60-69% range, 4 in the 70-79% range, 3 in the 80-89% range,
and 5 in the 90-99% range. Most often, discrepancies were not disagreement, but
rather missing information in one abstraction versus the other. One key variable,
whether the seizure, if one occurred during the visit, was considered new onset, had
low agreement. However, clinician reviewers re-assessed this variable for all cases,
and had additional information from ORS for some of the cases (see #5, above).
7. Individual reviews of abstractions and diagnosis code assignment. Data was
cleaned by looking for outlying or illogical values and addressing the issue with ORS
or the clinical reviewers, addressing those cases noted by the clinician reviewers to
have a clinical or administrative issue, and updating any previously reviewed cases if
there was a protocol change.
IX. Dissemination of Results
Aim—Maximize the scientific impact of the study through dissemination of the findings and
involvement of field experts in data analysis and manuscript development.
A. Purpose and plan of dissemination—information dissemination has remained an
important component of SCESESD. It includes various methods that allow diffusion of
knowledge and experience through various medium of communication. The project
strove continuously to keep stakeholders, i.e., policy makers, families, healthcare
providers, state and federal agencies, advocacy groups, and persons with epilepsy,
informed about the progress on all activities including data findings. Dissemination of
the study findings in scientific publications and presentation is a critical priority. The
project encourages all investigators, staff, and the CDC Technical Advisor to participate
72
in manuscript development in accordance with the suggested set of rules by the
International Council of Medical Journal Editors and the SC Data Oversight Council.
The following are venues that allow dissemination of the study methods, approaches,
activities, and findings.
1. Reports—prepared quarterly, semiannually, and annually were the major venues
utilized to engage the CDC and AAMC advisors and other stakeholders. We
attempted to provide interim results of the data generated and analyzed. The Steering
Committee and the Epilepsy Foundation of South Carolina (EFSC) have received
customized data for seeking legislative assistance.
2. Data Codebook and Dictionary—plan is underway to compile the extensive
documentation developed during the course of the study. This included the data
abstraction manual and data dictionary, the various coding protocols, the algorithm,
the IRB protocol, and the procedure manual for quality assurance and analysis.
3. Website—we developed a link to our sister project on epilepsy, the SC Health
Outcome Project on Epilepsy (SCHOPE), to provide useful information to local
support groups and families of persons with epilepsy. Once our data analysis is
completed, preliminary results will be posted at the website.
4. Presentations—we have actively pursued dissemination of interim data through
scientific presentation both locally, nationally, and internationally. The following 12
presentations were made during the past three years.
1. Selassie AW. A multi-faceted epidemiological investigation of epilepsy and
seizure disorders in South Carolina: how big is the problem? South Carolina
Department of Health and Environmental Control epidemiology seminar,
Columbia, SC, November 5, 2004.
2. Ferguson PL. Smith GS. Selassie AW. Turner RP. Wannamaker B. Use of a
statewide administrative dataset to determine number of seizure and epilepsy
cases. American Epilepsy Society 58th Annual Meeting. New Orleans, LA,
December 7, 2004.
3. Selassie AW. Ferguson PL. Smith G. Pickelsimer EE. Wannamaker BW.
Turner RP. The frequency of epilepsy and seizure disorders among persons with
traumatic brain injury: a population-based evaluation of hospital discharges and
73
emergency department visits in South Carolina, 2996-2001. American Epilepsy
Society 58th Annual Meeting. New Orleans, LA, December 7, 2004.
4. Ferguson PL. Highlights of the first year findings (TBI & epilepsy among the
topics covered). CDC Ground Rounds. Atlanta, GA, April 14, 2005.
5. Ferguson PF. Selassie AW. South Carolina Epidemiological Studies of
Epilepsy and Seizure Disorder (SCESESD): 2002 - 2005. AAMC Grantee’s
Meeting. Atlanta, GA, March 16, 2005.
6. Wagner JL. Sample PL. Phillips L. Selassie AW. Psychosocial concerns in
pediatric epilepsy: a qualitative analysis. American Psychological Association
National Convention. Washington, DC, August 18, 2005.
7. Ferguson PL. Smith G. Selassie AW. Turner RP. Wannamaker BB. Tyrell M.
Pope A. Cavins KA. Topping KB. Use of seizure and epilepsy codes in
emergency department and inpatient discharges – South Carolina, USA. 26th
International Epilepsy Conference. Paris, France, August 28-September 1, 2005.
8. Pickelsimer EE. Sample PL. Ferguson PL. Selassie AW. Personal
perspectives of living with epilepsy or a seizure disorder. 26th International
Epilepsy Conference. Paris, France, August 28-September 1, 2005.
9. Ferguson PL. Smith GS. Selassie AW. Use of a statewide administrative
dataset to determine use of monotherapy vs polytherapy in epilepsy. American
Epilepsy Society 59th Annual Meeting. Washington, DC, December 2-6, 2005.
10. Ferguson PL. Special Interest Group presentation on Epidemiology: CDC
Epidemiologic Research Initiative. American Epilepsy Society 59th Annual
Meeting. Washington, DC, December 2-6, 2005.
11. Pickelsimer EE. Ferguson PL. Smith G. Selassie AW. Occurrence of
Epilepsy and Seizure Disorder in a Population Ages >15 Years Before and After
Hospitalization for Traumatic Brain Injury – a 3-year Follow-up Study. 7th
European Congress on Epileptology. Helsinki, Finland, July 2-6, 2006.
12. Ferguson PL. Selassie AW. South Carolina Epidemiological Studies of
Epilepsy and Seizure Disorder (SCESESD): 2002 - 2006. CDC Skill Building
Institute. Charleston, SC, May 17, 2006.
5. Manuscripts completed and in preparation—the project pursued manuscript
development since data became available in 2005. This activity will remain engaging
for the next couple of years to develop as many as 10-12 manuscripts. The following
is the list of manuscripts published and in preparation for submission.
74
1. Centers for Disease Control and Prevention. Prevalence of epilepsy and
health-related quality of life and disability among adults with epilepsy South Carolina, 2003 and 2004. MMWR 2005;54:1080-2.
2. Sample PL. Ferguson PF. Wagner JL. Pickelsimer EE. Selassie AW.
Experiences of persons with epilepsy and their families as they look for
medical and community care: A focus group study from South Carolina.
Epilepsy & Behavior. 2006;9:649-662.
3. Ferguson PL. Smith GM. Wannamaker BW. Thurman DJ. Pickelsimer
EE. Selassie AW. A population-based study of risk of epilepsy after
hospitalization for traumatic brain injury. Submitted to CDC for
clearance.
4. Wagner JL. Sample PL. Smith G. Pickelsimer EE. Ferguson PL. Selassie
AW. Impact of Pediatric Epilepsy: Voices from a Focus Group in South
Carolina. Written, final edits being done.
5. Ferguson PL. Chiprich J. Dong B. Thurman DJ. Wannamaker BW. Smith
GM. Prevalence of epilepsy and health care access among adults with
epilepsy in South Carolina: 2003-2005. Methods & analyses complete,
writing not yet complete.
6. Selassie AW. Ferguson PL. Smith GM. Lineberry L. Wannamaker BW.
Thurman DJ. Epilepsy and Seizure Disorders among persons with TBI: A
population-based Evaluation of Hospital Discharges and ED Visits in SC,
1997-2001. Analyses being revised, writing not complete at this time.
7. Ferguson PL. Smith GM. Wannamaker BW. Thurman DJ. Selassie AW.
Antiepileptic drug use in a population-based sample of individuals with
epilepsy. Most analyses complete, writing not started.
8. Selassie AW. Ferguson PL. Smith GM. Gu J. Wannamaker BW. Thurman
DJ. Predictive value positive and sensitivity of administrative data for
epilepsy and seizures. Most analyses complete, writing not started.
75
Appendices
76
Appendix A - Abstraction manual for inpatient and emergency department charts
SC Epidemiological Studies of Epilepsy & Seizure Disorders
Data Abstraction Manual
SECTION 1: RANDOM SAMPLE INFORMATION (Verbatim from Random
Sample)
1a.
Date of Abstraction (DATEABS)
Description:
Date on which record was abstracted.
Field Length: 8
Values:
Date record actually abstracted -- mm/dd/ccyy
1b.
Abstracter Initials (INITIALS)
Description:
Initials of data abstractor.
Field Length: 2
Values:
First and last name initials
1c.
Hospital ID Number (HID)
Random Sample Information
Description:
Number identifying the hospital in which the individual was treated.
Field Length: 3
Values:
A combination of numbers, which make up the hospital ID number
Note: may not be applicable if individual not seen in a hospital. Enter ‘999’ if NA.
1d.
Medical Record ID Number (MEDRECID)
Random Sample Information
Description:
A required, unique identification code.
Field length:
20
Values:
The actual number found on the abstraction list
Note: Please enter medical record number from the random sample list we send you.
Include dashes, letters, etc., and type exactly as the number appears on the
abstraction list. This is only the number to link the data you send to the original
file.
1e.
Type of medical visit (TYPEVIS)
Random Sample Information
Description:
Type of medical visit.
Field length:
1
Values:
1 = hospital inpatient
2 = emergency department
3 = outpatient, primary care provider (GP, family practice, internist,
pediatrician)
4 = outpatient, neurologist
5 = outpatient, epileptologist
6 = outpatient, other
9 = not STATED on abstraction list
77
1f.
Admittance or Outpatient Visit Date (ADMIT) Random Sample Information
Description:
Date when individual was admitted to the hospital, ED, or seen in
clinic/office.
Field length:
8
Values:
Date -- mm/dd/ccyy
Note: Enter 11/11/1111 if not found on the abstraction list. If admittance date differs on
the medical record, make a note of the different date in the comments section.
1g.
Discharge Date (DISD)
Random Sample Information
Description:
Date when individual was discharged from the hospital, if applicable.
Field length:
8
Values:
Date in -- mm/dd/ccyy
Note: Enter 11/11/1111 if not found on the abstraction list. If discharge date differs on
the medical record, make a note of the different date in the comments section.
1h.
Case ID Number (CASEID)
Random Sample Information
Description:
A required, unique identification code.
Field length:
8
Values:
The actual number found on the abstraction list.
Note: Please enter the Case ID Number from the random sample list we send you.
Please type exactly as provided.
1i.
Is Medical Record Available (RECAVAIL)
Description:
Determines whether the chart was available to be abstracted.
Field length:
1
Values:
1 = Yes
2 = No, clerk states (verbal or written) that record is being microfilmed/
microfiched or off-site storage
3 = No, clerk states (verbal or written) unable to locate but no reason
given
4 = No, clerk states (verbal or written) other reason
5 = No identifiable reason
Note: If answers 2 through 5, program skips to Missing Record Comments at end of
program. If Yes, program continues to next question.
SECTION 2: PERSONAL INFORMATION (From Here Forward from Medical
Chart)
2a.
Individual’s Last Name (LNAME)
Description:
The last name of the individual.
Field length:
40
Values:
Any valid name
Note: Enter 999 in first column if not STATED in medical record.
Note: If the name on the medical record is different than the name on the random
sample, enter the name from the medical record, including incorrect spelling.
Document in the comment section and flag the record.
78
2b.
Individual’s First Name (FNAME)
Description:
The last name of the individual.
Field length:
20
Values:
Any valid name
Note: Enter 999 in first column if not STATED in medical record.
2c.
Date of Birth (DOB)
Description:
Individual's date of birth.
Field Length: 8
Values:
mm/dd/ccyy
Note: Enter 11/11/1111 if not found in medical record.
2d.
Age (AGE)
Description:
Individual’s age
Field Length: 3
Values:
Age in years (acceptable range 0 to 120)
Note: Enter 999 if no age or DOB in medical record.
2e.
Sex (SEX)
Description:
Field Length:
Values:
The gender of the individual.
1
M= Male
F= Female
U= Unknown/Not STATED in medical record
2f.
Race (RACE)
Description:
The race or ethnicity of the individual.
Field Length: 1
Values:
1 = White
2 = Black
3 = Oriental / Asian
4 = American Indian
5 = Hispanic
6 = Native Hawaiian or other Pacific Islander
8 = Other
9 = Unknown/Not STATED in medical record
2g.
Marital Status (MARISTAT)
Description:
Current marital status of the individual.
Field length:
1
Values:
1 = Married (includes separated, stated common law marriages)
2 = Widowed
3 = Single (includes divorced)
5 = Minor child (<18, unless stated as married)
79
9 = Unknown/Not STATED in medical record
2h.
Individual’s Street Address (INDADDR)
Description:
The street address of residence of the individual.
Field length:
40
Values:
Any street address
Note: Be sure to get apartment and route numbers if applicable.
Note: Enter 999 in first column if not STATED in medical record.
2i.
Individual’s City (INDCITY)
Description:
The city of residence of the individual.
Field length:
20
Values:
Any city name
Note: Enter 999 in first column if not STATED in medical record.
2j.
Individual’s State (INDSTATE)
Description:
The state of residence of the individual.
Field length:
2
Values:
SC = South Carolina
NC = North Carolina
GA = Georgia
OT = Other
UK = Unknown/Not STATED in medical record
2k.
Individual’s Zip Code (INDZIP)
Description:
The zip code of residence of the individual.
Field length:
5
Values:
Five-digit number
Note: Enter 999 in first column if not STATED in medical record.
2l.
Telephone Number (PHONE)
Description:
Telephone number of the individual.
Field length:
13
Values:
A telephone number with area code as stated in the medical record.
Note: Enter (000) 000-0000 if the number is not STATED in medical record. If the area
is missing, enter (000) for area code and then the 7-digit number.
2m.
Employment Status (EMPSTAT)
Description:
Employment status of the individual.
Field length:
1
Values:
1 = Student
2 = Employed (full time or part time)
3 = Employed & attending school
4 = Retired
5 = Disabled
80
6 = Unemployed
7 = Minor Child under age 5
8 = None of the above
9 = Not STATED in medical record
2n.
Family Structure (FAMSTRU)
Description:
Family structure of individual
Field length:
2
Values:
1 = Lives alone
2 = Lives with spouse/significant other
3 = Lives with parent(s)
4 = Lives with relative other than parent
5 = Lives with foster parent
6 = Lives with hired caregiver
7 = Lives in rehabilitation facility
8 = Lives in nursing home
10 = Lives in state residential facility
11 = Lives in group home
12 = Lives in detention or corrections facility
13 = Other
9 = Not STATED in medical record
2o.
Insurance Status (INSSTA)
Description:
Insurance of individual
Field length:
1
Values:
1 = no medical insurance/self-pay
2 = Medicaid (includes Select Health, a SC Medicaid HMO)
3 = Medicare
4 = HMO
5 = Other private insurance
6 = Champus, TRI Care, or VA
9 = not STATED in medical record
SECTION 3: DIAGNOSIS & SEIZURE SPECIFICS
Enter ‘999’ in text fields if no information in medical record.
3a.
Chief Complaint (PREDIAG)
Description:
Chief complaint
Field length: 40
Values:
Medical reason for the visit or diagnosis
3b.
Discharge Diagnosis (POSTDIAG)
Description:
Discharge diagnosis
Field length:
40
Values:
MD’s discharge diagnosis
3c.
Primary Diagnosis Code/ICD-9 Code (DIAG1)
81
Description:
An ICD-9 CM code and rubric assigned to the diagnosis.
Field Length: 5
Values:
Code that the hospital, clinic, or office listed first.
Note: Decimal points are not entered. Enter 5 nine's (99999) if no code is found.
Note: Do not Add Zeros to any three digit N-Code found in the record.
3d-l.
Secondary ICD-9 Codes (DIAG2-DIAG10)
Description:
An ICD-9 CM code and rubric assigned to the diagnoses.
Field Length: 5 for each, for up to 9 codes
Values:
Any code listed in the medical record.
Note: Decimal points are not entered. Enter 5 nine's (99999) if no code is found.
Note: Do not Add Zeros to any three digit N-Code found in the record.
3m.
Discharge medication prescribed (MEDRX1)
Description:
Maintenance anti-epileptic medications prescribed this visit at discharge.
Field Length: Checklist of anti-epileptic medications
Values:
Check off medication if listed in medical record as discharge
medication.
3n.
Discharge medication prescribed (MEDRX2)
Description:
Maintenance anti-epileptic medication prescribed this visit at discharge.
Field Length: Checklist of anti-epileptic medications
Values:
Check off medication if listed in medical record as discharge
medication.
3o.
Discharge medication prescribed (MEDRX3)
Description:
Maintenance anti-epileptic medication prescribed this visit at discharge.
Field Length: Checklist of anti-epileptic medications
Values:
Check off medication if listed in medical record as discharge
medication.
3p.
Other discharge medication(s) prescribed (MEDRX4)
Description:
Maintenance anti-epileptic medication prescribed this visit at discharge.
Field Length: Checklist of anti-epileptic medications
Values:
Check off medication if listed in medical record as discharge
medication.
3q.
Seizure treatments prescribed other than medication (OTHTRT)
Description:
Other non-drug treatments prescribed to individual.
Field Length: 1
Values:
1 = Vagal nerve stimulator
2 = Neurosurgery
3 = Ketogenic diet
9 = not STATED in medical record
82
3r.
Seizure visit (SZVISIT)
Description:
Is this visit in reference to a current (day of visit or occurring since last
visit) seizure, possible seizure, seizure-like episode, or epilepsy?
Field Length: 1
Values:
1 = Purpose of visit related to a current seizure
2 = Initial visit not related to seizure, but seizure occurred during visit
3 = No current seizure, but visit related to seizure treatment, assessment,
etc.
(If 1, 2, or 3, rest of sections 3, 4, & 5 refer to this seizure or seizurelike episode)
4 = None of the above, visit not related to seizures (skip to 6a)
Following questions in this section and next 2 sections refer to the CURRENT seizure or
seizure-like episode.
3s.
Date of current seizure or seizure-like episode (SZDATE)
Description:
Date of recent seizure or seizure-like episode (may be date of visit or
date of most recent episode since last visit)
Field Length: 8
Values:
Any month, day, and year – mm/dd/ccyy
Note: may be estimated if not explicitly stated in record. If not STATED at all in record, put
11/11/1111
3t-v.
Narrative of current seizure or seizure-like episode (NTSEIZ)
Description:
Description of the current seizure and/or seizure-like episode (what
happened to patient before, during, and after this episode, or during
typical episode)
Field Length: 40 for each of three lines
Values:
Any description of the seizure episode(s). Please be as descriptive as
possible.
3w.
Seizure Type (SZTYPE1)
Description:
Clinical determination by MD of current seizure type(s), seizure
disorder, seizure-like episode, &/or epilepsy syndrome
Field Length: Checklist of seizure types
Values:
Check off seizure type if listed in medical record describing this episode,
or typical episode.
3x.
Seizure Type (SZTYPE2)
Description:
Clinical determination by MD of current seizure type(s), seizure
disorder, seizure-like episode, &/or epilepsy syndrome
Field Length: Checklist of seizure types
Values:
Check off seizure type if listed in medical record describing this episode,
or typical episode.
3y.
Seizure Type (SZTYPE3)
83
Description:
Field Length:
Values:
Clinical determination by MD of current seizure type(s), seizure
disorder, seizure-like episode, &/or epilepsy syndrome
Checklist of seizure types
Check off seizure type if listed in medical record describing this episode,
or typical episode.
3z.
Other seizure type(s) (SZTYPE4)
Description:
Other clinical determination by MD of current seizure type or seizurelike episode.
Field Length: 40
Values:
Any additional seizure type(s) or epilepsy not included on above lists
(refer to list provided in class)
3aa.
Number of seizures or seizure-like episodes (NUMSZ)
Description:
How many seizures or seizure-like episodes did the individual
experience during this episode?
Field Length: 1
Values:
1 = One seizure
2 = Two seizures
3 = More than two seizures
9 = Not STATED in medical record
3bb.
Time of seizure or seizure-like episode onset (SZTIME)
Description:
Time of onset of seizure or seizure-like episode (if cluster of seizures or
seizure-like episodes, use time of onset of cluster).
Field Length: 1
Values:
1 = Morning (7 am to 11:59 am)
2 = Afternoon (noon to 5:59 pm)
3 = Evening (6 pm to 9:59 pm)
4 = Nighttime (10 pm to 6:59 am)
9 = Not STATED in medical record
Note: May be estimated if approximate time mentioned in medical record.
3cc.
Length of seizure (LENGTH)
Description:
How long did the seizure or seizure-like episode last?
Field Length: 1
Values:
1 = 30 seconds or less
2 = >30 secs & up to 2 minutes
3 = > 2 minutes & up to 5 minutes
4 = More than 5 minutes
9 = Not STATED in medical record
3dd.
Seizure or seizure-like episode witness (SZOBS)
Description:
Who gave the details of the seizure or seizure-like episode?
Field Length: 1
84
Values:
1 = A health-care professional who directly witnessed the seizure or
episode
2 = A non-health care professional who directly witnessed the seizure or
episode
3 = Someone who spoke with an individual who directly witnessed the
seizure or episode
9 = Not STATED in medical record
3ee-gg. Emergent medication(s) given (MEDTRT1-3)
Description:
Medications given pre-hospital, or by ED, if applicable.
Field Length: Checklist of anti-epileptic medications
Values:
Check off medication if listed in medical record as given for seizure or
seizure-like episode.
SECTION 4: DETERMINATION OF SEIZURE TYPE
All questions in Section 4 refer to the current seizure or seizure-like episode.
4a.
Change in Mood before Seizure (ASMOOD)
Description:
Did the individual have a change in mood (i.e. quiet, agitated, scared)
PRIOR to this seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = not STATED in medical record
4b.
Restlessness before Seizure (ASREST)
Description:
Did the individual have restlessness PRIOR to this seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4c.
Bad taste in mouth (BADTST)
Description:
Did the individual experience a bad taste in mouth PRIOR to seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4d.
Smelling foul odor (BADSML)
Description:
Did the individual smell a foul odor PRIOR to seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
85
4e.
Seeing spots or flashing lights or colors in front of eyes (BADSEE)
Description:
Did the individual see spots or flashing lights or colors PRIOR to
seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4f.
Strange feeling in stomach (STOMACH)
Description:
Did the individual experience a strange feeling in stomach PRIOR to
seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4g.
Nausea (NAUSEA)
Description:
Did the individual experience nausea PRIOR to seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4h.
Headache (HEADACHE)
Description:
Did the individual experience a headache PRIOR to seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4i.
Weakness (WEAK)
Description:
Did the individual experience weakness PRIOR to seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4j.
Numbness (NUMB)
Description:
Did the individual experience numbness PRIOR to seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4k.
Tingling (TINGLE)
86
Description:
Did the individual experience tingling in hands, feet, arms, legs, or face
PRIOR to seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4l.
Crying out (CRYOUT)
Description:
Did the individual cry out PRIOR to seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4m.
Mumbling (MUMBLE)
Description:
Did the individual mumble PRIOR to seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4n.
Making sounds (MAKSNDS)
Description:
Did the individual make sounds but not real words PRIOR to seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4o.
Other aura (OTHAURA)
Description:
Did the individual have a feeling or sense that a seizure was about to
occur that cannot be described?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4p.
Start of seizure (START)
Description:
Did the seizure start suddenly, without any warning?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4q.
Fall (FALL)
Description:
Did the individual fall DURING the seizure?
87
Field Length:
Values:
4r.
Stiff (STIFF)
Description:
Field Length:
Values:
1
1 = Yes, fell forward
2 = Yes, fell backward
3 = No, did not fall (skip to 4t)
8 = Not applicable, since individual was sitting, lying down, etc. (skip to
4t)
9 = Not STATED in medical record (skip to 4t)
Did the individual go stiff and fall like a tree DURING the seizure?
1
1 = Yes
2 = No
9 = Not STATED in medical record
4s.
Limp (LIMP)
Description:
Did the individual go limp and fall over DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4t.
Blacked out (BLACKOUT)
Description:
Did the individual black out DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4u.
Pale Face (PALFACE)
Description:
Did the individual’s face color become pale DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4v.
Red face (REDFACE)
Description:
Did the individual’s face color flush, or become red, DURING the
seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4w.
Blue face (BLUFACE)
88
Description:
Field Length:
Values:
Did the individual’s face color become blue DURING the seizure?
1
1 = Yes
2 = No
9 = Not STATED in medical record
4x.
Tongue/lip/cheek biting (TONGUE)
Description:
Did the individual bite their tongue, lip or cheek DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4y.
Remembers seizure (MEMORY)
Description:
Does the individual remember what happened DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4z.
Hear during seizure (HEAR)
Description:
Was the individual able to hear DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4aa.
Incontinence (INCONT)
Description:
Did the individual lost control of bladder &/or bowels DURING
seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4bb.
Ability to talk (TALK)
Description:
Was the individual able to speak clearly DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4cc.
Affected side (SIDE)
Description:
What side of the body was affected DURING the seizure?
Field Length: 1
89
Values:
1 = Right side only
2 = Left side only
3 = Both sides
4 = No activity on either side
9 = Not STATED in medical record
4dd. Chewing motions (CHEW)
Description:
Did the individual exhibit chewing motions DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4ee.
Lip motions (LIP)
Description:
Did the individual exhibit lip-smacking DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4ff.
Face pulling (PULLING)
Description:
Did the individual’s face pull to one side DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4gg.
Facial trembling/shaking/twitching (FACE)
Description:
Did the individual’s face tremble, shake or twitch DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4hh.
Head turning (HEAD)
Description:
How did the individual’s head turn DURING the seizure?
Field Length: 1
Values:
1 = Head turned to the right
2 = Head turned to the left
3 = Head turned back and forth
4 = Head did not turn
9 = Not STATED in medical record
4ii.
Eye movement (EYEMOVE)
Description:
How did the individual’s eyes move DURING the seizure?
90
Field Length:
Values:
1
1 = Eyes pointed to the right
2 = Eyes pointed to the left
3 = Eyes rolled upward
4 = Eyes moved around randomly
5 = Eyes were straight ahead
6 = Eyes were closed
9 = Not STATED in medical record
4jj.
Hand movement (HANDS)
Description:
Did the individual’s hands pick at or fumble with clothes or objects
DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4kk.
Staring (STARE)
Description:
Did the individual exhibit a blank stare DURING the seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4ll.
Eyelid fluttering/blinking (EYELID)
Description:
Did the individual exhibit eyelid fluttering or blinking DURING the
seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4mm. Extremity stiffening (STIFFEN)
Description:
Did the individual exhibit stiffening (or spasms) of the arms &/or legs
DURING the seizure?
Field Length: 1
Values:
1 = Arms stiffened
2 = Legs stiffened
3 = Both arms & legs stiffened
4 = Neither arms nor legs stiffened
9 = Not STATED in medical record
4nn.
Extremity jerking (JERKING)
Description:
Did the individual exhibit jerking (or twitching) movements of the arms
&/or legs DURING the seizure?
91
Field Length:
Values:
1
1 = Arms had jerking movements
2 = Legs had jerking movements
3 = Both arms & legs had jerking movements
4 = Neither arms nor legs had jerking movements
9 = Not STATED in medical record
4oo.
Body trembling (TREMBLE)
Description:
Did the individual exhibit trembling (other than in face) DURING the
seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4pp.
Grunting (GRUNT)
Description:
Did the individual make grunting noises DURING the seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4qq.
Stopped breathing (NOBREATH)
Description:
Did the individual stop breathing DURING the seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4rr.
Noisy labored breathing (STERTOR)
Description:
Did the individual have noisy labored (stertorous) breathing DURING
the seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4ss.
Salivation, drooling, foaming (DROOL)
Description:
Did the individual have increased salivation, drooling, or foaming at the
mouth DURING the seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
92
4tt.
Heart racing (TACHY)
Description:
Did the individual have experience tachycardia, or a feeling of their
heart racing, DURING the seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4uu.
Panic feelings (PANIC)
Description:
Did the individual experience feelings of panic DURING the seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4vv.
Recovery after seizure (RECOVER)
Description:
Did the individual immediately recover after the seizure, and was able to
return to previous activities AFTER the seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4ww. Sleepy after seizure (SLEEPY)
Description:
Was the individual sleepy AFTER the seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4xx.
Restless after seizure (RESTLESS)
Description:
Was the individual agitated or restless AFTER the seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4yy.
Combative after seizure (COMBAT)
Description:
Was the individual combative AFTER the seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4zz.
Confused after seizure (CONFUSED)
93
Description:
Field Length
Values:
Was the individual confused AFTER the seizure?
1
1 = Yes
2 = No
9 = Not STATED in medical record
4aaa. Trouble speaking (TRBSPEAK)
Description:
Did the individual have trouble saying words (mumbling, nonsense
speech) AFTER the seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4bbb. Trouble finding word (TRBWORD)
Description:
Did the individual have trouble finding the right word to say AFTER the
seizure?
Field Length
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
SECTION 5: CAUSE OF SEIZURE
Enter ‘999’ in text fields if no information in medical record.
5a-c. Narrative of Cause of Seizure or seizure-like episode (CAUSE)
Description:
Brief description of current circumstances that might have contributed to
this seizure or seizure-like episode (what provoked this seizure?).
Field Length: 40 characters for each of three lines
Values:
Any narrative that describes a possible current cause of seizure or
seizure-like episode.
Note: Be as specific as possible.
5d.
Injury (INJURY)
Description:
Is there report that the individual’s seizure or seizure-like episode
occurred due to current injury?
Field Length: 1
Values:
1 = Yes, head injury
2 = Yes, injury other than to head
3 = Yes, injury to both head and elsewhere
4 = No (skip to 5f)
9 = Not STATED in medical record (skip to 5f)
5e.
Injury Incident Location Type (INJLOC)
Description:
Describes the type of place of occurrence of the current injury.
94
Field Length:
Values:
2
1 = Home
2 = Residential Institution
3 = School, other Institution and Public Administrative Area
4 = Sports or Recreation area
5 = Street or Highway
6 = Trade or Service Area
7 = Industrial or Construction Area
8 = Other Specified Place
9 = Unspecified Place or not STATED in medical record
10 = Farm
5f.
Illness prior to current seizure or seizure-like episode (ILLNESS)
Description:
Is there report that the individual is or has recently been ill?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
5g.
Fever prior to seizure or seizure-like episode (FEVER)
Description:
Is there report that the individual has had an elevated temperature?
Field Length: 1
Values:
1 = Yes, stated in record but no temperature recorded
2 = Yes, 99.6 to 101.5 F degrees (37.6 to 38.6 C)
3 = Yes, greater than 101.5 F degrees (> 38.6 C)
4 = No
9 = Not STATED in medical record
5h.
Sleep deprivation (SLEEP)
Description:
Is there report that the individual has experienced sleep deprivation
recently?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
5i.
Pregnancy (PREG)
Description:
Is the individual pregnant?
Field Length: 1
Values:
1 = Yes, record states female is pregnant
2 = Teen or adult female is not pregnant (skip to 5m)
9 = Not STATED in medical record (skip to 5m)
5j.
Eclampsia (ECLAMP)
95
Description:
Field Length:
Values:
Does the individual have eclampsia (or pre-eclampsia, pregnancyinduced hypertension, PIH, toxemia)?
1
1 = Yes
2 = No
9 = Not STATED in medical record
5k.
Alcohol use (ETOHUSE)
Description:
Is there report that the individual is presently using alcohol?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
5l.
Drug use (DRUGUSE)
Description:
Is there report that the individual is presently using illicit drugs?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
5m.
New Onset (NEWONSET)
Description:
Is this visit in regard to the patient’s first seizure or seizure-like episode?
Field Length: 1
Values:
1 = Yes (skip to 6aa)
2 = No (previous seizures noted, or history of seizures in medical
record)
9 = Not STATED in medical record
5n.
Medication change (MEDCHNG)
Description:
Is there report that the individual has recently changed anti-epileptic
medications?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
5o.
Weight gain in children (WTGAIN)
Description:
Is there report that the child has gained weight recently?
Field Length: 1
Values:
1 = Yes, pt aged 1-18 years has gained weight recently
2 = No, pt aged 1-18 years had not gained weight recently
8 = Not applicable (individual 18 years or older)
9 = Aged 1-18 years, but weight change not STATED in medical record
96
5p.
Use of personal protective equipment (EQUIP)
Description:
Is there report that the individual was using a prescribed helmet when
seizure occurred (this would be different from the usual bicycle helmet,
etc.)?
Field Length: 1
Values:
1 = Yes, individual was using prescribed helmet
2 = No, individual was not using prescribed helmet
9 = Not STATED in medical record
5q.
Noncompliance with medication (NONCOMP)
Description:
Is there report that the individual has recently not been compliant with
his/her seizure medication regimen?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
SECTION 6: MEDICAL HISTORY
Note: Enter “YES” if the record states previous history for the following.
Enter “NO” if the record states NO previous history for the following.
Enter “999” if no previous history information is documented in the medical record.
6a.
Previous seizure disorder or epilepsy diagnosis (PREVSEIZ)
Description:
Is there an earlier diagnosis, or some evidence of, seizure disorder or
epilepsy in the past?
Field Length: 1
Values:
1 = Yes (some evidence of previous seizures in chart)
2 = No (no mention of any previous seizures) (skip to 6aa)
9 = Not STATED in medical record (skip to 6aa)
6b.
Previous seizure type (PREVTYP1)
Description:
Previous clinical determination of type of seizure(s), seizure disorder(s),
or epilepsy?
Field Length: Checklist of seizure types
Values:
Check off seizure type if previous determination of seizure, seizure
disorder, or epilepsy
6c.
Previous seizure type (PREVTYP2)
Description:
Previous clinical determination of type of seizure(s), seizure disorder(s),
or epilepsy?
Field Length: Checklist of seizure types
Values:
Check off seizure type if previous determination of seizure, seizure
disorder, or epilepsy
6d.
Previous seizure type (PREVTYP3)
97
Description:
Field Length:
Values:
Previous clinical determination of type of seizure(s), seizure disorder(s),
or epilepsy?
Checklist of seizure types
Check off seizure type if previous determination of seizure, seizure
disorder, or epilepsy
6e.
Other previous seizure type(s) (PREVTYP4)
Description:
Other previous clinical determination of type of seizure(s), seizure
disorder(s), or epilepsy?
Field Length: 40
Values:
Any previous seizure type(s) not included on above lists (refer to list
provided in class)
6f-h.
Narrative of past seizure(s) (PREVNAR)
Description:
Description of past seizure(s) – what happens to patient before, during,
& after.
Field Length: 40 for each of 3 lines
Values:
Any description of previous seizure(s). Please be as descriptive as
possible.
6i.
Onset of seizure disorder/epilepsy (SZONSET)
Description:
Date of original onset of seizure disorder or epilepsy.
Field Length: 8
Values:
mm/dd/ccyy
Note: enter 11/11/1111 if not found in medical record. Can estimate date if an
approximate date is mentioned in medical record.
6j.
Date of Seizure (PREVDATE)
Description:
Date when individual had most recent seizure other than current
seizure or seizure-like episode.
Field Length: 8
Values:
Any month, day, and year -- mm/dd/ccyy
Note: Put 11/11/1111, if not STATED in medical record. May be estimated if
approximate date mentioned in medical record.
6k.
Multiple seizure types (MULTTYPE)
Description:
How many types of seizures has the individual experienced?
Field Length: 1
Values:
1 = One
2 = Two
3 = More than two
9 = Not STATED in medical record.
6l.
Frequency of seizures (FREQSEIZ)
Description:
How frequently does individual experience any seizure activity?
98
Field Length:
Values:
1
1 = Less than once a year
2 = More than once a year
3 = More than once a month
4 = More than once a week
5 = More than once a day
9 = Not STATED in medical record
6m.
Previous EEG (PREVEEG)
Description:
Has individual previously had an EEG?
Field Length: 1
Values:
1 = Yes, but no comment as to results in chart
2 = Yes, normal
3 = Yes, abnormal
9 = Not STATED in chart
6n.
Previous video EEG (PREVVEEG)
Description:
Has individual previously had a video EEG?
Field Length: 1
Values:
1 = Yes, but no comment as to results in chart
2 = Yes, normal
3 = Yes, abnormal
9 = Not STATED in chart
6o.
Previous CT scan of the head (PREVCT)
Description:
Has individual previously had a CT scan of the head?
Field Length: 1
Values:
1 = Yes, but no comment as to results in chart
2 = Yes, normal
3 = Yes, abnormal
9 = Not STATED in chart
6p.
Previous MRI of the head (PREVMRI)
Description:
Has individual previously had a MRI of the head?
Field Length: 1
Values:
1 = Yes, but no comment as to results in chart
2 = Yes, normal
3 = Yes, abnormal
9 = Not STATED in chart
6q.
Previous seizure treatments - medication (PREVMED)
Description:
Has individual been on anti-epileptic medication in past?
Field Length: 1
Values:
1 = Yes
2 = No
99
9 = Not STATED in medical record
6r.
Previous seizure treatments – neurosurgery (PREVSURG)
Description:
Has individual had neurosurgery for epilepsy (lobectomy, resection,
hemispherectomy, corpus callosotomy, subpial transection) in the past?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
6s.
Previous seizure treatments – vagal nerve stimulator (PREVVNS)
Description:
Has individual had a vagal nerve stimulator implanted for epilepsy in the
past?
Field Length:
Values:
1
1 = Yes
2 = No
9 = Not STATED in medical record
6t.
Previous seizure treatments – ketogenic diet (PREVKETO)
Description:
Has individual been on a ketogenic diet in the past for epilepsy?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
6u.
Previous seizure treatments – other (PREVOTH)
Description:
Has individual received some other treatment for epilepsy other than
medication, ketogenic diet, vagal nerve stimulator, or neurosurgery?
Field Length:
Values:
40
Description of other treatments, including alternative therapies.
6v.
Present medication (PRESMED1)
Description:
All present anti-epileptic medication.
Field Length: Checklist of anti-epileptic medications.
Values:
Check off medication patient taking at onset of visit.
6w.
Present medication (PRESMED2)
Description:
All present anti-epileptic medication.
Field Length: Checklist of anti-epileptic medications.
Values:
Check off medication patient taking at onset of visit
6x.
Present medication (PRESMED3)
Description:
All present anti-epileptic medication.
Field Length: Checklist of anti-epileptic medications.
100
Values:
6y.
Check off medication patient taking at onset of visit
Other present medication(s) (PRESMED4)
Description:
All present anti-epileptic medication.
Field Length: Checklist of anti-epileptic medications.
Values:
Check off medication patient taking at onset of visit
6z.
Previous medication noncompliance (PREVNONC)
Description:
Prior to this episode, does the individual have a history of epilepsy
medication noncompliance?
Field Length: 1
Values:
1 = Yes, skipping doses
2 = Yes, stopping medication
3 = Yes, but not specified
4 = No
9 = Not STATED in medical record
Note: If ‘1’ and ‘2’, choose ‘2’.
6aa.
Previous TBI (PREVTBI)
Description:
Does the patient’s medical history include a previous TBI?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
6bb.
Previous Alcohol Misuse (PREVALC)
Description: Prior to this episode, does the patient’s medical history include alcohol
misuse?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
6cc.
Previous Illicit Drug Use (PREVDRUG)
Description:
Prior to this episode, does the patient’s medical history include illicit
drug use?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
6dd.
Previous illness or injury (ETIOLOGY)
Description:
Any past illness, condition, or injury in the patient’s history that initially
caused the seizure disorder/epilepsy.
Field Length: 40
101
Values:
Previous illness,
seizures/epilepsy.
condition,
or
injury
that
initially
caused
6ee-hh.Co-morbidities (COMORBID)
Description:
Any other current medical &/or psychological conditions.
Field Length: 40 for each of 4 lines
Values:
List all other current medical conditions.
6ii.
Family history of seizures (FAMHX)
Description:
Family history of seizures, seizure disorders, or epilepsy.
Field Length: 1
Values:
1 = Yes
2 = No (skip to section 7)
9 = Not STATED in medical record (skip to section 7)
6jj.
Specifics of seizure family history (SPECFMHX)
Description:
What type of seizure, etc., is mentioned in family history?
Field Length: 40
Values:
Write whether family history of seizures, seizure disorder, or epilepsy,
and what type, as well as family member(s) with disorder.
SECTION 7: DIAGNOSTIC TESTS
A physician’s interpretation, such as in the H&P or notes, is preferable to determining results
from departmental print-out.
7a.
Anti-epileptic drug level 1 (AED1)
Description:
Blood drug level of an anti-epileptic drug and results
Field Length: 1
Values:
1 = Test ordered, no results/interpretation in chart
2 = Test done, and within therapeutic range
3 = Test done, and below therapeutic range
4 = Test done, and above therapeutic range
9 = Not STATED in medical record
7b.
Anti-epileptic drug level 2 (AED2)
Description:
Blood drug level of an anti-epileptic drug and results
Field Length: 1
Values:
1 = Test ordered, no results/interpretation in chart
2 = Test done, and within therapeutic range
3 = Test done, and below therapeutic range
4 = Test done, and above therapeutic range
9 = Not STATED in medical record
7c.
Blood Alcohol Level (BAL)
Description:
BAL and Results?
Field Length: 1
102
Values:
1 = Test ordered, no results/interpretation in chart
2 = BAL was done and value is 0-10 BAC in mg/dl (Negative)
3 = BAL was done and value is > 10 BAC in mg/dl
9 = Not STATED in medical record
7d.
Toxicology Screen (TOX)
Description:
Toxicology screen and Results?
Field Length: 1
Values:
1 = Test ordered, no results/interpretation in chart
2 = Toxicology screen was done and Negative
3 = Toxicology was done and At least one positive result
9 = Not STATED in medical record
7e.
CT Information (CT)
Description:
CT of the head and Results?
Field length:
1
Values:
1 = Test ordered, no results/interpretation in chart
2 = CT was taken and Normal
3 = CT was taken and Abnormal
9 = Not STATED in medical record
7f.
MRI Information (MRI)
Description:
MRI of the head and Results?
Field length:
1
Values:
1 = Test ordered, no results/interpretation in chart
2 = MRI was taken and Normal
3 = MRI was taken and Abnormal
9 = Not STATED in medical record
7g.
EEG Information (EEG)
Description:
EEG and Results?
Field length:
1
Values:
1 = Test ordered, no results/interpretation in chart
2 = EEG was taken and Normal
3 = EEG was taken and Abnormal
9 = Not STATED in medical record
7h.
Video EEG Information (VEEG)
Description:
Video EEG and Results?
Field length:
1
Values:
1 = Test ordered, no results/interpretation in chart
2 = EEG was taken and Normal
3 = EEG was taken and Abnormal
9 = Not STATED in medical record
103
7i.
EKG Information (EKG)
Description:
EKG and results?
Field length:
1
Values:
1 = Test ordered, no results/interpretation in chart
2 = EKG was taken and Normal
3 = EKG was taken and Abnormal
9 = Not STATED in medical record
7j.
Neurology consultation (NEUROCON)
Description:
Was the patient seen by a neurologist?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record.
7k.
Other consultation (OTHERCON)
Description:
Was the patient seen by some other specialist regarding their seizure or
seizure-like episode?
Field Length: 1
Values:
1 = Yes
2 = No (skip to section 8)
9 = Not STATED in medical record (skip to section 8)
7l.
Other consultation specifics (CONSPEC)
Description:
By what other type of specialist was the patient seen?
Field Length: 40
Values:
Specify what other specialist (list only specialties - if only name
available, leave empty).
SECTION 8: DISCHARGE DISPOSITION
8a.
Patient discharged to (DISCHTO)
Description:
Determines the type of facility the patient was discharged to.
Field length:
1
Values:
0 = Transferred to another acute care hospital
1 = Returned home, self-care
2 = Returned home, requiring non-skilled assistance (family member,
etc.)
3 = Returned home, requiring home health services and/or outpatient
rehabilitation
4 = Transferred to a residential facility without skilled nursing services
or with an unknown level of nursing care
5 = Transferred to a residential facility with skilled nursing services
6 = Transferred to an inpatient rehabilitation facility
7 = Died
10 = Left against medical advice (AMA)
104
11 = Correctional facility - includes prison, jail and detention centers
8 = Other
9 = Unknown/Not STATED in medical record
SECTION 9: REFERRALS
9a.
Primary Care Physician or pediatrician (PCMD)
Description:
Is a primary care physician listed (may include PCP, pediatrician,
internist, family health clinic, family practice physician, etc)?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
9b.
Primary care physician or pediatrician referral (REFPCMD)
Description:
Did the individual receive a referral to a primary care physician (see
above)?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
9c.
Neurologist (NEURO)
Description:
Is a neurologist listed?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
9d.
Neurologist referral (REFNEURO)
Description:
Did the individual receive a referral to a neurologist?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
9e.
Epileptologist (EPIL)
Description:
Is the individual currently under the care of an epileptologist/epilepsy
specialist?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
9f.
Epileptologist referral (REFEPIL)
105
Description:
Field Length:
Values:
Did the individual receive a referral to an epileptologist/epilepsy
specialist?
1
1 = Yes
2 = No
9 = Not STATED in medical record
9g.
Neurosurgical referral (REFNS)
Description:
Did the individual receive a referral to a neurosurgeon?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
9h.
Referral for EEG or VEEG tests (REFEEG)
Description:
Did the individual receive a referral for an EEG or VEEG?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
9i.
Referral for an MRI (REFMRI)
Description:
Did the individual receive a referral for an MRI?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
9j.
Referral to an Epilepsy Center (REFEC)
Description:
Did the individual receive a referral to an epilepsy center?
Field length:
1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
SECTION 10: CLOSING
10a.
Abstractor Comments (COMMENTS)
Description:
Does the abstractor have any comments about this record?
Field length:
1
Values:
1 = Yes
2 = No (skip to 10g)
10b-c. Abstracter Administrative Comments (COMMENT1-2)
Description:
Informative remarks made by the data abstracter to add additional
insight to this particular patient record.
106
Field Length:
Values:
40 for each of 2 lines
Any narrative (administrative problems – random sample info different
from chart, chart difficult to read, etc.)
10d-f. Abstractor Clinical Comments (COMMENT3-5)
Description:
Informative remarks made by the data abstracter to add additional
insight to this particular patient record.
Field Length: 40 for each of 3 lines
Values:
Any narrative (clinically-related problems – need to add something extra
for which there was no entry place, note that question mark written in
text was copied from chart, note that question mark written in text due to
illegible chart, etc.)
10g.
Flagged for Special Review (FLAG)
Description:
Does this record need to be flagged for special review?
Field length:
1
Values:
1 = Yes
2 = No
Note: A record would need to be reviewed by another abstractor if there is
contradictory information in the chart (ex. a pregnant male), information in
medical record not matching random sample or other problems.
Note: Reason(s) for flag should be recorded in Abstractor Comments.
107
Appendix B - Abstraction manual for physician office visit charts
SC Epidemiological Studies of Epilepsy & Seizure Disorders
Data Abstraction Manual for Physician Office Visits
SECTION 1: RANDOM SAMPLE INFORMATION (Verbatim from Random
Sample)
1a.
Date of Abstraction (DATEABS)
Description:
Date on which record was abstracted.
Field Length: 8
Values:
Date record actually abstracted -- mm/dd/ccyy
1b.
Abstracter Initials (INITIALS)
Description:
Initials of data abstractor.
Field Length: 2
Values:
First and last name initials
1c.
Physician ID Number (PID)
Random Sample Information
Description:
Number identifying the individual’s physician.
Field Length: 3
Values:
A combination of numbers, which make up the physician ID number
Note: may not be applicable if individual not seen in a hospital. Enter ‘999’ if NA.
1d.
Medical Record ID Number (MEDRECID)
Random Sample Information
Description:
A required, unique identification code.
Field length:
20
Values:
The actual number found on the abstraction list
Note: Please enter medical record number from the random sample list we send you.
Include dashes, letters, etc., and type exactly as the number appears on the
abstraction list. This is only the number to link the data you send to the original
file.
1e.
Type of physician (TYPEMD)
Random Sample Information
Description:
Specialty of physician or other provider (ie, nurse practitioner).
Field length:
1
Values:
1 = primary care (ie, GP, family practice, internal medicine, pediatrics)
2 = neurology
3 = epileptology
4 = obstetrics and/or gynecology
5 = other
9 = not STATED on abstraction list
1f.
Outpatient Visit Date (ADMIT)
Random Sample Information
Description:
Date when individual was seen by physician.
108
Field length:
8
Values:
Date -- mm/dd/ccyy
Note: Enter 11/11/1111 if not found on the abstraction list. If date differs on the
medical record, make a note of the different date in the comments section.
1g.
Case ID Number (CASEID)
Random Sample Information
Description:
A required, unique identification code.
Field length:
8
Values:
The actual number found on the abstraction list.
Note: Please enter the Case ID Number from the random sample list we send you.
Please type exactly as provided.
1h.
ICD-9-CM code, most recent (ICD9ORS)
Random Sample Information
Description:
Seizure-related code provided in random sample.
Field length:
1
Values:
0 = 345.0
1 = 345.1
2 = 345.2
3 = 345.3
4 = 345.4
5 = 345.5
6 = 345.6
7 = 345.7
8 = 345.8
9 = 345.9
10 = 780.31
11 = 780.39
12 = 780.3
1i.
Is Medical Record Available (RECAVAIL)
Description:
Determines whether the chart was available to be abstracted.
Field length:
1
Values:
1 = Yes
2 = No, clerk states (verbal or written) that record is being microfilmed/
microfiched or off-site storage
3 = No, clerk states (verbal or written) unable to locate but no reason
given
4 = No, clerk states (verbal or written) other reason
5 = No identifiable reason
Note: If answers 2 through 5, program skips to Missing Record Comments at end of
program. If Yes, program continues to next question.
SECTION 2: PERSONAL INFORMATION (From Here Forward from Medical
Chart)
2a.
Individual’s Last Name (LNAME)
109
Description:
The last name of the individual.
Field length:
40
Values:
Any valid name
Note: Enter 999 in first column if not STATED in medical record.
Note: If the name on the medical record is different than the name on the random
sample, enter the name from the medical record, including incorrect spelling.
Document in the comment section and flag the record.
2b.
Individual’s First Name (FNAME)
Description:
The last name of the individual.
Field length:
20
Values:
Any valid name
Note: Enter 999 in first column if not STATED in medical record.
2c.
Date of Birth (DOB)
Description:
Individual's date of birth.
Field Length: 8
Values:
mm/dd/ccyy
Note: Enter 11/11/1111 if not found in medical record.
2d.
Age (AGE)
Description:
Individual’s age at time of most recent visit
Field Length: 3
Values:
Age in years (acceptable range 0 to 120)
Note: Enter 999 if no age or DOB in medical record.
2e.
Sex (SEX)
Description:
Field Length:
Values:
2f.
The gender of the individual.
1
M= Male
F= Female
U= Unknown/Not STATED in medical record
Race (RACE)
Description:
The race or ethnicity of the individual.
Field Length: 1
Values:
1 = White
2 = Black
3 = Oriental / Asian
4 = American Indian
5 = Hispanic
6 = Native Hawaiian or other Pacific Islander
8 = Other
9 = Unknown/Not STATED in medical record
110
2g.
Marital Status (MARISTAT)
Description:
Current marital status of the individual.
Field length:
1
Values:
1 = Married (includes separated, stated common law marriages)
2 = Widowed
3 = Single (includes divorced)
5 = Minor child (<18, unless stated as married)
9 = Unknown/Not STATED in medical record
2h.
Individual’s Street Address (INDADDR)
Description:
The street address of residence of the individual.
Field length:
40
Values:
Any street address
Note: Be sure to get apartment and route numbers if applicable.
Note: Enter 999 in first column if not STATED in medical record.
2i.
Individual’s City (INDCITY)
Description:
The city of residence of the individual.
Field length:
20
Values:
Any city name
Note: Enter 999 in first column if not STATED in medical record.
2j.
Individual’s State (INDSTATE)
Description:
The state of residence of the individual.
Field length:
2
Values:
SC = South Carolina
NC = North Carolina
GA = Georgia
OT = Other
UK = Unknown/Not STATED in medical record
2k.
Individual’s Zip Code (INDZIP)
Description:
The zip code of residence of the individual.
Field length:
5
Values:
Five-digit number
Note: Enter 999 in first column if not STATED in medical record.
2l.
Employment Status (EMPSTAT)
Description:
Employment status of the individual.
Field length:
1
Values:
1 = Student
2 = Employed (full time or part time)
3 = Employed & attending school
4 = Retired
5 = Disabled
111
6 = Unemployed
7 = Minor Child under age 5
8 = None of the above
9 = Not STATED in medical record
2m.
Family Structure (FAMSTRU)
Description: Family structure of individual
Field length:
2
Values:
1 = Lives alone
2 = Lives with spouse/significant other
3 = Lives with parent(s)
4 = Lives with relative other than parent
5 = Lives with foster parent
6 = Lives with hired caregiver
7 = Lives in rehabilitation facility
8 = Lives in nursing home
10 = Lives in state residential facility
11 = Lives in group home
12 = Lives in detention or corrections facility
13 = Other
9 = Not STATED in medical record
2n.
Insurance Status (INSSTA)
Description:
Insurance of individual
Field length:
1
Values:
1 = no medical insurance/self-pay
2 = Medicaid (includes Select Health, a SC Medicaid HMO)
3 = Medicare
4 = HMO
5 = Other private insurance
6 = Champus, TRI Care, or VA
9 = not STATED in medical record
SECTION 3: DIAGNOSIS & SEIZURE SPECIFICS
Enter ‘999’ in text fields if no information in medical record.
3a.
Date of most current seizure (SZDATE)
Description:
Date of most recent seizure (in relation to Outpatient Visit Date from
random sample information)
Field Length: 1
Values:
0 = prior to 2001
1 = 2001
2 = 2002
9 = not STATED in medical record
3b-g. Narrative of most current seizure (NTSEIZ)
112
Description:
Field Length:
Values:
possible.
Description of the most current seizure(s) (what happened to patient
before, during, and after this episode, or during typical episode)
40 for each of three lines
Any description of the seizure episode(s). Please be as descriptive as
3h.
Multiple seizure types (MULTTYPE)
Description:
How many types of seizures has the individual experienced?
Field Length: 1
Values:
1 = One
2 = Two
3 = More than two
9 = Not STATED in medical record.
3i.
Seizure Type (SZTYPE1)
Description:
Clinical determination by MD of most current seizure type(s), seizure
disorder, &/or epilepsy syndrome
Field Length: Checklist of seizure types
Values:
Check off seizure type if listed in medical record describing this episode,
or typical episode.
3j.
Seizure Type (SZTYPE2)
Description:
Clinical determination by MD of most current seizure type(s), seizure
disorder, &/or epilepsy syndrome
Field Length: Checklist of seizure types
Values:
Check off seizure type if listed in medical record describing this episode,
or typical episode.
3k.
Seizure Type (SZTYPE3)
Description:
Clinical determination by MD of most current seizure type(s), seizure
disorder, &/or epilepsy syndrome
Field Length: Checklist of seizure types
Values:
Check off seizure type if listed in medical record describing this episode,
or typical episode.
3l.
Other seizure type(s) (SZTYPE4)
Description:
Other clinical determination by MD of current seizure type.
Field Length: 40
Values:
Any additional seizure type(s) or epilepsy not included on above lists
(refer to list provided in class)
3m.
Number of seizures (NUMSZ)
Description:
How many seizures did the individual experience during most recent
episode of seizures?
Field Length: 1
113
Values:
1 = One seizure
2 = Two seizures
3 = More than two seizures
9 = Not STATED in medical record
3n.
Time of seizure onset (SZTIME)
Description:
Time of onset of most recent seizure (if cluster of seizures use time of
onset of cluster).
Field Length: 1
Values:
1 = Morning (7 am to 11:59 am)
2 = Afternoon (noon to 5:59 pm)
3 = Evening (6 pm to 9:59 pm)
4 = Nighttime (10 pm to 6:59 am)
9 = Not STATED in medical record
Note: May be estimated if approximate time mentioned in medical record.
3o.
Length of seizure (LENGTH)
Description:
How long did the most recent seizure last?
Field Length: 1
Values:
1 = 30 seconds or less
2 = >30 secs & up to 2 minutes
3 = > 2 minutes & up to 5 minutes
4 = More than 5 minutes
9 = Not STATED in medical record
SECTION 4: CAUSE OF SEIZURE
Enter ‘999’ in text fields if no information in medical record.
4a-c. Narrative of Cause of most recent Seizure (CAUSE)
Description:
Brief description of recent circumstances that might have contributed to
the most recent seizure (ie, what provoked this seizure?).
Field Length: 40 characters for each of three lines
Values:
Any narrative that describes a possible current cause of seizure
Note: Be as specific as possible.
4d.
Injury (INJURY)
Description:
Is there report that the individual’s most recent seizure occurred due to a
recent injury?
Field Length: 1
Values:
1 = Yes, head injury
2 = Yes, injury other than to head
3 = Yes, injury to both head and elsewhere
4 = No
9 = Not STATED in medical record
4e.
Illness prior to most recent seizure (ILLNESS)
114
Description:
Field Length:
Values:
Is there report that the individual was ill prior to their most recent
seizure?
1
1 = Yes
2 = No
9 = Not STATED in medical record
4f.
Fever prior to most recent seizure (FEVER)
Description:
Is there report that the individual had an elevated temperature prior to
their most recent seizure?
Field Length: 1
Values:
1 = Yes, stated in record but no temperature recorded
2 = Yes, 99.6 to 101.5 F degrees (37.6 to 38.6 C)
3 = Yes, greater than 101.5 F degrees (> 38.6 C)
4 = No
9 = Not STATED in medical record
4g.
Sleep deprivation (SLEEP)
Description:
Is there report that the individual experienced sleep deprivation prior to
their more recent seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4h.
Pregnancy (PREG)
Description:
Was the individual pregnant during their most recent seizure?
Field Length: 1
Values:
1 = Yes, record states female was pregnant
2 = Teen or adult female was not pregnant (skip to 4j)
9 = Not STATED in medical record (skip to 4j)
4i.
Eclampsia (ECLAMP)
Description:
Did the individual have eclampsia (or pre-eclampsia, pregnancy-induced
hypertension, PIH, toxemia)?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4j.
Alcohol use (ETOHUSE)
Description:
Is there report that the individual was using alcohol prior to the most
recent seizure?
Field Length: 1
Values:
1 = Yes
115
2 = No
9 = Not STATED in medical record
4k.
Drug use (DRUGUSE)
Description:
Is there report that the individual was using illicit drugs prior to the most
recent seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4l.
First seizure (SZFIRST)
Description:
Is the most recent seizure the individual’s first seizure?
Field Length: 1
Values:
1 = Yes (skip to 5l)
2 = No
9 = Not STATED in medical record
4m.
Medication change (MEDCHNG)
Description:
Is there report that the individual had recently changed anti-epileptic
medications before their most recent seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
4n.
Weight gain in children (WTGAIN)
Description:
Is there report that the child had gained weight recently prior to their
most recent seizure?
Field Length: 1
Values:
1 = Yes, pt aged 1-18 years had gained weight recently
2 = No, pt aged 1-18 years had not gained weight recently
8 = Not applicable (individual 18 years or older)
9 = Aged 1-18 years, but weight change not STATED in medical record
4o.
Noncompliance with medication (NONCOMP)
Description:
Is there report that the individual had recently not been compliant with
his/her seizure medication regimen prior to the most recent seizure?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
SECTION 5: MEDICAL HISTORY
Note: Enter “YES” if the record states previous history for the following.
116
5a.
Enter “NO” if the record states NO previous history for the following.
Enter “999” if no previous history information is documented in the medical record.
Onset of seizure disorder/epilepsy (SZONSET)
Description:
Year of original onset of seizure disorder or epilepsy.
Field Length: 4
Values:
ccyy
Note: enter 1111 if not found in medical record. Can estimate date if an approximate
date is mentioned in medical record.
5b.
Frequency of seizures (FREQSEIZ)
Description:
In the year prior to the most recent visit (Outpatient Visit Date from
random sample information) how many times did the individual
experience any seizure activity?
Field Length: 1
Values
1 = None in previous year
2 = 1-3 times
3 = 4-11 times
4 = 12-24 times, or once a month
5 = 25-51 times
6 = 52-104 times, or once a week
7 = 104-364 times
8 = 365 times or more, or once a day or more
9 = Not STATED in medical record
5c.
Seizure treatments – neurosurgery (PREVSURG)
Description:
Has individual had neurosurgery for epilepsy (lobectomy, resection,
hemispherectomy, corpus callosotomy, subpial transection?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
5d.
Seizure treatments – vagal nerve stimulator (PREVVNS)
Description:
Has individual had a vagal nerve stimulator implanted for epilepsy?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
5e.
Seizure treatments – ketogenic diet (PREVKETO)
Description:
Has individual been on a ketogenic diet for epilepsy?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
117
5f.
Medication (PRESMED1)
Description:
Any anti-epileptic medication at most recent visit (Outpatient Visit Date
from random sample information).
Field Length: Checklist of anti-epileptic medications.
Values:
Check off medication patient taking at onset of visit.
5g.
Medication (PRESMED2)
Description:
Any anti-epileptic medication at most recent visit (Outpatient Visit Date
from random sample information).
Field Length: Checklist of anti-epileptic medications.
Values:
Check off medication patient taking at onset of visit
5h.
Medication (PRESMED3)
Description:
Any anti-epileptic medication at most recent visit (Outpatient Visit Date
from random sample information).
Field Length: Checklist of anti-epileptic medications.
Values:
Check off medication patient taking at onset of visit
5i.
Medication (PRESMED4)
Description:
Any anti-epileptic medication at most recent visit (Outpatient Visit Date
from random sample information).
Field Length: Checklist of anti-epileptic medications.
Values:
Check off medication patient taking at onset of visit
5j.
Previous medication (PREVMED)
Description:
If individual not on anti-epileptic medication at most recent visit, has
individual ever been on anti-epileptic medication?
Field Length: 1
Values:
1 = Yes, took anti-epileptic medication in the past
2 = No evidence in chart that individual has ever taken anti-epileptic
medication (skip to 5l)
3 = N/A, individual taking anti-epileptic medication at most recent visit
9 = Not STATED in medical record
5k.
History of medication noncompliance (PREVNONC)
Description:
Does the individual have a history
noncompliance?
Field Length: 1
Values:
1 = Yes, skipping doses
2 = Yes, stopping medication
3 = Yes, but not specified
4 = No
9 = Not STATED in medical record
Note: If ‘1’ and ‘2’, choose ‘2’.
118
of
epilepsy
medication
5l.
History of TBI (PREVTBI)
Description:
Does the patient’s medical history include a TBI?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
5m.
History of Alcohol Misuse (PREVALC)
Description:
Does the patient’s medical history include alcohol misuse?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
5n.
History of Illicit Drug Use (PREVDRUG)
Description:
Does the patient’s medical history include illicit drug use?
Field Length: 1
Values:
1 = Yes
2 = No
9 = Not STATED in medical record
5o.
Previous illness or injury (ETIOLOGY)
Description:
Any past illness, condition, or injury in the patient’s history that initially
caused the seizure disorder/epilepsy. If there is mention of any of the
following terms, please make note under ‘etiology’: CRYPTOGENIC,
IDIOPATHIC, FAMILIAL, SYMPTOMATIC, REFLEX, PRIMARY,
or SECONDARY.
Field Length: 40
Values:
Previous illness, condition, or injury that initially caused
seizures/epilepsy.
5p-s. Co-morbidities (COMORBID)
Description:
Any other medical &/or psychological conditions at most recent visit
(Outpatient Visit Date from random sample information).
Field Length: 40 for each of 4 lines
Values:
List all other current medical conditions.
5t.
Family history of seizures (FAMHX)
Description:
Family history of seizures, seizure disorders, or epilepsy.
Field Length: 1
Values:
1 = Yes
2 = No (skip to section 6)
9 = Not STATED in medical record (skip to section 6)
119
5u.
Specifics of seizure family history (SPECFMHX)
Description:
What type of seizure, etc., is mentioned in family history?
Field Length: 40
Values:
Write whether family history of seizures, seizure disorder, or epilepsy,
and what type, as well as family member(s) with disorder.
SECTION 6: DIAGNOSTIC TESTS
A physician’s interpretation, such as in the H&P or notes, is preferable to determining results
from departmental print-out.
6a.
EEG (PREVEEG)
Description:
Has individual had an EEG?
Field Length: 1
Values:
1 = Yes, but no comment as to results in chart
2 = Yes, normal
3 = Yes, abnormal
9 = Not in medical record
6b.
Video EEG (PREVVEEG)
Description:
Has individual had a video EEG?
Field Length: 1
Values:
1 = Yes, but no comment as to results in chart
2 = Yes, normal
3 = Yes, abnormal
9 = Not STATED in medical record
6c.
CT scan of the head (PREVCT)
Description:
Has individual had a CT scan of the head?
Field Length: 1
Values:
1 = Yes, but no comment as to results in chart
2 = Yes, normal
3 = Yes, abnormal
9 = Not STATED in medical record
6d.
MRI of the head (PREVMRI)
Description:
Has individual had a MRI of the head?
Field Length: 1
Values:
1 = Yes, but no comment as to results in chart
2 = Yes, normal
3 = Yes, abnormal
9 = Not STATED in medical record
6e.
Anti-epileptic drug level 1 (AED1)
Description:
Most recent blood drug level of an anti-epileptic drug and results
Field Length: 1
Values:
1 = Test ordered, no results/interpretation in chart
120
2 = Test done, and within therapeutic range
3 = Test done, and below therapeutic range
4 = Test done, and above therapeutic range
9 = Not STATED in medical record
6f.
Anti-epileptic drug level 2 (AED2)
Description:
Most recent blood drug level of a second anti-epileptic drug and results
Field Length: 1
Values:
1 = Test ordered, no results/interpretation in chart
2 = Test done, and within therapeutic range
3 = Test done, and below therapeutic range
4 = Test done, and above therapeutic range
9 = Not STATED in medical record
SECTION 7 CLOSING
7a.
Abstractor Comments (COMMENTS)
Description:
Does the abstractor have any comments about this record?
Field length:
1
Values:
1 = Yes
2 = No (skip to7g)
7b-c. Abstracter Administrative Comments (COMMENT1-2)
Description:
Informative remarks made by the data abstracter to add additional
insight to this particular patient record.
Field Length: 40 for each of 2 lines
Values:
Any narrative (administrative problems – random sample info different
from chart, chart difficult to read, etc.)
7d-f.
Abstractor Clinical Comments (COMMENT3-5)
Description:
Informative remarks made by the data abstracter to add additional
insight to this particular patient record.
Field Length: 40 for each of 3 lines
Values:
Any narrative (clinically-related problems – need to add something extra
for which there was no entry place, note that question mark written in
text was copied from chart, note that question mark written in text due to
illegible chart, etc.)
7g.
Flagged for Special Review (FLAG)
Description:
Does this record need to be flagged for special review?
Field length:
1
Values:
1 = Yes
2 = No
Note: A record would need to be reviewed by another abstractor if there is
contradictory information in the chart (ex. a pregnant male), information in
medical record not matching random sample or other problems.
Note: Reason(s) for flag should be recorded in Abstractor Comments.
121
Appendix C - Comparison of inpatient/ED sample to population
Using population database from ORS, with sampled cases marked, and using abstracted values of
sex, age group, payer, and diagnosis for sample group (using race assigned by ORS for sample
since more complete).
‘ABS’ = ABSTRACTED CASES (IE, SAMPLE); ‘POP’ = WHOLE POPULATION OF CASES WITH SEIZURE-RELATED DIAGNOSES
‘CNT’ = COUNT; ‘PCNT’ = PERCENT; ‘LL’ = LOWER 95% CI; ‘UL’ = UPPER 95% CI
IF >1 DIAGNOSIS, POP. DIAGNOSIS ASSIGNED ACCORDING TO FOLLOWING HIERARCHY: 345.X > 780.3 > 780.2> 293.0.
2001, 345.X (n=765, n=1731)
SEX_ABS_
SEX_ABS_
SEX
CNT
PCNT
F
388
50.72
M
377
49.28
RACE_
ABS_CNT
315
12
438
RACE
BLACK
OTH/UNK
WHITE
PAYER
INSURANCE
MEDICAID
MEDICARE
NOT STATED
UNINSURED
AGEGRP
0-9
10-19
20-29
30-39
40-49
50-59
60-69
70-79
80-89
90+
RACE_
ABS_PCNT
41.18
1.57
57.25
PAYER_
ABS_CNT
196
210
260
3
96
AGEGRP_
ABS_CNT
88
49
87
125
125
109
93
56
30
3
AGEGRP_
ABS_PCNT
11.50
6.41
11.37
16.34
16.34
14.25
12.16
7.32
3.92
0.39
RACE_
ABS_CNT
819
26
920
RACE_
ABS_PCNT
46.40
1.47
52.12
SEX_
ABS_UL
57.26
55.91
RACE_
ABS_LL
34.03
0.00
51.17
PAYER_
ABS_PCNT
25.62
27.45
33.99
0.39
12.55
2001, 7803 (n=1765, N=18,685)
SEX_ABS_
SEX_ABS_
SEX
CNT
PCNT
F
839
47.54
M
926
52.46
U
.
.
RACE
BLACK
OTH/UNK
WHITE
SEX_
ABS_LL
44.18
42.65
RACE_
ABS_UL
48.32
10.81
63.34
PAYER_
ABS_LL
17.59
19.52
26.42
0.00
3.84
AGEGRP_
ABS_LL
2.74
0.00
2.61
7.82
7.82
5.62
3.43
0.00
0.00
0.00
SEX_
ABS_LL
43.09
48.24
.
RACE_
ABS_LL
41.91
0.00
47.88
SEX_POP_
CNT
862
869
RACE_
POP_CNT
734
33
964
PAYER_
ABS_UL
33.65
35.38
41.55
9.69
21.26
AGEGRP_
ABS_UL
20.26
15.41
20.14
24.86
24.86
22.87
20.89
16.29
13.05
9.69
SEX_
ABS_UL
51.98
56.69
.
RACE_
ABS_UL
50.89
7.56
56.37
SEX_POP_
PCNT
49.80
50.20
SEX_POP_
CNT
8935
9749
1
RACE_
POP_CNT
8004
356
10325
122
RACE_
POP_PCNT
42.40
1.91
55.69
PAYER_
POP_CNT
451
467
571
5
237
AGEGRP_
POP_CNT
209
142
192
266
306
236
175
134
61
10
SEX_
POP_LL
45.41
45.83
RACE_
POP_LL
37.70
0.00
51.57
PAYER_
POP_PCNT
26.05
26.98
32.99
0.29
13.69
AGEGRP_
POP_PCNT
12.07
8.20
11.09
15.37
17.68
13.63
10.11
7.74
3.52
0.58
SEX_POP_
PCNT
47.82
52.18
0.01
RACE_
POP_PCNT
42.84
1.91
55.26
SEX_
POP_UL
54.18
54.57
RACE_
POP_UL
47.10
8.04
59.81
PAYER_
POP_LL
20.73
21.69
27.92
0.00
7.94
AGEGRP_
POP_LL
6.27
2.27
5.25
9.67
12.06
7.88
4.24
1.79
0.00
0.00
SEX_
POP_LL
46.46
50.87
0.00
RACE_
POP_LL
41.41
0.04
54.00
PAYER_
POP_UL
31.38
32.27
38.05
6.47
19.44
AGEGRP_
POP_UL
17.88
14.14
16.93
21.06
23.29
19.39
15.98
13.69
9.61
6.75
SEX_
POP_UL
49.18
53.48
1.89
RACE_
POP_UL
44.26
3.77
56.52
PAYER
INSURANCE
MEDICAID
MEDICARE
NOT STATED
UNINSURED
AGEGRP
0-9
10-19
20-29
30-39
40-49
50-59
60-69
70-79
80-89
90+
PAYER_
ABS_CNT
404
397
704
7
253
AGEGRP_
ABS_CNT
207
113
161
215
275
253
194
210
115
22
PAYER_
ABS_PCNT
22.89
22.49
39.89
0.40
14.33
AGEGRP_
ABS_PCNT
11.73
6.40
9.12
12.18
15.58
14.33
10.99
11.90
6.52
1.25
2002, 345X (n=427, N=1656)
SEX_ABS_
SEX_ABS_
SEX
CNT
PCNT
F
220
51.52
M
207
48.48
RACE_
ABS_CNT
197
10
220
RACE
BLACK
OTH/UNK
WHITE
PAYER
INSURANCE
MEDICAID
MEDICARE
NOT STATED
UNINSURED
AGEGRP
0-9
10-19
20-29
30-39
40-49
50-59
60-69
70-79
80-89
90+
RACE_
ABS_PCNT
46.14
2.34
51.52
PAYER_
ABS_CNT
117
147
117
.
46
AGEGRP_
ABS_CNT
62
46
49
69
68
63
30
29
10
1
AGEGRP_
ABS_LL
5.97
0.47
3.28
6.44
9.95
8.66
5.21
6.14
0.59
0.00
SEX_
ABS_LL
42.84
39.53
RACE_
ABS_LL
36.99
0.00
42.84
PAYER_
ABS_PCNT
27.40
34.43
27.40
.
10.77
AGEGRP_
ABS_PCNT
14.52
10.77
11.48
16.16
15.93
14.75
7.03
6.79
2.34
0.23
PAYER_
ABS_LL
17.51
17.10
35.13
0.00
8.66
AGEGRP_
ABS_UL
17.49
12.33
14.97
17.93
21.21
20.01
16.78
17.65
12.44
7.34
SEX_
ABS_UL
60.20
57.43
PAYER_
POP_CNT
4548
4284
6936
91
2826
AGEGRP_
POP_CNT
2303
1259
1764
2303
3086
2683
1960
1903
1187
237
SEX_POP_
CNT
834
822
RACE_
ABS_UL
55.28
14.66
60.20
PAYER_
ABS_LL
16.78
24.33
16.78
.
0.00
AGEGRP_
ABS_LL
3.00
0.00
0.00
4.75
4.50
3.25
0.00
0.00
0.00
0.00
PAYER_
ABS_UL
28.27
27.89
44.64
6.52
20.01
AGEGRP_
POP_PCNT
12.33
6.74
9.44
12.33
16.52
14.36
10.49
10.18
6.35
1.27
SEX_POP_
PCNT
50.36
49.64
RACE_
POP_CNT
679
35
942
PAYER_
ABS_UL
38.02
44.52
38.02
.
22.55
AGEGRP_
ABS_UL
26.04
22.55
23.20
27.57
27.35
26.26
19.05
18.83
14.66
12.68
123
PAYER_
POP_CNT
460
489
489
1
217
AGEGRP_
POP_CNT
226
157
216
243
265
233
138
125
42
11
PAYER_
POP_PCNT
24.34
22.93
37.12
0.49
15.12
AGEGRP_
POP_LL
10.56
4.92
7.65
10.56
14.79
12.62
8.71
8.40
4.53
0.00
SEX_
POP_LL
45.90
45.15
RACE_
POP_PCNT
41.00
2.11
56.88
PAYER_
POP_PCNT
27.78
29.53
29.53
0.06
13.10
AGEGRP_
POP_PCNT
13.65
9.48
13.04
14.67
16.00
14.07
8.33
7.55
2.54
0.66
PAYER_
POP_LL
22.70
21.27
35.63
0.00
13.39
RACE_
POP_LL
36.14
0.00
52.73
AGEGRP_
POP_UL
14.09
8.56
11.23
14.09
18.24
16.10
12.27
11.97
8.18
3.14
SEX_
POP_UL
54.82
54.13
RACE_
POP_UL
45.86
8.38
61.04
PAYER_
POP_LL
22.40
24.22
24.22
0.00
7.20
AGEGRP_
POP_LL
7.77
3.46
7.14
8.83
10.20
8.20
2.27
1.46
0.00
0.00
PAYER_
POP_UL
25.98
24.58
38.61
2.37
16.86
PAYER_
POP_UL
33.16
34.84
34.84
6.39
19.00
AGEGRP_
POP_UL
19.53
15.50
18.95
20.52
21.80
19.94
14.39
13.63
8.79
6.97
2002, 7803 (n=1026, N=19,511)
SEX_ABS_
SEX_ABS_
SEX
CNT
PCNT
F
463
45.13
M
563
54.87
RACE
BLACK
OTH/UNK
WHITE
RACE_
ABS_CNT
476
18
532
PAYER
INSURANCE
MEDICAID
MEDICARE
NOT STATED
UNINSURED 174
AGEGRP
0-9
10-19
20-29
30-39
40-49
50-59
60-69
70-79
80-89
90+
RACE_
ABS_PCNT
46.39
1.75
51.85
SEX_
ABS_LL
39.17
49.47
RACE_
ABS_LL
40.51
0.00
46.27
PAYER_
PAYER_
ABS_CNT
ABS_PCNT
186
18.13
248
24.17
411
40.06
7
0.68
16.96
9.63
AGEGRP_
ABS_CNT
90
57
113
131
190
160
111
92
70
12
AGEGRP_
ABS_PCNT
8.77
5.56
11.01
12.77
18.52
15.59
10.82
8.97
6.82
1.17
SEX_
ABS_UL
51.08
60.28
RACE_
ABS_UL
52.28
9.73
57.43
PAYER_
ABS_LL
10.85
17.17
33.83
0.00
24.29
AGEGRP_
ABS_LL
1.09
0.00
3.43
5.26
11.26
8.21
3.22
1.29
0.00
0.00
SEX_POP_
CNT
9261
10250
RACE_
POP_CNT
8198
381
10932
SEX_POP_
PCNT
47.47
52.53
RACE_
POP_PCNT
42.02
1.95
56.03
SEX_
POP_LL
46.13
51.26
RACE_
POP_LL
40.61
0.13
54.81
PAYER_
PAYER_
PAYER_
ABS_UL
POP_CNT
POP_PCNT
25.40
4505
23.09
31.17
4772
24.46
46.28
7208
36.94
8.70
123
0.63
2903
14.88
13.18
AGEGRP_
ABS_UL
16.45
13.37
18.60
20.28
25.78
22.98
18.41
16.64
14.59
9.16
124
AGEGRP_
POP_CNT
2464
1287
1797
2439
3295
2803
2048
1903
1220
255
AGEGRP_
POP_PCNT
12.63
6.60
9.21
12.50
16.89
14.37
10.50
9.75
6.25
1.31
SEX_
POP_UL
48.80
53.80
RACE_
POP_UL
43.42
3.78
57.25
PAYER_
POP_LL
21.47
22.86
35.48
0.00
16.58
AGEGRP_
POP_LL
10.91
4.81
7.45
10.78
15.21
12.66
8.75
8.00
4.47
0.00
PAYER_
POP_UL
24.71
26.06
38.41
2.47
AGEGRP_
POP_UL
14.35
8.38
10.97
14.23
18.57
16.07
12.24
11.51
8.04
3.14
Appendix D - Comparison of physician office visit sample to population
Using population database from ORS, combining years and payer groups, with sampled cases
marked, and using population values of sex, age group, payer, and diagnosis for both sample and
population group.
345X (n=174, N=1157)
SEX
F
M
SEX_ABS_
CNT
89
85
RACE
BLACK
OTH/UNK
WHITE
PAYER
COMM-SHP
M/CAID
M/CARE
SEX_ABS_
PCNT
51.15
48.85
RACE_
ABS_CNT
44
55
75
RACE_
ABS_PCNT
25.29
31.61
43.10
PAYER_
ABS_CNT
48
67
59
AGEGRP_
ABS_CNT
37
6
13
31
32
27
12
13
3
AGEGRP
10-19
2-9
20-29
30-39
40-49
50-59
60-69
70-79
80+
SEX_ABS_
CNT
34
38
RACE
BLACK
OTH/UNK
WHITE
PAYER
COMM-SHP
M/CAID
M/CARE
RACE_
ABS_LL
8.41
15.46
28.37
PAYER_
ABS_PCNT
27.59
38.51
33.91
AGEGRP_
ABS_PCNT
21.26
3.45
7.47
17.82
18.39
15.52
6.90
7.47
1.72
7803 (n=72, N=2096)
SEX
F
M
SEX_
ABS_LL
37.50
34.88
SEX_ABS_
PCNT
47.22
52.78
RACE_
ABS_CNT
7
31
34
PAYER_
ABS_CNT
31
23
18
PAYER_
ABS_LL
10.97
23.19
18.03
AGEGRP_
ABS_LL
3.94
0.00
0.00
0.11
0.75
0.00
0.00
0.00
0.00
SEX_
ABS_LL
25.17
31.92
RACE_
ABS_PCNT
9.72
43.06
47.22
PAYER_
ABS_PCNT
43.06
31.94
25.00
RACE_
ABS_LL
0.00
20.15
25.17
PAYER_
ABS_LL
20.15
6.90
0.00
SEX_
ABS_UL
64.80
62.82
SEX_POP_
CNT
587
570
RACE_
ABS_UL
42.17
47.76
57.83
RACE_
POP_CNT
238
476
443
SEX_POP_
PCNT
50.73
49.27
RACE_
POP_PCNT
20.57
41.14
38.29
SEX_
POP_LL
45.42
43.87
SEX_
POP_UL
56.05
54.66
RACE_
POP_LL
13.82
35.33
32.34
RACE_
POP_UL
27.32
46.95
44.24
PAYER_
ABS_UL
44.20
53.82
49.78
PAYER_
POP_CNT
409
528
220
PAYER_
POP_PCNT
35.35
45.64
19.01
PAYER_
POP_LL
29.26
40.05
12.20
AGEGRP_
ABS_UL
38.59
22.64
26.25
35.52
36.03
33.47
25.74
26.25
21.08
AGEGRP_
POP_CNT
232
86
159
174
185
163
87
47
24
AGEGRP_
POP_PCNT
20.05
7.43
13.74
15.04
15.99
14.09
7.52
4.06
2.07
AGEGRP_
POP_LL
13.28
0.15
6.71
8.06
9.05
7.07
0.24
0.00
0.00
SEX_
ABS_UL
69.28
73.64
SEX_POP_
CNT
1060
1036
RACE_
ABS_UL
38.57
65.96
69.28
RACE_
POP_CNT
606
715
775
PAYER_
ABS_UL
65.96
56.99
51.29
125
PAYER_
POP_CNT
611
1151
334
SEX_POP_
PCNT
50.57
49.43
RACE_
POP_PCNT
28.91
34.11
36.98
PAYER_
POP_PCNT
29.15
54.91
15.94
SEX_
POP_LL
46.62
45.43
RACE_
POP_LL
24.17
29.55
32.51
PAYER_
POP_LL
24.42
51.14
10.78
PAYER_
POP_UL
41.44
51.22
25.83
AGEGRP_
POP_UL
26.82
14.72
20.78
22.02
22.93
21.11
14.80
11.48
9.57
SEX_
POP_UL
54.53
53.43
RACE_
POP_UL
33.66
38.68
41.44
PAYER_
POP_UL
33.89
58.69
21.09
AGEGRP
2-9
10-19
20-29
30-39
40-49
50-59
60-69
70-79
80+
AGEGRP_
ABS_CNT
.
5
6
15
14
11
12
8
1
AGEGRP_
ABS_PCNT
.
6.94
8.33
20.83
19.44
15.28
16.67
11.11
1.39
AGEGRP_
ABS_LL
.
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
AGEGRP_
ABS_UL
.
36.23
37.40
47.84
46.69
43.22
44.38
39.73
31.53
126
AGEGRP_
POP_CNT
155
244
258
314
351
339
233
123
79
AGEGRP_
POP_PCNT
7.40
11.64
12.31
14.98
16.75
16.17
11.12
5.87
3.77
AGEGRP_
POP_LL
1.98
6.35
7.04
9.79
11.61
11.02
5.81
0.41
0.00
AGEGRP_
POP_UL
12.81
16.93
17.58
20.17
21.88
21.32
16.42
11.33
9.29
Appendix E. Likelihood of an epilepsy diagnosis conditional on satisfying the model parameters (n=Random Sample 87 records)
Obs
id1
agegp
racegp
comorbgp
VISIT
dxgp
payer
beta0
beta11
beta12
beta13
beta14
beta15
beta16
38 955337687
10-19
BLACK
1)hi-risk
2-5
345X
MEDICAID
-1.0658
1.9364
0.0000
0.0000
0.0000
0.0000
0
207 959037307
10-19
WHITE
1)hi-risk
2-5
7803
MEDICAID
-1.0658
1.9364
0.0000
0.0000
0.0000
0.0000
0
678 955780301
20-39
WHITE
1)hi-risk
2-5
345X
MEDICARE
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
1478 950281255
0-9
WHITE
1)hi-risk
1
345X
MEDICAID
-1.0658
0.0000
0.0000
0.0000
0.0000
0.0000
0
2323 959696611
10-19
WHITE
2)lo-risk
1
7802+
MEDICAID
-1.0658
1.9364
0.0000
0.0000
0.0000
0.0000
0
2877 955165719
10-19
BLACK
2)lo-risk
1
7803
MEDICAID
-1.0658
1.9364
0.0000
0.0000
0.0000
0.0000
0
3462 959343277
60-79
BLACK
1)hi-risk
2-5
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
3944 955331223
10-19
BLACK
2)lo-risk
1
7802+
MEDICARE
-1.0658
1.9364
0.0000
0.0000
0.0000
0.0000
0
5495 955387868
60-79
BLACK
2)lo-risk
2-5
7803
MEDICAID
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
6085 959979595
20-39
BLACK
2)lo-risk
2-5
7803
MEDICAID
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
7885 959298518
10-19
BLACK
2)lo-risk
1
7803
INSURANCE
-1.0658
1.9364
0.0000
0.0000
0.0000
0.0000
0
9761 955829918
20-39
WHITE
2)lo-risk
1
345X
INSURANCE
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
11066 950358501
20-39
BLACK
2)lo-risk
1
7802+
MEDICAID
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
11527 955739597
40-59
BLACK
2)lo-risk
1
7802+
MEDICAID
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
11587 955861570
20-39
BLACK
2)lo-risk
1
7802+
MEDICAID
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
12246 955868655
10-19
WHITE
2)lo-risk
1
7803
INSURANCE
-1.0658
1.9364
0.0000
0.0000
0.0000
0.0000
0
14522 959548081
20-39
WHITE
1)hi-risk
1
7803
MEDICAID
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
14964 954090312
60-79
BLACK
2)lo-risk
2-5
7803
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
15886 959043134
40-59
BLACK
2)lo-risk
2-5
7803
MEDICARE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
16890 950895712
20-39
WHITE
2)lo-risk
1
7802+
MEDICAID
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
17260 955901033
20-39
WHITE
2)lo-risk
1
7802+
MEDICAID
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
17531 959560662
40-59
WHITE
2)lo-risk
1
7802+
MEDICAID
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
17647 950781243
40-59
WHITE
1)hi-risk
1
7802+
INSURANCE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
18596 959678822
60-79
WHITE
1)hi-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
18823 955235671
10-19
WHITE
2)lo-risk
1
7803
UNINSURED
-1.0658
1.9364
0.0000
0.0000
0.0000
0.0000
0
19011 955879589
40-59
BLACK
2)lo-risk
1
7803
MEDICAID
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
127
Appendix E. Likelihood of an epilepsy diagnosis conditional on satisfying the model parameters (n=Random Sample 87 records)
Obs
id1
agegp
racegp
comorbgp
VISIT
dxgp
payer
beta0
beta11
beta12
beta13
beta14
beta15
beta16
20199 955668458
40-59
BLACK
2)lo-risk
1
7803
MEDICAID
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
20669 959190026
40-59
BLACK
2)lo-risk
1
7803
MEDICAID
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
21256 952417855
60-79
WHITE
2)lo-risk
2-5
7803
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
23700 959634019
40-59
WHITE
2)lo-risk
2-5
7803
MEDICARE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
24169 950222829
40-59
BLACK
1)hi-risk
1
7803
INSURANCE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
25195 955715653
40-59
BLACK
2)lo-risk
2-5
7803
UNINSURED
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
26980 954290003
40-59
BLACK
2)lo-risk
1
7802+
INSURANCE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
27630 954863693
40-59
BLACK
2)lo-risk
1
7802+
INSURANCE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
28218 955302959
40-59
BLACK
2)lo-risk
1
7802+
INSURANCE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
29065 955897618
80-89
BLACK
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
0.0000
1.9839
0
29884 959378017
40-59
BLACK
2)lo-risk
1
7802+
INSURANCE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
32917 954426231
60-79
WHITE
1)hi-risk
1
7803
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
33715 959825560
60-79
WHITE
1)hi-risk
1
7803
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
34359 959975360
20-39
WHITE
2)lo-risk
2-5
7803
UNINSURED
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
35955 952252831
60-79
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
36432 952468497
80-89
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
0.0000
1.9839
0
36745 952638795
80-89
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
0.0000
1.9839
0
37754 954012591
60-79
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
39099 954226089
80-89
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
0.0000
1.9839
0
39856 954266263
60-79
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
40258 954332524
20-39
WHITE
2)lo-risk
1
7802+
INSURANCE
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
40459 954403152
60-79
WHITE
2)lo-risk
1
7802+
INSURANCE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
40498 954407233
80-89
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
0.0000
1.9839
0
40552 954413177
60-79
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
41808 954552065
80-89
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
0.0000
1.9839
0
42155 954591313
60-79
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
128
Appendix E. Likelihood of an epilepsy diagnosis conditional on satisfying the model parameters (n=Random Sample 87 records)
Obs
id1
agegp
racegp
comorbgp
VISIT
dxgp
payer
beta0
beta11
beta12
beta13
beta14
beta15
beta16
44838 955751246
80-89
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
0.0000
1.9839
0
45064 955874494
60-79
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
46455 959147161
40-59
WHITE
2)lo-risk
1
7802+
INSURANCE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
47165 959418311
40-59
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
47202 959439666
80-89
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
0.0000
1.9839
0
47661 959676433
60-79
WHITE
2)lo-risk
1
7802+
INSURANCE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
48159 959747803
80-89
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
0.0000
1.9839
0
48216 959753596
60-79
WHITE
2)lo-risk
1
7802+
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
50337 954261897
40-59
BLACK
2)lo-risk
1
7802+
UNINSURED
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
50342 954267565
20-39
BLACK
2)lo-risk
1
7802+
UNINSURED
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
52030 952947189
40-59
BLACK
2)lo-risk
1
7803
INSURANCE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
52041 954006697
40-59
BLACK
2)lo-risk
1
7803
INSURANCE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
53490 955750418
60-79
BLACK
2)lo-risk
1
7803
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
53595 955817050
60-79
BLACK
2)lo-risk
1
7803
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
53772 955927239
0-9
BLACK
2)lo-risk
1
7803
INSURANCE
-1.0658
0.0000
0.0000
0.0000
0.0000
0.0000
0
54153 959195727
40-59
BLACK
2)lo-risk
1
7803
MEDICARE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
54723 959660436
40-59
BLACK
2)lo-risk
1
7803
MEDICARE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
54764 959694110
60-79
BLACK
2)lo-risk
1
7803
MEDICARE
-1.0658
0.0000
0.0000
0.0000
1.8278
0.0000
0
54956 959903570
40-59
BLACK
2)lo-risk
1
7803
MEDICARE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
55628 950344027
20-39
WHITE
2)lo-risk
1
7802+
UNINSURED
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
55687 950697662
20-39
WHITE
2)lo-risk
1
7802+
UNINSURED
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
57018 956111353
40-59
WHITE
2)lo-risk
1
7802+
UNINSURED
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
57911 955563903
20-39
WHITE
2)lo-risk
1
7803
INSURANCE
-1.0658
0.0000
2.3996
0.0000
0.0000
0.0000
0
59907 954251015
40-59
WHITE
2)lo-risk
1
7803
INSURANCE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
60328 954432776
40-59
WHITE
2)lo-risk
1
7803
MEDICARE
-1.0658
0.0000
0.0000
2.1972
0.0000
0.0000
0
129
Obs
beta21
beta22
beta31
beta41
beta42 beta51
beta52
beta61 beta62 beta63
logits
probit
probit2
epilepgp3
38
0.4394
0.0000 0.8274
1.2732
0 0.0000
0.0000 0.9143
0.000 0.0000
4.3249
0.98694
98.69 1)Probable
207
0.0000
0.0000 0.8274
1.2732
0 0.0000
0.6168 0.9143
0.000 0.0000
3.2687
0.96334
96.33 1)Probable
678
0.0000
0.0000 0.8274
1.2732
0 1.5276
0.0000 0.0000
0.883 0.0000
2.5624
0.92840
92.84 1)Probable
1478
0.0000
0.0000 0.8274
0.0000
0 1.5276
0.0000 0.9143
0.000 0.0000
2.2035
0.90056
90.06 1)Probable
2323
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.9143
0.000 0.0000
1.7849
0.85630
85.63 1)Probable
2877
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.9143
0.000 0.0000
1.6075
0.83306
83.31 1)Probable
3462
0.4394
0.0000 0.8274
1.2732
0 0.0000
0.0000 0.0000
0.883 0.0000
1.4742
0.81369
81.37 1)Probable
3944
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
1.3100
0.78751
78.75 1)Probable
5495
0.4394
0.0000 0.0000
1.2732
0 0.0000
0.6168 0.9143
0.000 0.0000
0.9443
0.71997
72.00 1)Probable
6085
0.4394
0.0000 0.0000
1.2732
0 0.0000
0.6168 0.9143
0.000 0.0000
0.9443
0.71997
72.00 1)Probable
7885
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.000 0.0000
0.6932
0.66668
66.67 1)Probable
9761
0.0000
0.0000 0.0000
0.0000
0 1.5276
0.0000 0.0000
0.000 0.0000
0.4618
0.61344
61.34 1)Probable
11066
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.9143
0.000 0.0000
0.2879
0.57148
57.15 1)Probable
11527
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.9143
0.000 0.0000
0.2879
0.57148
57.15 1)Probable
11587
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.9143
0.000 0.0000
0.2879
0.57148
57.15 1)Probable
12246
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.000 0.0000
0.2538
0.56311
56.31 1)Probable
14522
0.0000
0.0000 0.8274
0.0000
0 0.0000
0.6168 0.9143
0.000 0.0000
0.0591
0.51477
51.48 1)Probable
14964
0.4394
0.0000 0.0000
1.2732
0 0.0000
0.6168 0.0000
0.883 0.0000
0.0300
0.50750
50.75 1)Probable
15886
0.4394
0.0000 0.0000
1.2732
0 0.0000
0.6168 0.0000
0.883 0.0000
0.0300
0.50750
50.75 1)Probable
16890
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.9143
0.000 0.0000
-0.1515
0.46220
46.22 1)Probable
17260
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.9143
0.000 0.0000
-0.1515
0.46220
46.22 1)Probable
17531
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.9143
0.000 0.0000
-0.1515
0.46220
46.22 1)Probable
17647
0.0000
0.0000 0.8274
0.0000
0 0.0000
0.0000 0.0000
0.000 0.0000
-0.2384
0.44068
44.07 1)Probable
18596
0.0000
0.0000 0.8274
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-0.2384
0.44068
44.07 1)Probable
18823
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.000 0.5422
-0.2884
0.42840
42.84 1)Probable
19011
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.9143
0.000 0.0000
-0.3289
0.41851
41.85 1)Probable
20199
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.9143
0.000 0.0000
-0.3289
0.41851
41.85 1)Probable
20669
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.9143
0.000 0.0000
-0.3289
0.41851
41.85 1)Probable
130
Obs
beta21
beta22
beta31
beta41
beta42 beta51
beta52
beta61 beta62 beta63
logits
probit
probit2
epilepgp3
21256
0.0000
0.0000 0.0000
1.2732
0 0.0000
0.6168 0.0000
0.883 0.0000
-0.4094
0.39906
39.91 2)Possible
23700
0.0000
0.0000 0.0000
1.2732
0 0.0000
0.6168 0.0000
0.883 0.0000
-0.4094
0.39906
39.91 2)Possible
24169
0.4394
0.0000 0.8274
0.0000
0 0.0000
0.6168 0.0000
0.000 0.0000
-0.4158
0.39752
39.75 2)Possible
25195
0.4394
0.0000 0.0000
1.2732
0 0.0000
0.6168 0.0000
0.000 0.5422
-0.5122
0.37468
37.47 2)Possible
26980
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.0000
-0.6264
0.34833
34.83 2)Possible
27630
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.0000
-0.6264
0.34833
34.83 2)Possible
28218
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.0000
-0.6264
0.34833
34.83 2)Possible
29065
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-0.6264
0.34833
34.83 2)Possible
29884
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.0000
-0.6264
0.34833
34.83 2)Possible
32917
0.0000
0.0000 0.8274
0.0000
0 0.0000
0.6168 0.0000
0.883 0.0000
-0.8552
0.29834
29.83 3)Unlikely
33715
0.0000
0.0000 0.8274
0.0000
0 0.0000
0.6168 0.0000
0.883 0.0000
-0.8552
0.29834
29.83 3)Unlikely
34359
0.0000
0.0000 0.0000
1.2732
0 0.0000
0.6168 0.0000
0.000 0.5422
-0.9516
0.27856
27.86 3)Unlikely
35955
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
36432
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
36745
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
37754
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
39099
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
39856
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
40258
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.0000
-1.0658
0.25620
25.62 3)Unlikely
40459
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.0000
-1.0658
0.25620
25.62 3)Unlikely
40498
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
40552
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
41808
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
42155
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
44838
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
45064
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
46455
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.0000
-1.0658
0.25620
25.62 3)Unlikely
47165
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
131
Obs
beta21
beta22
beta31
beta41
beta42 beta51
beta52
beta61 beta62 beta63
logits
probit
probit2
epilepgp3
47202
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
47661
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.0000
-1.0658
0.25620
25.62 3)Unlikely
48159
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
48216
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.883 0.0000
-1.0658
0.25620
25.62 3)Unlikely
50337
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.5422
-1.1686
0.23711
23.71 3)Unlikely
50342
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.5422
-1.1686
0.23711
23.71 3)Unlikely
52030
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.000 0.0000
-1.2432
0.22388
22.39 3)Unlikely
52041
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.000 0.0000
-1.2432
0.22388
22.39 3)Unlikely
53490
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.883 0.0000
-1.2432
0.22388
22.39 3)Unlikely
53595
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.883 0.0000
-1.2432
0.22388
22.39 3)Unlikely
53772
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.000 0.0000
-1.2432
0.22388
22.39 3)Unlikely
54153
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.883 0.0000
-1.2432
0.22388
22.39 3)Unlikely
54723
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.883 0.0000
-1.2432
0.22388
22.39 3)Unlikely
54764
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.883 0.0000
-1.2432
0.22388
22.39 3)Unlikely
54956
0.4394
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.883 0.0000
-1.2432
0.22388
22.39 3)Unlikely
55628
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.5422
-1.6080
0.16687
16.69 3)Unlikely
55687
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.5422
-1.6080
0.16687
16.69 3)Unlikely
57018
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.0000 0.0000
0.000 0.5422
-1.6080
0.16687
16.69 3)Unlikely
57911
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.000 0.0000
-1.6826
0.15675
15.68 3)Unlikely
59907
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.000 0.0000
-1.6826
0.15675
15.68 3)Unlikely
60328
0.0000
0.0000 0.0000
0.0000
0 0.0000
0.6168 0.0000
0.883 0.0000
-1.6826
0.15675
15.68 3)Unlikely
132
Appendix F - Posttraumatic epilepsy incidence analysis
SCTBIFR: Overall risk of developing posttraumatic epilepsy (PTE) within 3 years of discharge after TBI.
Original cohort = 2118 persons. 12 individuals removed who did not answer epilepsy-related questions.
Also removed 145 cases with pre-existing epilepsy. Analysis cohort = 1961 persons.
Note: there were 208 individuals who were inadvertently not asked epilepsy-related question in year 2 or 3. 35 of the individuals not
asked in year 2 did not participate in year 3, and 2 individuals were not asked the epilepsy-related questions in year 3.
Years of interview participation (with years adjusted to whether asked epilepsy-related questions on 2nd and/or 3rd interviews) for
those 1846 without any epilepsy:
Cumulative
Cumulative
YEAR
Frequency
Percent
Frequency
Percent
ƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒ
FIRST
556
30.12
556
30.12
Participated only in 1st year
SECON
280
15.17
836
45.29
Participated in 1st & 2nd years
THIRD
1010
54.71
1846
100.00
Participated all 3 years
Year of onset of 115 cases with PTE:
Cumulative
ONSET
Frequency
Percent
Frequency Crude rates
ƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒ
YEAR 1
43
37.39
43
43/1961 = 2.2% of those at risk developed PTE in 1st year
YEAR 2
44
38.26
87
44/1362 = 3.2% of those at risk developed PTE in 2nd year
YEAR 3
28
24.35
115
28/1038 = 2.7% of those at risk developed PTE in 3rd year
IF UNSURE OF YEAR OF ONSET, TOOK LATER YEAR TO BE CONSERVATIVE (INCLUDE MAX YEARS AT RISK).
How years were adjusted for missing years of questions:
Last year of interview participation of cases not developing epilepsy:
Cumulative
Cumulative
YEAR
Frequency
Percent
Frequency
Percent
ƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒƒ
FIRST
521
28.22
521
28.22
SECON
313
16.96
834
45.18
THIRD
1012
54.82
1846
100.00
Remaining cases interviewed each year (include those w/o posttraumatic epilepsy at start of year, so ‘at risk’):
Y1 = 1961
Y2 = 1012 + 313 + 28 + 44 =1397
Y3 = 1012 + 28 =1040
But:
35 individuals without epilepsy were not asked ESD questions in year 2, and did not participate in year 3.
2 individuals without epilepsy were not asked ESD questions in year 3.
133
So, adjusting for above,
Individuals interviewed concerning new PTE each year (person-years at risk):
Y1 =
1961
Y2 = 1397 – 35 = 1362
Y3 = 1040 – 2 = 1038
4361
Crude incidence rate over these 3 years (or incidence density):
115 with PTE/4361 person-yrs = 0.0264 person-yrs, or average of 2.6 cases per 100 person-years, or average of 2.6 cases per 100
people over a 1 year period.
Using exponential formula:
Year Δt # new cases Person-yrs ID(1/yr)
approx. R [= 1 – exp(-ID*Δt)]
1
1
43
1961
.02193
.02169
2
1
44
1362
.03231
.03179
3
1
28
1038
.02697
.02661
3 year risk = 1 – exp(-Σ ID * Δt) = .07697 = 7.7 cases per 100 people over a 3 year period.
The above formula is the exponential formula for relating rates and incidence proportions (Morgenstern H, Kleinbaum DG, Kupper
LL. Measures of disease incidence used in epidemiologic research. International Journal of Epidemiology. 9(1):97-104;1980.) (Also
see Rothman & Greenland, Modern Epidemiology, 2nd edition, 1998). However, it is subject to 3 assumptions:
1. the population is closed;
2. the event under study is inevitable (there is no competing risk); and
3. the number of events at each time event is a small proportion of the number at risk at that time (<0.1).
I do not believe assumptions 1 (because members are lost to follow-up) and 2 (because the event is not inevitable, death is a
competing risk) hold for this cohort. Regardless, it is extremely close to the other results.
Using the Classical Life Table method (Szklo & Nieto, Epidemiology Beyond the Basics, 2000): the 3-year cumulative incidence
(probability) would equal 115/(1961 – ½(599+324)) = 115/1499.5 = .0767
In this method, half of those lost to follow-up are subtracted from those at risk, assuming that they were, on average, at risk for only
half that time period.
Using the Kaplan-Meier method: if you take into account the 3 time periods (which is ‘iffy’ considering we don’t know exact
onsets of epilepsy for some cases), the cumulative probability of epilepsy during 3 years is 1 –
[(1918/1961)*(1318/1362)*(1010/1038)] = .0791
Incidence rate based on aggregate data: 115/[(1961+1038)/2] = 115/1499.5 = .0767 per person-3 years = .0256 per person-year =
2.6 per 100 person-years.
Incidence rate per person-time: .0767 per person-3 years = .0256 per person-year = 2.6 per 100 person-years.
Confidence intervals using tabulated values of 95% confidence limit factors for a Poisson-distributed variable*. Observed number of
events on which estimate is based = 115. Lower limit factor for n=100 is 0.818, upper limit factor for n=100 is 1.22. Lower limit
factor for n=120 is 0.833, upper limit factor for n=120 is 1.200. Interpolated lower limit factor for 115 is 0.818 + .75(0.833 – 0.818) =
134
0.82925. Interpolated upper limit factor for 115 is 1.22 - .75(1.22 – 1.20) = 1.205. So, confidence limits for the 115 count are as
follows: lower = 115*0.82925 = 95.36; upper = 115*1.205 = 138.58,
and the 95% confidence limits for the rate are: lower = 95.36/1499.5 = 0.0636 per person-3 years; upper = 138.58/1499.5 = 0.0924
per person-3 years, or 2.1 and 3.1 per 100 person-years.
*Values from Haenszel W, Loveland DB, Sirken MG. Lung cancer mortality as related to residence and smoking histories, I. White males. Journal of the
National Cancer Institute. 28:947-1001, 1962.
I believe the most appropriate methods for this data are the Classical Life Table methods, or the incidence rate based on aggregate data
(which are equivalent). So, incidence rate of PTE = 2.6 per 100 person-years, 95% CI 2.1 – 3.1 per 100 person-years.
Determine risk stratifying by severity
Mild = AIS_H of 2 = 21/[(765+411)/2] = 21/588 = 0.0357 per person-3 year = 0.0119 per person-year = 1.2 per 100 person-years
LCL: .619*21 = 12.999; 12.999/588 = 0.0221 per person-3 year = 0.0074 per person-year = 0.7 per 100 person-years
UCL: 1.53*21 = 32.13; 32.13/588 = 0.0546 per person-3 year = 0.0182 per person-year = 1.8 per 100 person-years
Moderate = AIS_H of 3 = 16/[(322+165)/2] = 16/243.5 = 0.0657 per person-3 year = 0.0219 per person-year = 2.2 per 100 personyears
LCL: 0.572*16 = 9.152; 9.152/243.5 = 0.0376 per person-3 year = 0.0125 per person-year = 1.3 per 100 person-years
UCL: 1.62*16 = 25.92; 25.92/243.5 = 0.1064 per person-3 year = 0.0355 per person-year = 3.6 per 100 person-years
Severe = AIS_H of 4, 5 = 78[(874+462)/2] = 78/668 = 0.1168 per person-3 year = 0.0389 per person-year = 3.9 per 100 person-years
LCL: .785+[.80(.798-.785)] = 0.7954; .7954*78 = 62.0412; 62.0412/668 = 0.0929 per person-3 year = 0.0310 per person-year = 3.1
per 100 person-years
UCL: 1.27-[.80(1.27-1.25)] = 1.254; 1.254*78 = 97.812; 97.812/668 = 0.1464 per person-3 year = 0.0488 per person-year = 4.9 per
100 person-years
135
Appendix G - Sampling plan for inpatient and emergency department charts
Final Sampling Write-Up - Inpatient/ED
For each abstraction year (2001-2002) X number of records will be abstracted annually. In each year, 28.3%
of the records abstracted will have a diagnosis code of 345.0-345.9 (Epilepsy), 60% will have a diagnosis
code of 780.3 (Seizure NOS), 10% will have a diagnosis code of 780.2 (Syncope and Collapse), and 1.7%
will have a diagnosis code of 293.0 (Acute Delirium). The following is the process for drawing the stratified
random sample.
It is recommended that an unduplicated data set be used in order to have a person level sample.
Unduplicated Data Set:
1. Select all records in a calendar year that are from a South Carolina hospital for from individuals who
have a county of residence in SC. The individuals must be over the age of one when the encounter
occurred (this was inadvertently changed to include those under 1 year of age).
2. Every individual is assigned a unique ID. The unique ID was developed with the purpose to allow
person identification across different data systems. The estimated proportion of correctness for most
data sets is 99.5%
3. Individuals will be sorted based on unique ID and then the first record in order of date of occurrence
during the calendar year of interest will be pulled to create the sample universe. Since epilepsy is a
chronic condition, taking the first record in a calendar year is a random method for creating the
sample universe.
Once the unduplicated data set is created there will be a number of variables added to make pulling the
sample easier and more logical.
Organizing the Data Set:
1. Based on both primary and secondary diagnosis code (i.e. 345.x, 780.3, 780.2, and 293.0) each record
is assigned a group and could be assigned more than one group if the individual has multiple
diagnosis codes in the same record.
a. GroupA=345.x (epilepsy)
b. GroupB=780.3 (Seizure NOS)
c. GroupC=780.2 (Syncope and Collapse)
d. GroupD=293.0 (Acute Delirium)
IF (PDIAG=:'345') THEN GROUPA=1;
IF (SDIAG1=:'345') THEN GROUPA=2; IF (SDIAG2=:'345') THEN GROUPA=3;
IF (SDIAG3=:'345') THEN GROUPA=4; IF (SDIAG4=:'345') THEN GROUPA=5;
IF (SDIAG5=:'345') THEN GROUPA=6; IF (SDIAG6=:'345') THEN GROUPA=7;
IF (SDIAG7=:'345') THEN GROUPA=8; IF (SDIAG8=:'345') THEN GROUPA=9;
IF (PDIAG=:'7803') THEN GROUPB=1;
IF SDIAG1=:'7803' THEN GROUPB=2; IF SDIAG2=:'7803' THEN GROUPB=3;
IF SDIAG3=:'7803' THEN GROUPB=4; IF SDIAG4=:'7803' THEN GROUPB=5;
IF SDIAG5=:'7803' THEN GROUPB=6; IF SDIAG6=:'7803' THEN GROUPB=7;
IF SDIAG7=:'7803' THEN GROUPB=8; IF SDIAG8=:'7803' THEN GROUPB=9;
136
IF PDIAG=:'7802' THEN GROUPC=1;
IF SDIAG1=:'7802' THEN GROUPC=2; IF SDIAG2=:'7802' THEN GROUPC=3;
IF SDIAG3=:'7802' THEN GROUPC=4; IF SDIAG4=:'7802' THEN GROUPC=5;
IF SDIAG5=:'7802' THEN GROUPC=6; IF SDIAG6=:'7802' THEN GROUPC=7;
IF SDIAG7=:'7802' THEN GROUPC=8; IF SDIAG8=:'7802' THEN GROUPC=9;
IF PDIAG=:'2930' THEN GROUPD=1;
IF SDIAG1=:'2930' THEN GROUPD=2; IF SDIAG2=:'2930' THEN GROUPD=3;
IF SDIAG3=:'2930' THEN GROUPD=4; IF SDIAG4=:'2930' THEN GROUPD=5;
IF SDIAG5=:'2930' THEN GROUPD=6; IF SDIAG6=:'2930' THEN GROUPD=7;
IF SDIAG7=:'2930' THEN GROUPD=8; IF SDIAG8=:'2930' THEN GROUPD=9;
RUN;
2. Once all the records have been assigned a group, they will be given another variable that will tell
what type of record it is to help when drawing the sample. This is simply to make understanding the
program clearer.
IF GROUPA GE 1 THEN EPILEPSY=1;
IF GROUPB GE 1 THEN NOS=1;
IF GROUPC GE 1 THEN SYNC=1;
IF GROUPD GE 1 THEN AD=1;
RUN;
3. After every record is assigned the appropriate groupings (remember they can be in more than one
group) there will be four different random samples drawn to match the sampling proportion presented
in the grant. However, no record will be chosen more than once if that record falls in more than one
group.
DATA EPILEPSY;
SET TABLE2;
IF EPILEPSY=1; run;
PROC FREQ DATA=EPILEPSY; tables LOCATE / outpct out=size; run;
DATA SIZE;
SET SIZE;
_NSIZE_=ROUND((PERCENT/100)*850); RUN;
PROC SORT DATA=EPILEPSY; BY LOCATE; RUN;
PROC SORT DATA=SIZE; BY LOCATE; RUN;
PROC SURVEYSELECT
DATA=EPILEPSY METHOD=SRS OUT=OUT.UNEPSAMP SAMPSIZE=SIZE;
STRATA LOCATE ;
TITLE'UNDUPSAMP';
RUN;
From an e-mail asking for clarification from ORS: ‘For a given
sampling year (which is the Calendar year) there was a hierarchy for the diagnosis, but
no hierarchy for primary vs. secondary diagnosis or inpatient vs outpatient.’
137
Appendix H- Sampling plan for physician office charts
Sampling Write-Up -- physician office visits
Sample 1 – 360 (8:2 ratio of epilepsy:seizure)
• Medicaid – 86
• Medicare – 175
• SHP – 99
Sample 2 – 61 (Still 8:2 ratio and exclude one neurology practice)
• Medicaid – 17
• Medicare – 35
• SHP – 9
Sample 3 – 60 (All Medicare)
Sample 4 – 101 (Keep 8:2 ratio and exclude Columbia and Charleston practices)
• Kept all 81 epilepsy records left and drew additional 20 needed to keep 8:2 ratio
• Medicaid – 16
• Medicare – 52
• SHP – 32
Epilepsy = 345.x, seizure = 780.3.
Sampling excluded anyone who had had an inpatient or ED visit in 2001 or 2002.
138
ACKNOWLEDGMENT
We express our heartfelt gratitude and appreciation to the following people for their participation in the
South Carolina Epidemiological Studies of Epilepsy and Seizure Disorders.
The South Carolina Department of Health and Environmental Control, especially
Ms. Lou-Ann Carter
Ms. Georgette Demian
Ms. Lynnore Liggins
Mr. Wesley Gravelle
Ms. Harriet Range
Ms. Beili Dong
Dr. Jennifer Chiprich
The Office of Research and Statistics, South Carolina Budget and Control Board, especially
Mr. Andrew Pope
Mr. Christopher Finney
The Epilepsy Foundation of South Carolina, especially
Ms. Christine Porter
Ms. Barbara Brothers
Department of Neurosciences and Clinical Neurophysiology Services,
Medical University of South Carolina, especially
Ms. Kelly Cavins
Ms. Kris Topping
Department of Physical Therapy, Colorado State University,
Dr. Patricia Sample
Center for Health Services and Policy Research, University of South Carolina,
Ms. Lyn Phillips
Division of Adult and Community Health, National Center for Chronic Disease Prevention and Health
Promotion, Centers for Disease Control and Prevention, especially
Ms. Rosemarie Kobau
139