Lenz—Ped surgery—3.25.10 Evaluation of Pediatric Patient History
advertisement
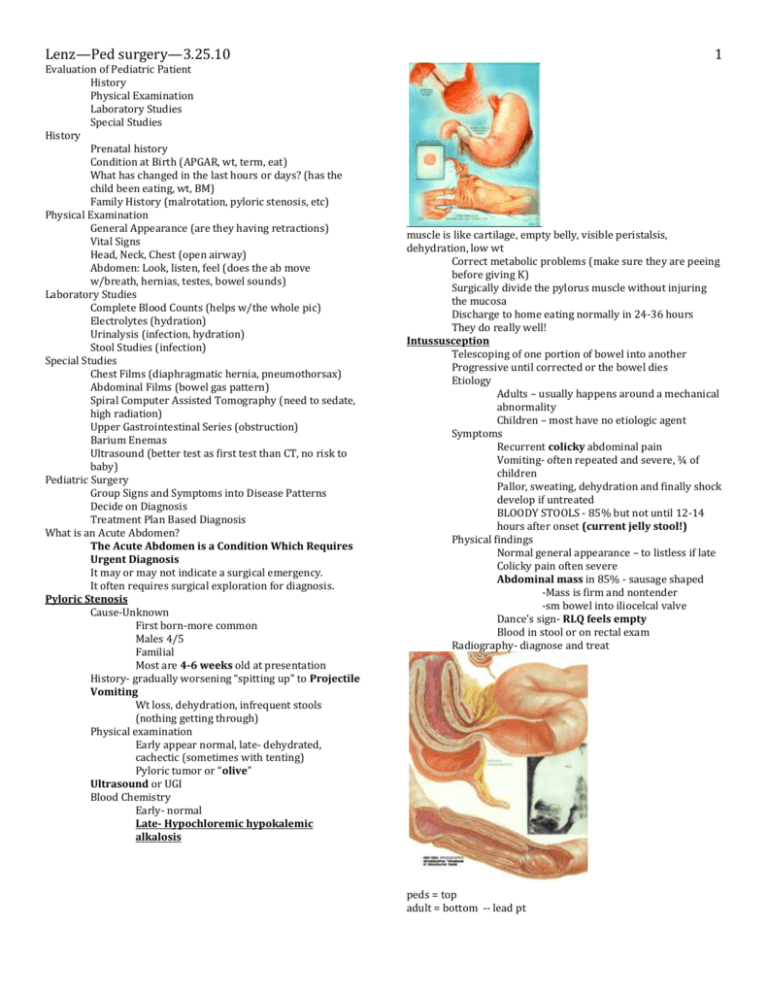
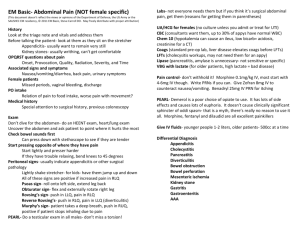
1 Lenz—Ped surgery—3.25.10 Evaluation of Pediatric Patient History Physical Examination Laboratory Studies Special Studies History Prenatal history Condition at Birth (APGAR, wt, term, eat) What has changed in the last hours or days? (has the child been eating, wt, BM) Family History (malrotation, pyloric stenosis, etc) Physical Examination General Appearance (are they having retractions) Vital Signs Head, Neck, Chest (open airway) Abdomen: Look, listen, feel (does the ab move w/breath, hernias, testes, bowel sounds) Laboratory Studies Complete Blood Counts (helps w/the whole pic) Electrolytes (hydration) Urinalysis (infection, hydration) Stool Studies (infection) Special Studies Chest Films (diaphragmatic hernia, pneumothorsax) Abdominal Films (bowel gas pattern) Spiral Computer Assisted Tomography (need to sedate, high radiation) Upper Gastrointestinal Series (obstruction) Barium Enemas Ultrasound (better test as first test than CT, no risk to baby) Pediatric Surgery Group Signs and Symptoms into Disease Patterns Decide on Diagnosis Treatment Plan Based Diagnosis What is an Acute Abdomen? The Acute Abdomen is a Condition Which Requires Urgent Diagnosis It may or may not indicate a surgical emergency. It often requires surgical exploration for diagnosis. Pyloric Stenosis Cause-Unknown First born-more common Males 4/5 Familial Most are 4-6 weeks old at presentation History- gradually worsening “spitting up” to Projectile Vomiting Wt loss, dehydration, infrequent stools (nothing getting through) Physical examination Early appear normal, late- dehydrated, cachectic (sometimes with tenting) Pyloric tumor or “olive” Ultrasound or UGI Blood Chemistry Early- normal Late- Hypochloremic hypokalemic alkalosis muscle is like cartilage, empty belly, visible peristalsis, dehydration, low wt Correct metabolic problems (make sure they are peeing before giving K) Surgically divide the pylorus muscle without injuring the mucosa Discharge to home eating normally in 24-36 hours They do really well! Intussusception Telescoping of one portion of bowel into another Progressive until corrected or the bowel dies Etiology Adults – usually happens around a mechanical abnormality Children – most have no etiologic agent Symptoms Recurrent colicky abdominal pain Vomiting- often repeated and severe, ¾ of children Pallor, sweating, dehydration and finally shock develop if untreated BLOODY STOOLS - 85% but not until 12-14 hours after onset (current jelly stool!) Physical findings Normal general appearance – to listless if late Colicky pain often severe Abdominal mass in 85% - sausage shaped -Mass is firm and nontender -sm bowel into iliocelcal valve Dance’s sign- RLQ feels empty Blood in stool or on rectal exam Radiography- diagnose and treat peds = top adult = bottom -- lead pt 2 Lenz—Ped surgery—3.25.10 -empty RLQ as SI enters colon -use air & pressure to reduce it 1-2 times, then take to surgery – remove bad tissue. Appendicitis History of patient Symptoms/Signs of the attack The Order of Occurrence (fever or vomit first is not appendicitis) History When first noted a problem Recent illnesses/ prior hx of similar pain/behavior (viral illness, sick, dif behavior colicky, etc) Medications- OTC or Rx (if on ABx suppressing some Sx of appendicitis, steroid for asthma attack can mask what is happening in the belly) Prior surgery (adhesions, malrotation, etc) Family history (have parents had appendicits, sick sib, etc) Signs and Symptoms Pain (epigastric then iliac) (whole tummy hurt yesterday, now it hurt right hear (McBurney’s pt) Nausea, vomiting and anorexia Local rigidity (inconstant) Local distention (inconstant) Fever Constipation (due to dec intake, dehydration) The Order of Occurrence of Symptoms -The specific order of symptoms can be very helpful in determining the diagnosis!! -Fever or vomiting prior to the onset of pain is much less likely to be appendicitis. -Pain that comes and goes is also not likely to be appendicitis -Leucocytosis is often not accurate! A normal WBC does not rule anything out!! High counts more assoc with pneumonia, leukemia, pylonephritis if over 30,000. -Infants rarely get appendicitis but are much more likely to have perforation at diagnosis (at presentation). -Ultrasound exams are much easier and more likely to be helpful in patients with minimal abdominal fat!! Thus they are a good study in infants and children if necessary -Treatment- open appendectomy usually through a RLQ muscle splitting incision or midline if suspicious of perforation. -Larger children may have laparoscopy -Noncomplicated cases may eat POD#1 and be home by POD#3 -Perforated patients with diffuse peritonitis may need hospitalization for weeks location of appendix determines Sx. Peak is spring/fall due to viral infections – when mesenteric nodes get large it can obstructs the lumen of appendix. Appendix is a safe home for good bacteria. -most common in 6-12 yr group, Dx made early so less likely to rupture. -over 3 days Sx they are ruptured. iliopsoas test – hyperextend thigh = pain obturator test = pain Practice Questions: 1. what is an acute abdomen? 2. 4 week old male presents with projectile vomiting and you can palpate an “olive” in his abdomen. What is the likely Dx? What do you expect his acid/base status to be? 3. Baby presents with colicky pain and current jelly stool, What is the most likely Dx? What physical exam and x-ray findings would confirm your Dx? 4. Child presents with diffuse abdominal pain that is now localized to the RLQ. Will a CBC make your diagnosis definitive? 5. If a patient presents with fever, vomiting or intermittent pain is appendicitis likely? Answers: 1. The Acute Abdomen is a Condition Which Requires Urgent Diagnosis 2. Pyloric stenosis. Early = normal, Late = Hypochloremic hypokalemic alkalosis 3. Sausauged shaped abdominal mass & Dance’s sign- RLQ feels empty 4. this is appendicitis, CBC can be inaccurate. 5. No