cme: The Differential Diagnosis of Right Lower Quadrant Pain
advertisement

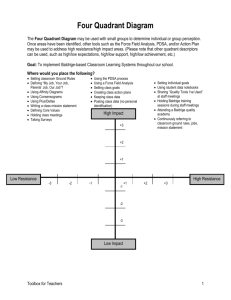
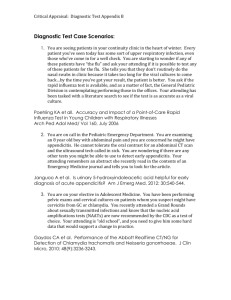
MEDICINE cme: The Differential Diagnosis of Right Lower Quadrant Pain Martin E. Kreis, Franz Edler v. Koch, Karl-Walter Jauch, Klaus Friese SUMMARY Introduction: There are numerous differential diagnoses for right lower quadrant pain, which can present in a variety of ways. Methods: Selective literature review. Results/Discussion: The most frequent differential diagnoses are acute appendicitis and diseases of the female genital tract. However, a variety of rarer diseases involving several medical subspecialties can also underlie this symptom. While acute appendicitis may be diagnosed relatively simply, sophisticated diagnostic tests may be needed to identify other disorders, particularly where the clinical presentation is atypical. Close interdisciplinary cooperation with other specialties is of major importance for the optimal management of right sided lower abdominal pain. Dtsch Arztebl 2007; 104(45): A 3114–21 Key words: acute abdomen, appendicitis, differential diagnosis, pelvic inflammatory disease, right lower quadrant pain A cute right lower quadrant pain is the most common type of acute abdomen (e1). This symptom has many different causes, particularly in female patients; the most common cause requiring surgery is acute appendicitis (e1, e2). The diagnostic assessment of right lower quadrant pain presents a challenge, not just because of the variety of causes, but also because the leading entities in the differential diagnosis are very different depending on the patient's age and sex (1, 2, e3). Immune-suppressed patients with an acute abdomen are often oligosymptomatic even when seriously ill (1, 3). Patients with right lower quadrant pain often come to medical attention during off hours and therefore require an efficient and goal-directed diagnostic assessment to receive the proper treatment as soon as possible. The assessment must often be carried out at times when the availability of ancillary testing is limited. The importance of speed should not be underestimated: patients with a perforated hollow viscus, for example, can be seriously endangered by delays in treatment (e4). In this article, we will discuss the most important clinical entities causing right lower quadrant pain, and we will propose an algorithm for its rapid and efficient diagnostic assessment, taking into consideration the often limited access to ancillary testing. Previous articles in this journal about the acute abdomen have dealt with the problem from a single specialty's point of view (e5) and have considered the differential diagnosis of upper abdominal pain (e6). Here, we consider the diagnostic assessment and management of right lower quadrant pain. Treatment will not be discussed in detail. This article is based on a selective review of published reports that were retrieved by a PubMed search on the following terms: "acute abdomen," "appendicitis," "right-sided lower abdominal pain," "right lower quadrant pain," and "pelvic inflammatory disease." Chirurgische Klinik und Poliklinik, Klinikum Großhadern, München: PD Dr. med. Kreis, Prof. Dr. med. Dr. h. c. Jauch; Klinik und Poliklinik für Frauenheilkunde und Geburtshilfe, Klinikum Großhadern, München: PD Dr. med. Edler von Koch, Prof. Dr. med. Friese Right lower quadrant pain Its diagnostic assessment presents a challenge because the leading entities in the differential diagnosis are different depending on the patient's age and sex. Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 1 MEDICINE History and physical examination: the key elements of case stratification The history and physical examination are the key elements leading to the determination of the diagnosis and of the further management of the patient (4, e7). The physician should inquire in general about the onset, duration, nature, and intensity of the pain, as well as about the following specific features: > Defecation: has the patient noticed any abnormalities? > Is the patient suffering from nausea, vomiting, or alguria/dysuria (painful or otherwise abnormal micturition)? In female patients, a gynecological history is obligatory and often points to the diagnosis. In taking the history, the physician should always try to gain information of differential diagnostic value in order to determine which further tests should be performed. The physical examination serves the same purpose. The physician should inspect, auscult, and palpate the abdomen, look for guarding and peritoneal signs, check the renal beds and potential hernia sites, and perform a digital rectal examination. Female patients should have an intravaginal examination as well, as a component of the acute gynecological consultation (e8). Diagnostic testing as an adjunct to clinical examination Testing with diagnostic apparatus should be performed only after the history and physical examination have been completed. Its purpose is to confirm the diagnosis that seems most likely among the possible differential diagnoses and to exclude all of the competing diagnoses (box). If appendicitis is suspected, a blood draw for laboratory testing (e9, 5) and an ultrasonographic examination of the abdomen are indicated (e10, 6). These tests can be performed quickly and with negligible distress to the patient. It should be borne in mind, however, that these tests are not very sensitive or specific. Conditions affecting the female reproductive tract, such as adnexitis, symptomatic ovarian cysts, or extrauterine pregnancy, are common causes of right lower quadrant pain; thus, a properly performed gynecological examination is recommended, combined with an endovaginal ultrasonographic examination, as long as it can be performed in an acceptably short time frame (7, 8). If a woman with right lower quadrant pain is first seen by a gynecologist and the cause of the trouble is not definitively found to be gynecological, then a general surgeon should be consulted next. The same procedure applies to patients who present with additional symptoms or findings in the urological area, e.g., renal percussion tenderness, alguria/dysuria, or macrohematuria, or in the orthopedic/neurological area, e.g., movement-related pain, radicular or pseudoradicular symptoms, and percussion tenderness of the spine. The specialists that are consulted to evaluate symptoms of these types will then determine the indication for further tests such as > Extended urinalysis > Voiding urography > Plain x-rays of the pelvis and spine > Spinal CT. If there are right lower quadrant symptoms suggesting perforation (e.g., due to right-sided diverticulitis) or ileus, then plain abdominal and chest x-rays should be obtained to determine the possible presence of free intraperitoneal air or adynamic intestinal loops (figure 1). Plain films of the abdomen should not be obtained routinely in the diagnostic assessment of right lower quadrant pain. Unless these are ordered to answer a specific question, their diagnostic value is limited (9, e11). If the initial diagnostic evaluation has not revealed any definitive or suspected diagnosis, it would seem more reasonable either to observe the History In women with right lower quadrant pain, a gynecological examination often leads to the diagnosis. Systematic history-taking If the patient has been examined by a gynecologist and her symptoms do not appear to be due to a gynecological problem, a general surgeon should be consulted. Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 2 MEDICINE BOX The most common causes of right lower quadrant pain > Surgery/Gastroenterology – Acute appendicitis – Gastroenteritis (bacterial/viral) – Mesenteric lymphadenitis (Yersinia enterocolitica infection) – Perforated or infected cecal pole diverticulum – Sigmoid diverticulitis or perforation – Crohn's disease, ulcerative colitis – Carcinoma of the colon – Ileus – Meckel's diverticulum > Gynecology – Adnexitis/tubo-ovarian abscess – Extrauterine pregnancy – Torsion of an ovarian cyst > Urology – Cystitis/pyelonephritis – Urolithiasis – Tumors of the urinary tract > Neurology/orthopedics – Radicular/pseudoradicular symptoms of disc prolapse or protrusion – Coxarthrosis – Sacroileitis – Herpes zoster patient further and reassess at close intervals or to proceed right away to computerized tomography, depending on the severity of the symptoms ([10, 11]; see also the diagnostic algorithm shown in diagram 1). Differential diagnosis: the typical causes of right lower quadrant pain Up to this point, we have discussed the initial steps in the evaluation of all cases of right lower quadrant pain. We will now describe its various typical and common causes, classified according to the relevant medical specialties. It should be borne in mind that patients' complaints are highly variable and often atypical. This factor complicates the diagnostic process still further. Moreover, in each specialty area there are rarer causes of right lower quadrant pain, not all of which can be listed here. Surgery/gastroenterology Appendicitis is probably the most common cause of right lower quadrant pain. The abdominal pain is typically diffuse and poorly localizable at first, until it becomes concentrated in the right lower quadrant (e9). Classic symptoms are nausea, vomiting, and cessation of defecation. Plain abdominal x-ray Plain films of the abdomen should not be obtained routinely in the diagnostic assessment of right lower quadrant pain. Unless they are ordered to answer a specific question, their diagnostic value is limited. Diagnostic assessment Appendicitis is the most common cause of right lower quadrant symptoms. Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 3 MEDICINE Patients generally present to medical attention after having suffered abdominal pain for 1 or 2 days. Examination usually discloses localized lower abdominal pain and peritoneal signs at McBurney's or Lanz's point, including percussion tenderness, rebound pain, and local guarding (diagram 2). Patients with appendicitis may also have the following: > Blumberg's sign: contralateral rebound pain (e9, 5) > The psoas sign: pain on lifting of the straightened right leg against resistance. This is a classic finding of retrocecal appendicitis. > Rovsing's sign: pain when manual pressure is applied to the ascending colon in a retrograde direction. Figure 1: Plain abdominal x-ray of a 53year-old woman presenting with an acute abdomen. The typical findings of ileus are present: adynamic loops of small bowel, with fluid levels. Fever may or may not be present. Studies have not confirmed the hypothesis that the difference between the axillary and rectal temperatures is of diagnostic significance (12, e12). The same holds for the digital rectal examination (e12, 13), though it is in any case an integral part of a thorough physical examination of the abdomen. Further information can be obtained by ultrasonography (concentric ring sign, free fluid) and by laboratory testing (leukocytosis) (e10, 6, 12). Modern computerized tomography enables appendicitis to be diagnosed with high sensitivity and specificity (11, 14, e13). Nonetheless, because of its cost and the radiation exposure associated with it, the use of CT as a routine investigation in all patients with acute right lower quadrant pain cannot be justified. If the typical symptoms and signs of appendicitis are present, the correct diagnosis can be established and a decision to operate can be made on clinical grounds alone. The protean manifestations of appendicitis make it impossible to state universally applicable rules about when to operate. In general, however, whenever appendicitis is strongly suspected, the patient should be taken to surgery. The suspicion of appendicitis is usually based on the clinical findings (local peritoneal signs and guarding) but can also be derived from ancillary tests. To the best of the authors' knowledge, it is common practice in most hospitals to rely more on the clinical findings than on ancillary tests in cases of doubt. Appendicitis can usually be distinguished from bacterial or viral gastroenteritis on clinical grounds (the latter is associated with recent consumption of possibly tainted food, vomiting, diarrhea, absence of peritoneal signs and guarding, and hyperperistaltic bowel sounds [12]). Chronic inflammatory bowel diseases such as Crohn's disease and ulcerative colitis can produce symptoms and signs resembling those of acute gastroenteritis; these entities should be suspected in patients with chronically recurring diarrhea, weight loss, a history of perianal fistulae, and a prior appendectomy. Right lower quadrant pain is an The three steps in the diagnostic assessment of right lower quadrandt pain > History > Physical examination > Is appendicitis suspected? Appendicitis If the clinical assessment reveals entirely typical findings of appendicitis, the diagnosis and the indication for surgery can be established on clinical grounds alone. Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 4 MEDICINE DIAGRAM 1 Algorithm for the differential diagnostic assessment of right lower quadrant pain *1 Female patients with right lower quadrant pain should always consult a gynecologist if the gynecological examination can be performed in an acceptably short time frame. especially typical feature of terminal ileitis (e14). Gastroenteritis, Crohn's disease, and ulcerative colitis generally do not produce peritoneal signs or guarding unless a perforation has occurred. Often, these diseases can be distinguished from appendicitis by ultrasonography or CT (e10, 6, e13). Colonoscopy may be used for the definitive diagnosis of chronic inflammatory bowel disease but is not useful as an emergency diagnostic test because it requires prior bowel preparation with appropriate rinsing solutions. Further ancillary tests, such as plain x-ray of the abdomen with an emptied gastrointestinal tract and computerized tomography, should be performed in atypical cases and when yet other possible diagnoses are suspected (e13). In the surgical-gastroenterological area, another possible cause of right lower quadrant pain is diverticulitis (e15), which is particularly likely to arise in the right hemicolon in patients of Asian extraction (15). Even sigmoid diverticulitis can present in the right lower quadrant if a large sigmoid loop is present. Infection of a Meckel's diverticulum is a special type of diverticulitis that is only rarely correctly diagnosed preoperatively (e16). Other diseases causing right lower quadrant pain usually have further accompanying symptoms that can aid in the differential diagnosis. Tumors of the right hemicolon, for example, usually cause right lower quadrant pain only Further diagnostic testing Right lower quadrant pain is a typical manifestation of diseases affecting the terminal ileum. A CT or plain film of the abdomen should be obtained if the constellation of clinical findings is atypical. Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 5 MEDICINE DIAGRAM 2 The three pressure points of Blumberg, McBurney, and Lanz. after a long, chronic course; the affected patients may also complain of weight loss, altered bowel habits, and blood in the stool. Some other conditions causing pain in the right lower quadrant without peritoneal signs are: > Mesenteric lymphadenitis due to infection with Yersinia enterocolitica (16) > Inguinal hernia (palpable, pain often exacerbated by the Valsalva maneuver) > Adhesion ileus (symptoms of ileus, lack of flatus or defecation) > Adhesion-related pain, classically occurring in a patient who has previously had an appendectomy (17). If the clinical examination and ancillary tests do not provide a clear answer and the abdominal symptoms and signs are so severe that the presence of a life-threatening condition cannot be ruled out with certainty, diagnostic laparoscopy should be performed (e17). Diagnostic laparoscopy can also be used instead of laparotomy when an acute disease process in the abdomen has already been successfully diagnosed on the basis of the clinical examination, laboratory tests, and imaging studies. Laparoscopy often enables immediate treatment of the problem, e.g., by laparoscopic appendectomy. The known contraindications to laparoscopy should be borne in mind, however, including a history of extensive abdominal surgery (18). Gynecology Appendicitis is suspected and then not confirmed at surgery more often in women than in men (14, e18). This fact indicates the major importance of gynecological conditions in the differential diagnosis of appendicitis (7). Among the various types of infectious/inflammatory change coming under the heading of "pelvic inflammatory disease" (PID), the most important differential diagnoses of appendicitis are acute adnexitis/salpingitis, abscesses in the adnexal region, and parametritis (e19). Like appendicitis, acute adnexitis often presents in atypical fashion and can then be definitively diagnosed only by laparoscopy. It characteristically arises in sexually active women, is often bilateral, and is sometimes accompanied by abnormal vaginal bleeding or discharge. In many cases, acute adnexitis arises in connection with the use of an intrauterine contraceptive device (IUD or spiral) (19). Palpation generally yields no definitive findings. Unless an abscess has formed, the oviducts are often not especially thickened and therefore Diagnostic laparoscopy Diagnostic laparoscopy can be performed when the foregoing clinical, laboratory, and imaging tests all point to an acute intra-abdominal process. Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 6 With permission from K. Jundt MEDICINE Figure 2: Extrauterine pregnancy usually not palpable. There may be lower abdominal guarding, pain on passive movement of the cervix, and/or uterine tenderness to palpation. Laboratory testing only reveals elevated inflammatory parameters. Vaginal ultrasound can reveal the diagnosis if the oviducts are markedly distended by pus or blood (pyosalpinx or hematosalpinx) (e20). Another gynecological disease that can cause acute right lower quadrant pain is ectopic pregnancy (figure 2). Its manifestations include > Secondary amenorrhea > A positive pregnancy test > Normal inflammatory parameters > Abnormal vaginal bleeding. Extrauterine pregnancy often becomes symptomatic when it perforates, causing a potentially life-threatening intra-abdominal hemorrhage (e21). Patients may have a history of bouts of adnexitis or a prior extrauterine pregnancy. The diagnosis can often be made with endovaginal ultrasonography (20). An adnexal mass is seen; sometimes the fetal heartbeat can be seen as well. The uterine cavity is usually empty even though the endometrium is greatly thickened. The "pseudogestational sac" that is sometimes found in the uterine cavity by ultrasonography makes an intrauterine pregnancy more difficult to rule out. Extrauterine pregnancies are often found in the oviducts but can also be located in an ovary or in the peritoneal cavity. Torsion of an ovarian tumor or cyst, or cyst rupture, can also cause acute right lower quadrant pain. In cases of torsion, ultrasonography usually reveals a fairly large ovarian cyst (> 5 cm). In many cases, Doppler ultrasonography reveals diminished or absent blood flow in the affected ovary (21). This entity causes very severe pain that generally arises quite suddenly, e.g., in connection with intense physical activity such as sport or dancing. In premenopausal women, ovulation itself can sometimes cause acute lower abdominal pain, even if the menstrual cycles are regular. A carefully obtained history (last menstrual period, previous episodes of mid-cycle pain) can yield important diagnostic clues (2). Whenever the clinical findings lead to no clear diagnosis, and particularly in young women who may be suffering either from appendicitis or from adnexitis, laparoscopy is a good option (e19) that should be considered if the patient wishes to avoid the radiation exposure associated with CT. Urological causes Lower abdominal pain can also be due to urological causes such as macroor microhematuria, renal tenderness, and dys- or alguria. Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 7 MEDICINE Urology Right lower quadrant pain is rarely the major clinical finding of an acute urological illness, but it can nevertheless be the presenting symptom of pyelonephritis, urinary colic, cystitis, or a tumor of the urinary tract. In all of these cases, it is usually accompanied by other symptoms or signs pointing to the urological origin of the problem (22), including macroor microhematuria, renal percussion tenderness, and dys- or alguria. Obstructions to the flow of urine can often be seen when ultrasonography is performed as part of the emergency diagnostic evaluation. If any of the above manifestations are present in a patient with acute right lower quadrant pain, urological consultation should be obtained. If the urologist also suspects a urological condition, contrast-enhanced CT or micturition urography can be performed to complete the diagnostic evaluation (e22). Orthopedics/neurology Orthopedic and neurological conditions, like urological conditions, generally do not cause isolated right lower quadrant pain; rather, the pain is typically accompanied by other symptoms and signs. Leukocytosis is absent, and abdominal ultrasonography is unremarkable. The pain is classically associated with movement and can be deliberately manually provoked at its site of origin (e8) when it is due to conditions such as > Coxarthrosis > Sacroileitis > Intervertebral disc prolapse > Lumbago. The absence of fever and laboratory changes indicating inflammation is a further criterion by which these processes can be distinguished from an acute infectious/inflammatory disease in the abdomen. Rare causes of right lower quadrant pain There are a large number of rarer causes of right lower quadrant pain, including common iliac artery aneurysm (23), infarction of the cecal pole (24), cecal volvulus (25), and intussusception (19). These entities can usually be recognized by CT or by laparoscopy. Abdominal pain is only rarely caused by a systemic metabolic disease or temporary metabolic derangement. Diabetic ketoacidosis is easily distinguished from an infectious or inflammatory process in the abdomen by the history and by simple laboratory tests. Acute intermittent porphyria is exceedingly rare and often hard to diagnose because its abdominal manifestations are combined with mental changes and variable neurological manifestations. A change of the color of the urine to dark red on exposure to light is the classic diagnostic criterion. Even if the patient is known to suffer from a systemic metabolic disease, this disease is not necessarily the cause of the abdominal pain, because an intra-abdominal cause may be present as well. Thus, the treating physician should always take care to exclude other causes. Further systemic diseases that can mimic a local abdominal disturbance include heavy metal poisoning (lead, thallium, arsenic) and familial hyperlipoproteinemias with hypertriglyceridemia. When poisoning is suspected, the physician should attempt to determine the nature of the exposure; in lipid metabolic disorders, further manifestations of the disease should be sought, e.g., xanthomatoses or lipemic retinitis (e23). Overview Right lower quadrant pain can be due to a large variety of diseases whose causes must be diagnosed and treated by physicians from a number of different specialties. If the clinical Rare causes Abdominal pain is only rarely due to a metabolic disturbance or systemic metabolic disease. Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 8 MEDICINE manifestations are sufficiently typical, extensive ancillary diagnostic testing can often be dispensed with. If the findings are unclear, however, modern radiological studies should be performed as soon as possible, as these will make an important contribution to the diagnostic process. When the cause of acute right lower quadrant pain is not immediately evident, a rapid and interdisciplinary evaluation is essential, because delays in treatment lead to excess morbidity and mortality. Conflict of Interest Statement The authors state that they have no conflict of interest as defined by the guidelines of the International Committee of Medical Journal Editors. Manuscript received on 23 February 2007; final version accepted on 4 September 2007. Translated from the original German by Ethan Taub, M.D. REFERENCES For e-references please refer to the additional references listed below. 1. Laurell H, Hansson LE, Gunnarsson U: Acute abdominal pain among elderly patients. Gerontology 2006; 52: 339–44. 2. O´Byrne JM, Dempsey CB, O`Malley MK, O´Connel FX: Non-specific abdominal pain in pre-menopausal women. Ir Med Sci 1991; 160: 344–6. 3. Menegaux F: Acute abdominal pain in immunodepressed patients. Rev Prat 2001; 51: 1665–9. 4. Bohner H, Yang Q, Franke K, Ohmann C: Significance of anamnesis and clinical findings for diagnosis of acute appendicitis. Acute Abdominal Pain Study Group. Z Gastroenterol 1994; 32: 579–83. 5. Andersson REB: Meta-analysis of the clinical and laboratory diagnosis of appendicits. British J Surg 2004; 91: 28–37. 6. Lehmann D, Uebel P, Weiss H, Fiedler L, Bersch W: Sonographic representation of the normal and acutely inflamed appendix in patients with right sided abdominal pain. Ultraschall Med 2000; 21: 101–6. 7. Bonqard F, Landers DV, Lewis F: Differential diagnosis of appendicitis and pelvic inflammatory disease. A prospective analysis. Am J Surg 1985; 150: 90–6. 8. Sivyer P: Pelvic ultrasound in women. World J Surg 2000; 24: 188–97. 9. Boleslawski E, Panis Y, Benoist S, Denet C, Mariani P, Valleur P: Plain abdominal radiography as a routine procedure for acute abdominal pain of the right lower quadrant: prospective evaluation. World J Surg 1999; 23: 262–4. 10. Mackersie AB, Lane MJ, Gerhardt RT, Claypool HA, Keenan S, Katz DS, Trucker J: Nontraumtic acute abdominal pain: unenhanced helical CT compared with three-view acute abdominal series. Radiology 2005; 237: 114–22. 11. Macari M, Balthazar EJ: The acute right lower quadrant: CT evaluation. Radiol Clin North Am. 2003; 41: 1117–36. 12. Putzki H, Reichert B: Does measuring axillo-rectal temperature difference help in the diagnosis of acute appendicitis? Langenbecks Arch Chir 1988; 373: 310–2. 13. Dixon JM, Elton RA, Rainey JB, MacLeod DAD: Rectal examination in patients with pain in the right lower quadrant of the abdomen. BMJ 1991; 302: 386–8. 14. Morse BC, Roettger RH, Kalbaugh CA, Blackhurst DW, Hines WB Jr: Abdominal CT scanning in reproductive-age women with right lower quadrant abdominal pain: does its use reduce negative appendectomy rates and healthcare costs? Am Surg 2007; 73: 580–4. 15. Chan CC, Lo KK, Chung EC, Lo SS, Hon TY: Colonic diverticulosis in Hong Kong: distribution pattern and clinical significance. Clin Radiol 1998; 53: 842–4. 16. Perdikogianni C, Galanakis E, Michalakis M, Giannoussi E, Maraki S, Tselentis Y, Charissis G: Yersinia enterocolitica infection mimicking surgical conditions. Ped Surgery Int 2006; 22: 589–92. 17. Kreis ME, Jauch KW: Surgical treatment of ileus. Differential diagnosis and therapeutic results. Chirurg 2006; 77: 883–8. 18. Keller R, Kleemann M, Hildebrand P, Roblick UJ, Bruch HP: Diagnostische Laparoskopie beim akuten Abdomen. Chirurg 2006; 77: 981–5. 19. Matsuba, Y, Mizuiri H, Murata T, Nimi K: Adult intussusception due to lymphangioma of the colon. J Gastroenterol 2003; 38: 181–5. 20. Gurel S, Sarikaya B, Gurel K, Akata D: Role of sonography in the diagnosis of ectopic pregnancy. J Clin Ultrasound 2007 13 Aug e-pub ahead of print. 21. Willms AB, Schlund JF, Meyer WR: Endovaginal Doppler ultrasound in ovarian torsion: a case series. Ultrasound Obstet Gynecol 1995; 5: 129–32. 22. Paajanen H, Tainio H, Laato M: A chance of misdiagnosis between acute appendicitis and renal colic. Scand J Urol Nephrol 1996; 30: 363–6. 23. Tsatalpas P, Butters M: Aneurysms of the iliac artery in fibromuscular dysplasia as differential diagnostic consideration in acute lower abdominal pain. Zentralbl Chir 1997; 122: 413–7. 24. Schuler JG, Hudlin MM: Cecal necrosis: infrequent variant of ischemic colitis. Report of five cases. Dis Colon Rectum 2000; 43: 708–12. 25. Kokoska ER, Herndon CD, Carney DE, Lerner M, Grosfeld JL, Rink RC, West KW: Cecal volvulus: a report of two cases occurring after antegrade colonic enema procedure. J Pediatr Surg 39: 916–9. ADDITIONAL REFERENCES e1. Reifferscheid M, Weller S: Chirurgie. Stuttgart: Georg Thieme Verlag 1986; 153–62. e2. Miettinen P, Pasanen P, Lahtinen J, Alhava E: Acute abdominal pain in adults. Ann Chir Gynaecol 1996; 85: 5–9. e3. Quan M: Pelvic inflammatory disease: diagnosis and management. J Am Board Fam Pract 1994; 7: 110–23. Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 9 MEDICINE e4. Svanes C: Trends in perforated peptic ulcerr: incidence, etiology, treatment, and prognosis. Word J Surg 2000; 24: 277–83. e5. Lankisch PG, Mahlke R, Lübbers H: Das akute Abdomen aus internistischer Sicht. Dtsch Arztebl 2006; 103(33): A2179–88. e6. Niedergethmann M, Post S: Differenzialdiagnose des Oberbauchschmerzes. Dtsch Arztebl 2006; 103(13): A 862–71. e7. Joppich I et al.: S1-AWMF-Leitlinie der Deutschen Gesellschaft für Kinderchirurgie 2002. e8. Bates B: A guide to physical examination and history taking. 4th edition. Philadelphia: Lippincott Company 1987; 333–50. e9. Amman R: Schmerzen im Bereich des Abdomens. In: Siegenthaler W (Hrsg.): Diagnose innerer Krankheiten. Stuttgart: Georg Thieme Verlag 1988; S. 20.1–20.19 e10. Jahn H, Mathiesen FK, Neckelmann K, Hovendal CP, Bellstrom T, Gottrup F: Comparison of clinical judgment and diagnostic ultrasonography in the diagnosis of acute appendicits: experience with a score-aided diagnosis. Eur J Surg 1997; 163: 433–43. e11. Rao PM, Rhea JT, Rao JA, Conn AK: Plain abdominal radiography in clinically suspected sppendicitis: diagnostic yield, resource use, and comparison with CT. Am J Emerg Med 1999; 17: 325–8. e12. John H, Neff U, Kelemen M: Appendicitis diagnosis today: clinical and ultra-sonic deductions. World J Surg 1993; 17: 243–9. e13. Hof K H, van Lankeren W, Krestin GP, Bonjer HJ, Lange JF, Becking WB, Kazemeier G: Surgical validation of unenhanced helical computed tomography in acute appendicits. British J Surg 2004; 91: 1641–5. e14. Starlinger M: Chirurgische Therapie des Morbus Crohn. In: Adler G (Hrsg.): Morbus Crohn – Colitis ulcerosa. Berlin: Springer Verlag 1996; 263–93. e15. Neff CC, van Sonnenberg E: CT of diverticulitis. Diagnosis and treatment. Radiol Clin North Am 1989; 27: 743–52. e16. McKay R: High incidence of symptomatic Meckel´s diverticulum in patients less than fifty years of age: an indication for resection. Am Surg 2007; 73: 271–5. e17. Schietroma M, Cappelli S, Carlei F, Pescosolido A, Lygidakis NJ, Amicucci G: "Acute abdomen": early laparoscopy or active laparotomic-laparoscopic observation? Hepatogastroenterology 2007; 54: 1137–41. e18. McDonald GP, Pendarvis DP, Wilmoth R, Daley BJ: Influence of preoperative computed tomography on patients undergoing appendectomy. Am Surg 2001; 67: 1017–21. e19. Crossman SH: The challenge of pelvic inflammatory disease. Am Fam Physician 2006; 73: 859–64. e20. Horrow MM: Ultrasound of pelvic inflammatory disease. Ultrasound quarterly 2004; 20: 171–9. e21. Lozea AM, Potter B: Diagnosis and management of ectopic pregnancy. Am Fam Physician 2005; 72: 1707–14. e22. Miller NL, Lingemann JE: Management of kidney stones. BMJ 2007; 334: 468–72. e23. Andersson RE, Hugander AP, Ghazi SH, Ravn H, Offenbartl SK, Nyström PO, Olaison G: Diagnostic value of disease history, clinical presentation, and in-flammatory parameters of appendicits. World J Surg 1999; 23: 133–40. Corresponding author PD Dr. med. Martin E. Kreis Ludwig-Maximilians Universität München Chirurgische Klinik Großhadern Marchioninistr. 15 81377 München, Germany martin.kreis@med.uni-muenchen.de Further Information This article has been certified by the North Rhine Academy for Postgraduate and Continuing Medical Education. Deutsches Ärzteblatt provides certified continuing medical education (CME) in accordance with the requirements of the Chambers of Physicians of the German federal states (Länder). CME points of the Chambers of Physicians can be acquired only through the Internet by the use of the German version of the CME questionnaire within 6 weeks of publication of the article. See the following website: www.aerzteblatt.de/cme Participants in the CME program can manage their CME points with their 15-digit "uniform CME number" (einheitliche Fortbildungsnummer, EFN). The EFN must be entered in the appropriate field in the www.aerzteblatt.de website under "meine Daten" ("my data"), or upon registration. The EFN appears on each participant's CME certificate. The solutions to the following questions will be published in Volume 1–2/2008. The CME unit "The Purpose and Practice of Notification in Infectious Diseases" (Volume 41/2007) can be accessed until the 23rd November. For Volume 49/2007 we plan to offer the topic "The Involuntary Weight Loss of the Elderly". Solutions to the CME questionnaire in Volume 37/2007: Wojtecki L, Südmeyer M, Schnitzler A: Current Treatment of Parkinson’s Disease: 1/d, 2/b, 3/b, 4/c, 5/a, 6/d, 7/e, 8/e, 9/c, 10/b Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 10 MEDICINE Please answer the following questions to participate in our certified Continuing Medical Education program. Only one answer is possible per question. Please select the answer that is most appropriate. Question 1 Which of the following statements is correct? (a) Right lower quadrant pain is rare in patients presenting with abdominal symptoms. (b) Nausea and vomiting are atypical manifestations of appendicitis. (c) The absence of leukocytosis rules out appendicitis. (d) When the appendix is retrocecal, appendicitis usually causes a positive psoas sign. (e) Rebound tenderness in the left lower quadrant is not consistent with appendicitis. Question 2 Which of the following statements is correct? (a) Lanz's point is defined as the pressure point located 2 handbreadths above the navel. (b) Blumberg's sign is elicited by retrograde pressing on the colon. (c) Rovsing's sign of the left hemicolon is positive when there is contralateral rebound tenderness. (d) In acute appendicitis, tenderness and peritoneal signs are typically found at McBurney's point. (e) Appendicitis is always heralded by severe constipation. Question 3 In which of the following conditions are peritoneal signs usually found in the right lower quadrant? (a) Inguinal hernia (b) Adhesion-related ileus (c) Acute appendicitis (d) Mesenteric lymphadenitis (e) Adhesions after appendectomy Question 4 Which of the following statements about ruptured tubal pregnancy is correct? (a) The accompanying acute hemorrhage is often life-threatening. (b) It occurs so early in pregnancy that a pregnancy test is usually negative. (c) The pain is always only on the right side. (d) This disorder cannot be diagnosed by vaginal ultrasonography, because the oviducts are too far away from the head of the ultrasound device. (e) If this diagnosis is suspected, initial conservative management is a viable option. Question No. 5 Acute adnexitis (a) occurs only in sexually inactive women. (b) is always found bilaterally in the lower abdomen. (c) often causes pain on passive movement of the cervix. (d) is an important element of the differential diagnosis of appendicitis in men. (e) is usually accompanied by extreme weight loss. Question 6 Which of the following suggests that an attack of right lower quadrant pain is due to Crohn's disease? (a) Constipation (b) Weight gain (c) A history of perianal fistulae or abscesses (d) Increased hunger (e) Guarding in the right lower quadrant Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 11 MEDICINE Question 7 Gastroenteritis is characterized by: (a) Abdominal symptoms limited to the right lower quadrant (b) Constipation (c) Diffuse peritoneal signs (d) Hyperperistaltic bowel sounds (e) No generalized sense of feeling unwell Question 8 Urological diseases that cause right lower quadrant pain can also cause (a) Dysuria/alguria (b) Macro- or microhematuria (c) Renal percussion tenderness (d) Urinary obstruction that can be seen by ultrasonography (e) All of the above Question 9 Orthopedic/neurological diseases causing right lower quadrant symptoms are characterized by (a) Movement-related pain (b) High fever (c) Reproducibility of the pain with manual maneuvers (d) Leukocytosis (e) Abnormal abdominal ultrasonography Question 10 Which of the following statements is correct? Right lower quadrant pain due to systemic metabolic diseases or transient metabolic derangements (a) is common. (b) always occurs after the patient touches heavy metals. (c) can arise in diabetic ketoacidosis. (d) is never accompanied by neurological manifestations when the cause is acute intermittent porphyria. (e) may arise through an allergic reaction. CASE ILLUSTRATION: SEE NEXT PAGE Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 12 MEDICINE Case Illustration The Differential Diagnosis of Right Lower Quadrant Pain O ne morning after breakfast, this 24-year-old college German major felt mildly nauseated and unwell. At first she thought this was the effect of the previous day's lunch in the student cafeteria. By afternoon, she also had a diffuse abdominal ache, which she interpreted as an ordinary upset stomach. After the afternoon's lectures, she went to her general practitioner, who found tenderness to palpation in the epigastrium and in the right lower quadrant. To be on the safe side, he advised her to be examined in the university surgical clinic, because he could not rule out an incipient appendicitis. She considered this excessive and could not imagine at that point that she might need surgery. Later that night, however, her pain worsened, and she vomited some bilious material. She was now sufficiently worried to present to the surgical clinic and undergo an examination. When she was seen in the surgical outpatient department, the pain was already clearly localized to the right lower quadrant. Her nausea persisted, and she had not had a bowel movement all day. The examining physician documented the presence of local peritoneal signs, contralateral rebound tenderness, and a body temperature of 37.5°C. The bowel sounds were hypoactive. Laboratory tests disclosed a mild leukocytosis, and abdominal ultrasonography showed a concentric ring sign in the right lower quadrant. A gynecological consultation was obtained. No abnormalities were found by palpation or by endovaginal ultrasonography, but adnexitis could not be ruled out with certainty. Because of the local peritoneal signs and the difficulty of determining whether the symptoms were due to appendicitis or to a problem in the reproductive tract, the general surgeon on call recommended a diagnostic laparoscopy. At laparoscopy, phlegmonous appendicitis was found, and a laparoscopic appendectomy was performed. There were no further complications. The patient was discharged from the hospital two days later. Dtsch Arztebl 2007; 104(45): A 3114–21 ⏐ www.aerzteblatt.de 13