Standard procedures for assessing hypersecretion or secretory
advertisement

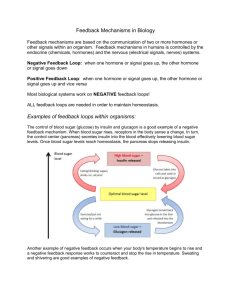
Downloaded from http://pmj.bmj.com/ on March 4, 2016 - Published by group.bmj.com Festschrift for Sir John McMichael 53 Standard procedures for assessing hypersecretion or secretory capacity for human growth hormone, using the radioimmunoassay RUSSELL FRASER A. D. WRIGHT Royal Postgraduate Medical School, London THERE are no easily measured clinical signs of growth hormone (GH) activity though it is closely reflected by growth in children, and by skin thickness, hair growth and skin secretory activity in adults. Yet there is need to assess GH activity, not only for the diagnosis and management of various pituitary disease, but also in the study of disease such as diabetes mellitus and its complications. A radioimmunoassay sufficiently sensitive to measure GH levels in body fluids (Glick et al., 1963; Hunter & Greenwood, 1964) has recently offered hopeful prospects for doing this. But the initial studies soon revealed the variability of normal GH levels (Knobil, 1966; Copinschi et al., 1967) and their rapid fluctuation with various stimuli (Glick et al., 1965). However, suitable diagnostic procedures for assessing GH activity in relation to various clinical problems have now evolved and here we shall appraise the use of some of these procedures, and define the normal responses. The radioimmunoassay of human growth hormone (HGH) While only one bioassay (Daughaday, Salmon & Alexander, 1959; Daughaday & Parker, 1963) is sufficiently sensitive to measure GH activity in serum, the radioimmunoassay is more sensitive and more specific. In this method radioactive HGH (labelled with 1311 or 125I) and a known amount of anti-HGH antibody is added to a series of tubes containing either a standard amount of unlabelled pure HGH or a diluted serum sample. Subsequent measurement of the percentage 131I or 1251 bound to the antibody is the basis of the assay, for this clearly should index the amount of unlabelled hormone added. When an effect is obtained from an unknown sample, its specificity can be assessed by comparing its dose response effect with that of the standard HGH preparation. Some substances, such as human placental lactogen, are partly identical with HGH (Greenwood, Hunter & Klopper, 1964), while GH from non-primate species are non-identical. Further, the radioimmunoassay can be affected non-specifically by such factors as plasma proteins, or changes of pH or ionic strength; effects which must be covered by the standardization of the assay procedure and adequate dilution of serum samples. Different methods are used to separate the antibody-bound and free fraction of labelled HGH. In our Unit we have developed this assay using the double-antibody method (Hartog et al., 1964b), using anti-y-globulin antiserum to precipitate the antibody-bound fraction. With suitable precautions (Welborn & Fraser, 1966), this method has certain advantages over the original chromatoelectrophoresis separation of Glick et al. (1963). It is particularly important to ensure that complete precipitation will occur under all the conditions possible in the assay. 131I-labelled -y-globulin in trace amounts provides a useful check for this precipitation, and the optimal concentrations of anti-y-globulin antiserum can be determined for the chosen concentration of y-globulin. Recent developments are evolving simpler separation methods, still needing careful appraisal of their sensitivity and specificity-such as dextran-coated charcoal (Lau, Gottlieb & Herbert, 1966) and silica powders (Rosselin et al., 1966) and solid synthetic protein-binding discs (Catt, Niall & Tregear, 1966). A good clinical assay should be adaptable to semi- or complete automation which is true of the double-antibody procedure. An immunologically pure, radioactively labelled hormone is essential for the assay. The hormone becomes damaged to some extent during the labelling, during subsequent storage and during the 4-7 days incubation for the assay. Fractionation of the prepared 1311-HGH by gel filtration as described by Touber & Maingay (1963) is a simple purification step which we use routinely. A fraction, up to 40% of which will bind to protein in the absence of anti-HGH Downloaded from http://pmj.bmj.com/ on March 4, 2016 - Published by group.bmj.com 54 Postgraduate Medical Journal antiserum, can be separated from the immunologically pure hormone (Fig. 1). Incubation damage of the labelled hormone can be avoided by limiting the specific radioactivity to 200 uCi/ ,tg HGH and also by assaying the serum diluted to at least 1: 5 in the final incubate. W steroids (Hartog et al., 1964a) and some drugs acting on the central nervous system (Muller et al., 1967), the response to insulin hypoglycaemia is suppressed. It is therefore important to standardize the conditions under which samples are collected. Standard clinical tests The HGH level in routine fasting serum samples varies considerably unless the status at collection is basal (Copinschi et al., 1967). Basal samples should only be taken after ensuring rest and calm for +-1 hr. Since, however, a basal status cannot be ensured, a standard suppression test, such as oral glucose (GTT), is useful. Further truly basal levels are often too low to be measured in normals and a standard stimulation such as intravenous insulin (ITT) is also important for suspected loss of secretory capacity. 0 0 0 4- 4 8 Sample No. 12-->23/6/65 [5ml sampl FIG. 1. Fractionation of 1311-HGH on Sephadex G-200 (15 x 1 *2 cm). The results of the assays in this paper are expressed in terms of the M.R.C. reference standard 'A', kindly supplied by Dr D. R. Bangham. The precision of our assay has been assessed by reviewing the results of the standard sera assayed each day. For samples above 10 ng/ml, the coefficient of variation of the mean value has ranged between 14 and 17% ; for those with lower values this has varied from 23 to 25%. In normal urine without concentration HGH is barely demonstrable as have found Girard & Greenwood (1967) and Roth et al. (1967), contrary to the reports of Geller & Loh (1963) based on the less specific haemagglutination separation of bound and free. A suitable urinary concentration procedure has yet to be evolved. (1) GH levels at 1 and 2 hr after oral glucose: a test for acromegaly The serum GH levels observed in nineteen normal adults taken while at rest in bed following an oral glucose load of 40 g glucose per m2 body surface area are shown in Fig. 2. Clearly the lowest values are at 1-2 hr; the secondary postprandial rise may sometimes appear at 21 hr but not before. Evidently, if the subject has been at rest during the test, though the fasting Ilustrative cases Mean and 2 hr values Acromegaly subjects Normal 01 0lo 08 E 88 Stimuli which can increase or suppress GH secretion In normal subjects serum levels of GH increase following insulin-induced hypoglycaemia or 2-desoxyglucose, intravenous tolbutamide, stress, surgical operations, exercise, pyrogen, prolonged fasting and intravenous arginine or other amino acids. Conversely serum levels are suppressed to a minimum for the first 2 hr following a meal or a glucose load. Also, oestrogens potentiate the GH response to exercise (Frantz & Rabkin, 1965) and to arginine (Merimee, Burgess & Rabinowitz, 1966) while after cortico- a I/c_ *8 nr I I 0_ 2 Hours after oral glucose FIG. 2. Serum HGH levels during oral GTTs in normal subjects (nineteen) and acromegaly (ninety). 0, Normal subjects; 0, acromegalic patients. Downloaded from http://pmj.bmj.com/ on March 4, 2016 - Published by group.bmj.com Festschrift for Sir John McMichael level may be variable, the mean 1-2-hr levels should rarely be as high as 5 and never exceed 10 ng/ml serum. Fig. 2 also shows our findings during this test in ninety acromegalic patients. Firstly the GH levels usually did not alter significantly during the oral GTT and secondly all but one of the mean 1-2-hr levels exceeded 10 ng/ml serum. These levels varied widely within this group of acromegalics, twenty "I of whom had been given external irradiation to the pituitary; but the level did not appear to correlate with the severity or duration of the clinical syndrome, or with the age of the patient. These levels offer the best measure for assessing any treatment. After pituitary implantation with 90yttrium, serum levels are usually restored towards normal (Fig. 3). Treated (Before ond 3monthssofter-with clin. remission) Satisfactory 400 ry 70 W' 0~~~~~~~~~~~~~~ ~~I I LI: L r~~~~L~ 10 2 0 Hours (after i.v. insulin 0C1 u/kg) FIG. 4. Serum HGH during intravenous insulin tolerance test for GH reserve; in twelve normal subjects. -, Mean. (Insulin 0-1 u/kg causing hypoglycaemia under 50 mg/100 ml in each subject.) CIQ 0 50 0 0' 0 0' E ~~~~~0 ~~~~~~ c o serum (Fig. 4). The peak GH levels were closely reproducible in one normal subject (DW) on six separate tests (mean 67 ng/ml, range 53-88). NiI Partial _200- E 55 Upper onormal jimit 3- .01 (6) (12) (10) (15) No. of subjects (2) (3) FIG. 3. Serum HGH before and after 90Y treatment of acromegaly: mean 1- and 2-hr values of oral GTT, in groupings by clinical response. * Mean values at 60-120 min of oral GTT. (2) GH levels during hypoglycaemia of an ITT: a test for GH secretory capacity The GH response to the hypoglycaemia induced by insulin is a useful test for abnormalities of the hypothalamo-pituitary axis. There is often a slight initial fall in serum GH, but then a sharp rise to a peak at 60 or 90 min, whose value is usually 30-70 and always over 20 ng/ml In this test the maximal GH secretion must be stimulated, though it is less easy to define adequate hypoglycaemia for this purpose. A rapid fall of blood sugar is more effective, which an intravenous dose achieves while also offering the least hazard of prolonged hypoglycaemia. In normal subjects (Fig. 4) a standard intravenous ITT (0-1 units soluble insulin/kg body weight or 3 7 u/M2 body surface area) lowers at least one of the '-hourly blood sugar values under 50 mg/100 ml and usually induces symptoms of hypoglycaemia; we have felt that equivalent hypoglycaemia should be obtained in this test-i.e. after intravenous administration of the insulin in a dosage suited to the patient's sensitivity, at least one blood sugar should fall below 50 mg/100 ml. In subjects with either increased or decreased insulin sensitivity, the insulin dosage is varied. Subjects who are hypersensitive to insulin, for example hypopituitary subjects, are tested with half the standard dose, or those expected to be insulin resistant, for example the obese or patients with Cushing's disease or acromegaly and most diabetics, are given three times the standard dose. The adaptation of this test to diabetics (Oakley et al., 1967) has helped confirm these criteria of adequate hypoglycaemia for maximum GH stimulation. In a group of twenty-three diabetic patients with retinopathy the preliminary diabetic control was carefully adjusted to attain a near Downloaded from http://pmj.bmj.com/ on March 4, 2016 - Published by group.bmj.com Postgraduate Medical Journal 56 normal fasting blood sugar (that is under 150 if possible, or at least under 200 mg/ 100 ml), a 'Dextrostix' check of this being done before giving the intravenous insulin, usually at a dose of 03 u/kg body weight except when the blood sugar was already well under 150 mg/ 100 ml. Fig. 5(a) shows thirteen such tests on diabetics whose blood sugar fell to under 50 mg/ 100 ml. It will be seen that all these showed normal GH peaks, that is over 32 ng/ml; while in Fig. 5(b) will be seen the test results in the other ten diabetics tested whose blood sugar did not fall below 50 mg/ 100 ml, only four of whom showed normal GH peaks. It will be noted that nine of these ten had initial fasting blood sugar levels of over 200 mg/100 ml indicating the probability of inadequate hypoglycaemia within the test period. In several Blood sugar Serum HGH 200 Late GH (a) . . - ' peaks 32+--i-i'\ -IN~~~~I 0 z 20 - --- - - - 1I00 0 ~~~~~~~E / 10 501 -~ ~ ~ -t 0~~~~~~~~~~~~~~~~~~~~~B 0 0 2 0 1 2 Hoursb(afr i..i Normal :GH peak-, 32+ L--- .-- 20 T 200 '~~~ 0 - I 0 afe iv nui---01~~Hur /g FIG. 5. Serum HGH during intravenous insulin tolerance test for GH reserve. (a) In thirteen diabetics, whose blood sugar fell under 50 mg/100 ml. (b) In ten diabetics, whose blood sugar did not fall under 50 mg/100 ml. Downloaded from http://pmj.bmj.com/ on March 4, 2016 - Published by group.bmj.com 57 Festschrift for Sir John McMichael x % (Associated blood sugar) I 0 0 c E 2 0 2 0 Hours Hours FInsulin dose 0.3 u/kg pre 1 IO01 u/kg post L FIG. 6. Serum HGH during intravenous insulin tolerance test in Cushing's syndrome before and after 90Y pituitary implantation. patients considerable percentage falls in blood (exceeding 50%) occurred without inducing maximal GH secretion, though occasionally steep falls from high levels did attain this. Others (Powell et al., 1966) have suggested that a 50% blood sugar fall is a sufficient stimulus in this sugar test. We have found the test useful in assessing pituitary ablation performed to arrest diabetic retinopathy (Joplin et al., 1967); a response to a level of 5 or more ng/ml serum was found to indicate an inadequate degree of pituitary ablation. The ITT response may be abnormal in Cushing's disease (Fig. 6) indicating a subnormal secretory capacity in this disease, but not necessarily primary pituitary deficiency. Similarly in very severe obesity we have found that even with adequate hypoglycaemia from 11-1 u soluble insulin/M2, the GH peak may be subnormal, though there is usually some response. In malnutrition we find that the levels may be raised and do not tend to be lowered. (3) Urinary GH levels: a possible measurement of mean GH secretion With the variability of serum levels of GH found in all subjects except in acromegaly, it is difficult to assess the daily GH production by the pituitary. In such conditions as diabetes mellitus this may be an important factor and urinary measurements might provide a useful estimate of the mean rate of GH secretion. As yet a satisfactory concentrating procedure has to be evolved to enable the levels to be measured in normal subjects. High levels have, however, been observed in uraemia, which we have found partly depend upon the higher clearance found in uraemia. Conclusion Suitable tests are now available to reveal: (1) GH hypersecretion, and so to index the primary disorder in acromegaly (GH levels at 1-2 hr of an oral GTT), and (2) the GH secretory capacity and so potentially hypopituitary states (GH levels during adequate hypoglycaemia during an ITT). Further evolution of the assay procedure is needed to enable measurement of the usual daily GH secretory level, for which measurement of urinary levels combined with an assessment of renal function may be most helpful. Acknowledgments We are grateful to Dr R. M. Haslam and her colleagues in the Department of Chemical Pathology for the blood sugar measurements. The M.R.C. standard 'A' was kindly supplied by Dr D. R. Bangham, Division of Biological Standards, National Institute for Medical Research, London, N.W.7, and the HGH for iodination by Dr Anne S. Hartree, Department of Biochemistry, University of Cambridge. This work was supported by an M.R.C. technical grant. A.D.W. is in receipt of an M.R.C. Junior Research Fellowship. References CATT, K., NIALL, H.D. & TREGEAR, G.W. (1966) Solid phase radioimmunoassay of human growth hormone. Biochem. J. 100, 31c. COPINSCHI, G., HARTOG, M., EARLL, J.M. & HAVELL, R.J. (1967) Effect of various blood sampling procedures on serum levels of immunoreactive human growth hormone. Metabolism, 16, 402. Downloaded from http://pmj.bmj.com/ on March 4, 2016 - Published by group.bmj.com 58 Postgraduate Medical Journal DAUGHADAY, W.H. & PARKER, M.L. (1963) Sulfation factor measurement as an aid in the recognition of pituitary dwarfism. J. clin. Endocr. 23, 638. DAUGHADAY, W.H., SALMON, W.D. & ALEXANDER, J. (1959) Sulfation factor activity of sera from patients with pituitary disorders. J. clin. Endocr. 19, 743. FRANTZ, A.G. & RABKIN, M.T. (1965) Effects of oestrogen and sex differences on secretion of human growth hormone. J. clin. Endocr. 25, 1470. GELLER, J. & LOH, A. (1963) Identification and measurement of growth hormone in extracts of human urine. J. clin. Endocr. 23, 1107. GIRARD, J. & GREENWOOD, F.C. (1967) The radioimmunoassay of urine for human growth hormone. J. Endocrin. 37, xxxiv. GLICK, S.M., ROTH, J., YALOW, R.S. & BERSON, S.A. (1963) Immunoassay of human growth hormone in plasma. Nature (Lond.), 199, 784. GLICK, S.M., ROTH, J., YALOW, R.S. & BERSON, S.A. (1965) The regulation of growth hormone secretion. Rec. Prog. Hormone Res. 21, 241. GREENWOOD, F.C., HUNTER, W.M. & KLOPPER, A. (1964) Assay of human growth hormone in pregnancy at parturition and in lactation. Brit. med. J. i, 22. HARTOG, M., GAAFAR, M.A. & FRASER, T.R. (1964a) Effect of corticosteroids on serum growth hormone. Lancet, i, 376. HARTOG, M., GAAFAR, M.A., MEISSER, B. & FRASER, T.R. (1964b) Immunoassay of serum growth hormone in acromegalic patients. Brit. med. J. ii, 1229. HUNTER, W.M. & GREENWOOD, F.C. (1964) A radioimmunoelectrophoretic assay for human growth hormone. Biochem. J. 91, 43. JOPLIN, G.F., OAKLEY, N.W., HILL, D.W., KOHNER, E.M. & FRASER, T.R. (1967) Diabetic retinopathy, II. Comparison of disease remission induced by various degrees of pituitary ablation by Y90. Diabetologia (In press). KNOBIL, E. (1966) The pituitary growth hormone: an adventure in physiology. Physiologist, 9, 25. LAU, K.S., GOTTLIEB, C.W. & HERBERT, V. (1966) Preliminary report on coated charcoal immunoassay of human chorionic 'growth hormone-prolactin' and growth hormone. Proc. Soc. exp. Bio. (N. Y.), 123, 126. MERIMEE, T.J., BURGESS, J.A. & RABINOWITZ, D. (1966) Sexdetermined variation in serum insulin and growth hormone response to amino acid stimulation. J. clin. Endocr. 26, 79 1. MULLER, E.E., SAITO, T., ARIMURA, A. & SCHALLY, A.V. (1967) Hypoglycaemia, stress and growth hormone release: blockade of growth hormone release by drugs acting on the central nervous system. Endocrinology, 80, 109. OAKLEY, N.W., WRIGHT, A.D., FRASER, T.R. & HASLAM, R.M. (1967) Fasting blood-sugar and serum-growthhormone in hypopituitary diabetics. Lancet, i, 523. POWELL, E.D.U., FRANTZ, A.G., RABKIN, M.T. & FIELD, R.A. (1966) Growth hormone in relation to diabetic retinopathy. New Engl. J. Med. 275, 922. ROSSELIN, G., ASSAN, R., YALOW, R.S. & BERSON, S.A. (1966) Separation of antibody-bound and unbound peptide hormones labelled with iodine-131 by talcum powder and precipitated silica. Nature (Lond.), 212, 355. ROTH, J., GLICK, S.M., CUATRECASAS, P. & HOLLANDER, C.S. (1967) Acromegaly and other disorders of growth hormone secretion. Ann. intern. Med. 66, 760. TOUBER, J.L. & MAINGAY, D. (1963) Heterogeneity of human growth hormone. Its influence on a radioimmunoassay of the hormone in serum. Lancet, i, 1403. WELBORN, T.A. & FRASER, T.R. (1965) The double-antibody immunoassay of insulin. Diabetologia, 1, 211. Total fasting in the treatment of obesity I. C. GILLILAND Royal Postgraduate Medical School, and Prince of Wales' General Hospital, London IN AN affluent and labour-saving society energy intake often exceeds output and consequently obesity is the most frequently encountered metabolic disturbance. It is known to be associated with an increased morbidity and mortality rate. As Harrison & Harden (1966) point out, if this increased mortality rate returns to normal on losing weight (Metropolitan Life Assurance Co., 1962) then measures to lose weight must necessarily be of major therapeutic importance. Current methods of sub-caloric diet weight reduction tend to be very unsatisfactory. Stunkard & McLaren-Hume (1959) showed that out of 100 patients attending an ordinary weight-reduction clinic only two had lost weight after 2 years. Fasting was described by Folin & Denis in 1915 as 'a safe, harmless and effective method for reducing the weight of those suffering from obesity', and in the same year Benedict (1915) reviewed many previous examples of lengthy fasting as well as giving detailed observations on his own patient. Bloom (1959) revived this method of absolute starvation and much interest has since been concentrated on it. Bloom's initial periods of fasting were short, but very much longer periods have since been reported by Thomson, Runcie & Miller (1966) and Harrison & Harden (1966). We are here recording our experience with forty-six patients whose reducing regime started with a standard absolute fast for 14 days. Patients Any patient with sufficient motivation to seek Downloaded from http://pmj.bmj.com/ on March 4, 2016 - Published by group.bmj.com Standard procedures for assessing hypersecretion or secretory capacity for human growth hormone, using the radioimmunoassay. R. Fraser and A. D. Wright Postgrad Med J 1968 44: 53-58 doi: 10.1136/pgmj.44.507.53 Updated information and services can be found at: http://pmj.bmj.com/content/44/507/53.citation These include: Email alerting service Receive free email alerts when new articles cite this article. Sign up in the box at the top right corner of the online article. Notes To request permissions go to: http://group.bmj.com/group/rights-licensing/permissions To order reprints go to: http://journals.bmj.com/cgi/reprintform To subscribe to BMJ go to: http://group.bmj.com/subscribe/