Identifying
Efficacious Treatment Components
of Panic Control Treatment for Adolescents:
A Preliminary Examination
Jamie A. Micco
Molly L. Choate-Summers
Jill T. Ehrenreich
Donna B. Pincus
Sara G. Mattis
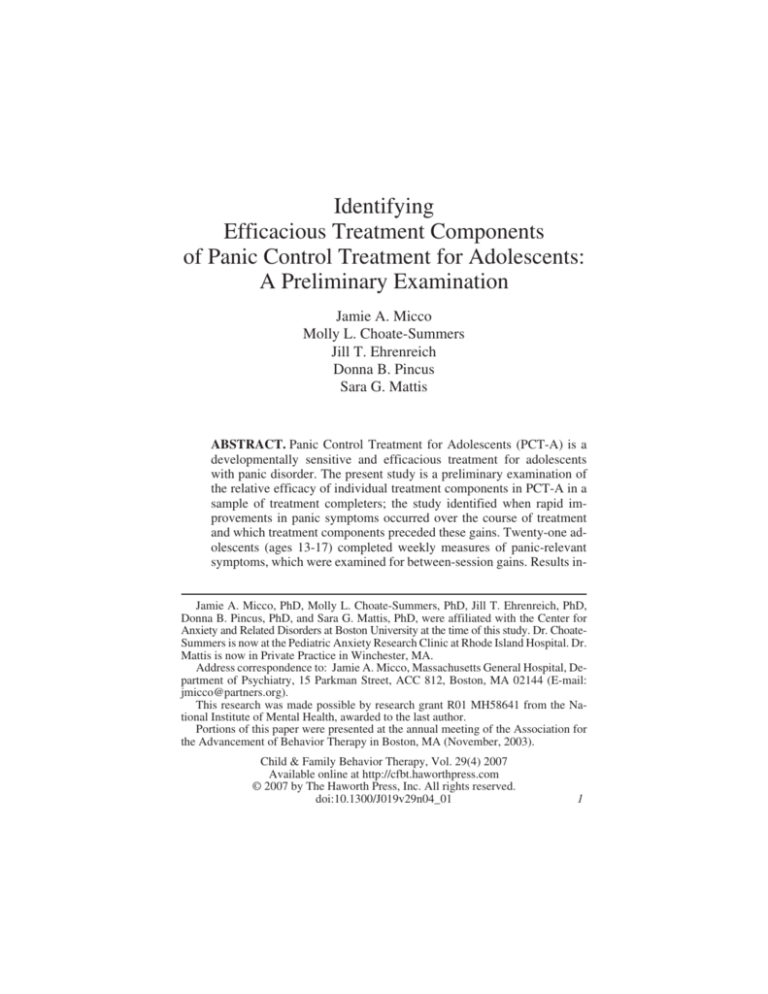
ABSTRACT. Panic Control Treatment for Adolescents (PCT-A) is a
developmentally sensitive and efficacious treatment for adolescents
with panic disorder. The present study is a preliminary examination of
the relative efficacy of individual treatment components in PCT-A in a
sample of treatment completers; the study identified when rapid improvements in panic symptoms occurred over the course of treatment
and which treatment components preceded these gains. Twenty-one adolescents (ages 13-17) completed weekly measures of panic-relevant
symptoms, which were examined for between-session gains. Results inJamie A. Micco, PhD, Molly L. Choate-Summers, PhD, Jill T. Ehrenreich, PhD,
Donna B. Pincus, PhD, and Sara G. Mattis, PhD, were affiliated with the Center for
Anxiety and Related Disorders at Boston University at the time of this study. Dr. ChoateSummers is now at the Pediatric Anxiety Research Clinic at Rhode Island Hospital. Dr.
Mattis is now in Private Practice in Winchester, MA.
Address correspondence to: Jamie A. Micco, Massachusetts General Hospital, Department of Psychiatry, 15 Parkman Street, ACC 812, Boston, MA 02144 (E-mail:
jmicco@partners.org).
This research was made possible by research grant R01 MH58641 from the National Institute of Mental Health, awarded to the last author.
Portions of this paper were presented at the annual meeting of the Association for
the Advancement of Behavior Therapy in Boston, MA (November, 2003).
Child & Family Behavior Therapy, Vol. 29(4) 2007
Available online at http://cfbt.haworthpress.com
© 2007 by The Haworth Press, Inc. All rights reserved.
doi:10.1300/J019v29n04_01
1
2
CHILD & FAMILY BEHAVIOR THERAPY
dicate that psychoeducation may precede notable decreases in panic attacks while cognitive restructuring may contribute to rapid declines in
overall anxiety and cognitive errors. The authors discuss the importance
of future controlled dismantling studies to examine the relative contribution of PCT-A treatment components. doi:10.1300/J019v29n04_01 [Article copies available for a fee from The Haworth Document Delivery Service:
1-800-HAWORTH. E-mail address: <docdelivery@haworthpress.com> Website:
<http://www.HaworthPress.com> © 2007 by The Haworth Press, Inc. All rights
reserved.]
KEYWORDS. Adolescents, panic disorder, panic control treatment,
cognitive behavioral therapy, sudden gains
PREVALENCE AND PHENOMENOLOGY OF PANIC
IN ADOLESCENT COMMUNITY
AND CLINICAL SAMPLES
The onset of panic disorder, with or without agoraphobia, occurs
most often in late adolescence (American Psychiatric Association, 2000),
although a number of community and clinical studies have found that
full-blown panic attacks and situational avoidance are also prevalent in
early to mid-adolescence. While the proportion of adolescents who endorse having experienced a panic attack varies across studies, researchers consistently find that adolescents in the community endorse having
had panic attacks both with self-report measures and clinical interviews
(Hayward, Killen, & Taylor, 1989; Hayward, Killen, & Hammer, 1992;
King, Ollendick, Mattis, Yang, & Tonge, 1996; Lau, Calamari, &
Waraczynski, 1996; Macaulay & Kleinknecht, 1989). For instance, a
large community study of 2,365 high school students (mean age = 15.4
years) found that 135 (5.7%) students reported a lifetime history of at
least one panic attack with four or more symptoms, and 62 (2.6%) reported at least one spontaneous panic attack (Hayward, Killen,
Kraemer, & Taylor, 2000). Prevalence estimates of panic disorder in
adolescence range from 0.5% (Hayward, Killen, & Taylor, 2003) to
1.6% (Reed & Wittchen, 1998) in community samples.
In clinical samples, panic disorder is clearly a clinically relevant
problem, with estimates ranging from 6% (in a pediatric psychopharmacology clinic; Biederman et al., 1997) to approximately 10% (in
both an anxiety disorders clinic and an Italian outpatient clinic; Last &
Micco et al.
3
Strauss, 1989; Masi, Favilla, Mucci, & Millepiedi, 2000) of referred
children and adolescents meet criteria for the disorder. Additionally,
compared to psychiatric and non-clinical control groups, adolescents
who meet criteria for panic and/or agoraphobia have elevated comorbidity with depression and other anxiety disorders (Biederman et al.,
1997), and they report higher anxiety sensitivity compared to a clinical
control sample of children without panic disorder (Kearney et al.,
1997). This underscores the importance of developing efficacious treatments for children and adolescents who experience panic attacks and
panic disorder.
PANIC CONTROL TREATMENT
FOR PANIC DISORDER AND AGORAPHOBIA
A number of studies have established the efficacy of cognitive-behavioral treatments (CBT) for adults with panic disorder and agoraphobia (Clark, 1989; Clark, Salkavakis, Hackmann, Middleton, Anastasiades, & Gelder, 1994; Telch, Schmidt, Jaimez, & Harrington, 1995).
Panic Control Treatment (PCT) is one such cognitive-behavioral treatment developed by Barlow and Craske (2000) in the mid-1980s. PCT
has been found to be superior to progressive muscle relaxation and
waitlist control groups at both post-treatment and follow-up (Barlow,
Craske, Cerny, & Klosko, 1989; Craske, Brown, & Barlow, 1991), and
it appears to have a more durable effect at follow-up than tricyclic
medication for panic-disordered patients (Barlow, Gorman, Shear, &
Woods, 2000).
Ollendick (1995) conducted the first controlled study of CBT for
panic-disordered adolescents, which employed a multiple-baseline design with four participants (ages 13 to 17). The treatment contained
components of PCT, but also included progressive muscle relaxation
and situational exposure. At post-treatment, all adolescents reported a
reduction in the frequency of panic attacks, less situational avoidance,
and lower scores on self-report questionnaires of anxiety sensitivity,
fear, and overall anxiety (Ollendick, 1995).
Given the efficacy of PCT with panic-disordered adults, as well as
Ollendick’s finding that CBT can be successfully applied to adolescents
with panic disorder, Mattis and colleagues (Hoffman & Mattis, 2000;
Mattis & Ollendick, 2002) developed a developmentally sensitive adaptation of the PCT protocol for adolescents. Panic Control Treatment for
Adolescents (PCT-A) shares its predecessor’s focus on three main as-
4
CHILD & FAMILY BEHAVIOR THERAPY
pects of panic disorder. Specifically, PCT-A targets: (1) the cognitive,
or misinterpretational, aspect, (2) the hyperventilatory response, and (3)
conditioned reactions to physical sensations. However, several changes
in the protocol were made so that it would be more appropriate for use
with adolescents. These changes include clearer, simplified language
(particularly during the psychoeducational component of the manual)
and visual and verbal examples of important concepts. Situational exposure was also added to the PCT-A manual, given the high frequency
of agoraphobic avoidance in panic-disordered adolescents (Biederman
et al., 1997; Kearney et al., 1997).
Results of a recent, randomized controlled trial of PCT-A support the
efficacy of the treatment protocol with adolescents who have been diagnosed with panic disorder and agoraphobia (Mattis, Cohen, Hoffman,
Pincus, Choate, & Micco, 2001; Mattis & Pincus, 2003; Mattis, Pincus,
Ehrenreich, & Barlow, 2006). Compared to adolescents randomly assigned to a waitlist control group and assessed post-waitlist, adolescents
assigned to the treatment group showed significantly greater improvements on clinician severity ratings of panic disorder, the Multidimensional Anxiety Scale for Children (MASC; March, 1997), and the
Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds &
Richmond, 1978) at post-treatment assessment (Mattis et al., 2006),
among other measures (see Mattis et al., 2006, for a full review of the
study’s findings).
TREATMENT COMPONENTS OF PCT-A:
DESCRIPTION AND RATIONALE
PCT-A consists of 11 individual treatment sessions that are 60-90 minutes in length. There are seven main treatment components of PCT-A,
which are described in Table 1. Breathing retraining is introduced in session three, following psychoeducation (session one) and situation exposure (session two). The inclusion of breathing retraining is based on the
hyperventilation model of panic disorder, which holds that subtle,
chronic hyperventilation (or overbreathing) in people with panic disorder
leads to physical symptoms that, when noticed, can spiral into a
full-blown panic attack (Ley, 1985). In support of this model, studies
have shown that people with panic disorder have lower basal pCO2 levels
(Roth, Wilhelm, & Trabert, 1998; Papp et al., 1997) and greater subjective response to voluntary hyperventilation (Rapee, Brown, Antony, &
Barlow, 1992). Breathing retraining is intended to correct the patient’s
Micco et al.
5
TABLE 1. Treatment Components Included in PCT-A
Treatment Component
Session(s)
Introduced
Description
1-2
Therapist provides accurate information about
feared physical sensations in the context of
the body’s fight/flight system and describes
and discusses the “cycle of panic”
Situational Exposure (SE)
2
Fear and Avoidance Hierarchy is developed;
therapist emphasizes that remaining in feared
situations will lead to habituation in
panic-related symptoms; exposure from FAH
is assigned at each session
Breathing Retraining (BR)
3-4
Adolescent is taught to breathe slowly from
the diaphragm and practices twice daily at
home
Cognitive Restructuring (CR)
4-5
Described as “thinking like a detective”;
adolescent learns to identify automatic
thoughts, including probability overestimation
and catastrophic thinking, and is taught to
challenge thoughts by looking at the evidence
and generating rational responses
Interoceptive Exposure (IE)
5-6
Adolescent is desensitized to panic-like
physical sensations through a series of
exercises designed to elicit these sensations,
such as spinning in a chair, breathing through
a straw, and hyperventilating; exercises are
repeatedly practiced in several settings until
the sensations do not elicit anxiety
Hypothesis Testing
7
Adolescent makes predictions regarding the
outcome of a feared situation, engages in the
situation, and evaluates his/her original
prediction
Naturalistic Interoceptive
Exposure
8
Adolescent engages in situations in everyday
life that elicit physical sensations (i.e.,
drinking caffeine, exercising, going on a roller
coaster)
Psychoeducation
tendency towards subtle hyperventilation, and thus decrease physical
sensations that predispose the patient to experience a panic attack.
The rationale for including cognitive restructuring and hypothesis
testing in PCT-A is based on Clark’s (1988) cognitive model of panic,
which holds that catastrophic misinterpretation of normal physiological
anxiety reactions result in panic attacks. Indeed, adult patients with
panic disorder are more likely than patients with other anxiety disorders
and adults with no psychiatric disorder to interpret ambiguous physical
sensations as something being physically or mentally wrong with them
(Clark et al., 1997). Cognitive restructuring addresses this misinter-
6
CHILD & FAMILY BEHAVIOR THERAPY
pretational aspect of panic disorder, as does hypothesis testing (behavioral experiments that test the accuracy of panic-related cognitions).
Children and adolescents with panic disorder and panic attacks are
more likely to experience anxiety sensitivity, or hypervigilance and fear
of physiological sensations than children and adolescents without panic
disorder or panic attacks (Calamari et al., 2001; Ginsburg & Drake,
2002; Kearney et al., 1997; Weems, Hayward, Killen, & Taylor, 2002).
Thus, helping adolescents with panic disorder become less fearful and
vigilant of normal physiological sensations appears to be an important
treatment goal, and this is the purpose of interoceptive exposure.
Although PCT-A is primarily an individual treatment, parents are included in the last 10 minutes of sessions one, four, seven, and 11 of
PCT-A. Given that parents are integrally involved in their adolescents’
lives, it is expected that including them as part of therapy will result in
greater reinforcement of the use of cognitive-behavioral skills at home,
although more research is necessary to determine if this is the case
(Barrett, 2000).
IDENTIFYING EFFICACIOUS
TREATMENT COMPONENTS OF PCT
Examination of Specific Treatment Components of PCT in Adults
Identifying components of a treatment that most effectively lead to
symptom reduction allows researchers to “fine tune” the treatment manuals
they develop and clinicians to spend more time on aspects of treatment that
seem to work. There are a number of studies that have examined the efficacy of specific cognitive-behavioral treatment components for adults with
panic disorder, many of which have compared interoceptive exposure (IE)
to other treatment components (Arntz, 2002; Bouchard et al., 1996; Craske,
Rowe, Lewin, & Noriega-Dimitri, 1997; Hecker, Fink, Vogeltanz, Thorpe,
& Sigmon, 1998; Ito, Noshirvani, Basoglu, & Marks, 1996). For instance,
Hecker and colleagues (1998) provided 18 patients with panic disorder
with four sessions of cognitive therapy (CT) and four sessions of IE; half of
the patients got CT first, and half got IE first. Results show that both treatments led to similar clinical improvements, with the only difference being
lower self-ratings of global disturbance in the CT-first group. The order of
the treatment components did not influence outcome, as most patients
made clinically significant treatment gains during the first half of treatment
and maintained them during the second half (Hecker et al., 1998). Another
Micco et al.
7
study randomly assigned 26 patients with panic disorder and agoraphobia
to 10 weekly sessions of IE plus situational exposure (SE) or SE alone; neither treatment condition included CT (Ito et al., 1996). There were few differences in treatment outcome between the two groups, although more
patients who had both IE and SE improved greater than 50% on measures
of apprehension and agoraphobia (Ito et al., 1996).
Craske et al. (1997) compared IE to breathing retraining (BR) in a
group of 38 adults with panic disorder and agoraphobia. All patients
were treated using cognitive restructuring and SE, but half also received
IE while the other half received BR. While both treatment packages
were equally effective on a number of panic-relevant measures, those
who had received IE (compared to those who received BR) had fewer
panic attacks and lower overall severity at post-treatment and fewer
panic attacks and phobic fears at six-month follow-up (Craske et al.,
1997). Schmidt and colleagues (2000) found that adults with panic disorder and agoraphobia who received BR in combination with SE tended
to have lower end-state functioning at a follow-up assessment when
compared to adults who received SE without BR. The authors suggest
that this finding may be due to patients using deep breathing in an attempt to avoid panicky physical sensations during panic attacks
(Schmidt et al., 2000).
In sum, studies that have compared the efficacy of specific treatment
components that are included in PCT for adults have found few differences in overall outcome on panic-relevant measures, including panic
attack frequency, apprehension of panic, and agoraphobic avoidance,
although there is some evidence for the efficacy of IE and SE having an
advantage over that of BR in treatment outcome, particularly at follow-up. To date, however, no study has looked at specific treatment
components of panic control treatment in children and adolescents.
“Sudden Gains” Treatment Studies
One way of examining the contribution of individual treatment components to overall improvement is to look at between-session treatment
changes. If an abrupt reduction in symptoms occurs following a specific
session, a treatment component addressed in that session may have contributed to overall improvement. Tang and DeRubeis (1999) examined
between-session changes for adults receiving CBT for depression,
particularly looking for abrupt changes from one session to the next, or
“sudden gains” in treatment. The researchers found that significant
cognitive changes (as measured by a clinician rating scale) tended to
8
CHILD & FAMILY BEHAVIOR THERAPY
precede sudden gains on the Beck Depression Inventory (Tang &
DeRubeis, 1999). Pham and colleagues (2004) found similar results in
their analysis of sudden gains on the Anxiety Sensitivity Index (ASI)
for adults receiving CBT for panic disorder. Specifically, patients who
made sudden gains had significantly lower anxiety sensitivity at
post-treatment compared to patients who did not make sudden gains
(Pham, Tang, Zinbarg, & Andrusyna, 2004). Thus, analysis of between-session treatment change may contribute to an understanding of
the contribution of treatment components and have an impact on treatment outcome.
AIMS OF THE PRESENT STUDY
Given that a sizeable number of adolescents and children present to
clinical settings with panic disorder and agoraphobia or sub-syndromal
panic disorder, it is important to evaluate the efficacy of treatments provided to this population. While PCT-A appears to be an efficacious
treatment for panic-disordered adolescents, it is unclear which components of the protocol actively contribute to the treatment’s efficacy.
There have been a number of studies examining the relative efficacy of
specific CBT components for adults with panic disorder but not for adolescents. The purpose of the present study is to conduct a preliminary
examination of panic-related symptom changes in relation to the introduction of different treatment components of PCT-A, using sudden
gains analysis. However, in contrast to Tang and DeRubeis (1999), who
compared individuals who made sudden gains to those who did not, the
purpose of the present study is to identify when adolescents with panic
disorder as a group experienced significant improvements in panic-related symptoms over the course of PCT-A. More specifically, we
sought to generate hypotheses about the relative efficacy of the treatment components of PCT-A by determining which treatment components of PCT-A were followed by sudden treatment gains.
METHODS
Participants
The data used in the present analysis were drawn from a randomized,
controlled trial of PCT-A at an outpatient anxiety disorders clinic. The
study included 21 adolescents (18 girls, three boys; mean age = 15.38,
Micco et al.
9
SD = 1.16) who completed the treatment in its entirety. All adolescents,
ages 13 to 17, who were principally diagnosed with panic disorder (with
or without agoraphobia) at intake via the Anxiety Disorders Interview
Schedule, Child/Parent Version (ADIS-IV-C/P; Silverman & Albano,
1996) between 1998 and 2002 were offered participation in the project.
Exclusion criteria included diagnosis of a psychotic disorder, pervasive
developmental disorder, mental retardation, and current suicidal ideation. Adolescents taking psychiatric medication were required to take
the same dose of the medication for at least one month (for anti-anxiety
medications) or three months (for anti-depressant medications) prior
to participation in the project and remain on the same dose of medication until the end of their participation in the study. Of those who were
offered the project, 80% agreed to participate; the primary reason for
adolescents choosing not to participate was not wanting to wait for
treatment should they be randomized to the waitlist condition of the
study.
Adolescents who were eligible and agreed to participate in the project reviewed and signed informed consent and assent forms, along with
their parents, after which they were randomly assigned to either the
treatment or waitlist condition. The latter involved bi-weekly, 30-minutes “check-in” sessions over the course of eight weeks, during which
adolescents established rapport with their therapist and described any
panic-related symptoms they experienced over the course of the intervening two weeks. Other than the completion of weekly monitoring
forms, waitlist sessions did not include any cognitive-behavioral treatment components. After the completion of the waitlist period, adolescents in this group received a full-course of PCT-A. Therapists included
doctoral students in clinical psychology and doctoral-level psychologists. All sessions were videotaped, and 32.5% of the sessions were randomly selected and reviewed for treatment integrity by either a
bachelor’s level research assistant or doctoral student. All session components were rated on a scale from 1 (not at all covered in session) to 5
(completely and thoroughly covered in session) and then averaged to
create one treatment adherence rating for the entire session. The average
treatment adherence across sessions in this study was 4.57 (SD = .37).
Ten girls and two boys from the immediate treatment group completed all the measures of interest to the present study. Two additional
adolescents, one girl and one boy, dropped out of treatment after session
eight and are not included in the analyses below. Of the waitlist group,
eight girls and one boy who chose to participate in treatment after completing the waitlist period also completed all study measures; two girls
10
CHILD & FAMILY BEHAVIOR THERAPY
and one boy chose not to participate in treatment after completing the
waitlist period. As the waitlist group did not differ from the immediate
treatment group prior to treatment initiation on measures of anxiety,
panic disorder, depression, or anxiety sensitivity (Mattis et al., 2006),
both groups were combined to analyze their treatment sessions. Thus,
21 adolescents are included in the present study.
Despite efforts to recruit a more ethnically diverse sample, all participants in the study were Caucasian. Most of the adolescents’ parents
were married (90%), while 10% were divorced or separated. The modal
level of education for both parents was a bachelor’s degree. Of the 21
participants, 19 were diagnosed with panic disorder with agoraphobia at
the initial assessment, while two were diagnosed with panic disorder
without agoraphobia. The mean clinician severity rating of panic disorder, based on the ADIS-IV-C/P (zero to eight, with a CSR of four and
higher representing a clinical level of severity), was 5.52. Most of the
participants (85.7%) had at least one additional clinical anxiety or mood
disorder; the mean number of additional diagnoses was 1.71.
Measures
Weekly Measures
Weekly Record of Anxiety and Depression (WRAD). The WRAD is a
monitoring form on which adolescents recorded their daily levels of average anxiety, depression, and pleasantness on a zero (not at all) to eight
(very much) scale. In a study of younger children (grades 3-6), the use
of a daily self-monitoring form to record anxiety symptoms was found
to be reliable, and the form differentiated test-anxious from non-testanxious children (Beidel, Neal, & Lederer, 1991). Adolescents in the
present study brought the WRAD to session each week and reviewed it
with their therapist. The present study used the “average anxiety” component of the WRAD. We averaged the adolescents’ daily anxiety ratings for each week, which yielded one average anxiety rating per
session.
Panic Attack Record (PAR). Adolescents monitored the frequency
and qualitative aspects of panic attacks over the course of the week on
the PAR, a self-monitoring form initially developed for adults by
Rapee, Craske, and Barlow (1990). Adolescents were instructed to use
one form per panic attack and to record the duration of the attack, maximum anxiety level, possible antecedents, and symptoms. In a largely
college-aged sample, Nelson and Clum (2002) found that the frequency
Micco et al.
11
of panic attacks over a two-week period as measured by the PAR correlated highly (r = .89) with the frequency as measured by a Panic Attack
Frequency Calendar. From the PAR, we calculated the average number
of unexpected, full-blown panic attacks (i.e., with four or more physical
or cognitive symptoms) adolescents experienced in the week prior to
each session of PCT-A.
Weekly Measure After Session 5
Belief Ratings. Belief ratings measured the degree to which adolescents engaged in “probability overestimation” and “catastrophic thinking.” Probability overestimation is the tendency to think that events are
more likely to occur than evidence would suggest. Catastrophic thinking is the tendency to believe that the consequences of a feared outcome
would be horrible and too difficult to handle. At session five, adolescents identified their most anxiety-provoking probability overestimation and rated the likelihood that the thought would come true (0 = not at
all likely to 100 = very likely). In addition, adolescents identified their
worst catastrophic thought and rated their ability to cope if the feared
outcome actually occurred (0 = very poorly to 100 = very well). At every session after session five, adolescents re-rated these two beliefs.
Measure Collected at Session 11
Perceptions of Treatment Questionnaire (PTQ). The PTQ is a
self-report questionnaire, designed for the purposes of the PCT-A
study, which includes both forced-choice and free-response questions.
This measure assesses the aspects of treatment that adolescents did and
did not find to be helpful, such as specific treatment components and
therapist alliance. For the purposes of the present study, we only examined adolescents’ responses to the free-response PTQ question, “What
was most helpful about the treatment?”
Data Analysis
Sudden gains, or treatment improvements, using group averages for
each measure were analyzed for each of the three weekly measures. If
an adolescent did not complete a measure for a particular session, it was
not replaced with an individual average and instead dropped from the
calculated group average for that particular session. Although sudden
gains have previously been examined across individuals completing
12
CHILD & FAMILY BEHAVIOR THERAPY
treatment for depression (Tang & DeRubeis, 1999; Stiles et al., 2003),
there is no precedent for examining sudden gains from session-to-session across group averages. Thus, for each measure, we defined the first
criterion for a sudden gain as a between-session change score of at least
two standard deviations from the mean of all between-session changes
across the 11 sessions. This “two standard deviation” criterion ensured
that sudden gains were large relative to overall changes. In addition,
similar to criteria established in Tang and DeRubeis’ (1999) study, sudden gains had to represent at least 25% of the pre-gain session’s WRAD
score, panic attack frequency, or belief rating. Furthermore, to ensure
that the improvement was stable, the mean scores across the three sessions before the sudden gain had to be significantly higher than the
mean scores across the three sessions after the gain (when applicable),
using a t-test with an alpha of 0.05. Finally, we examined the PTQ to
determine which treatment component adolescents perceived to be
most helpful during PCT-A.
RESULTS
Sudden Gains on WRAD, PAR, and Belief Ratings
The mean “average anxiety” score on the WRAD, as rated by the adolescents on a scale from zero to eight, was 2.90 (SD = 1.70) at pretreatment and 1.20 (SD = 1.77) at session 11. The average between-session change across all sessions on the WRAD-Average Anxiety was a
decrease of 0.15 units (SD = 0.33; range = ⫺0.40-0.70). Thus, a between-session change on the WRAD had to exceed 0.66 to meet the two
SD criterion as a sudden gain. The mean decrease in average anxiety between sessions four and five was 0.70, which met the first criterion.
This gain was also greater than 25% of the previous session’s mean average anxiety rating of 0.30 (0.30 ⫻ 0.25 = 0.08). In addition, the mean
average anxiety rating for the three sessions preceding the sudden gain
(2.87) was significantly greater than that of the three sessions after the
sudden gain (2.27; t = 10.39, p = 0.01). This significant improvement in
average anxiety notably occurred after the introduction of cognitive restructuring in the treatment protocol. No additional between-session
changes in average anxiety met sudden gain criteria (see Figure 1).
Adolescents experienced an average of 2.63 (SD = 3.50) panic attacks a week at pre-treatment, which decreased to 0.31 (SD = 0.58) at
session 11. The average between-session decrease in number of
Micco et al.
13
FIGURE 1. Mean change in average anxiety, as measured by the WRAD,
across treatment sessions.
3.5
Average Anxiety (0-8)
3
2.5
2
1.5
1
0.5
0
Pre
1
2
3
4
5
6
Session
7
8
9
10
11
full-blown panic attacks (as measured by the PAR) was 0.26 (SD =
0.50; range = ⫺0.25-1.50). In order to be considered a “sudden gain,” a
between-session change in frequency of panic attacks would have to exceed 1.00. One between-session change met this criterion: the average
decrease in panic attacks between sessions one and two (after the first
session of psychoeducation) was 1.50 (see Figure 2). This between-session change met the second criterion to be considered a “sudden gain”;
it was greater than at least 25% of the previous session’s panic attack
frequency of 2.88 (2.88 ⫻ 0.25 = 0.72). However, although the mean
number of panic attacks of the two sessions before the sudden gain
(pre-treatment and session one; mean = 2.76) was greater than the mean
frequency of attacks in the three sessions after the sudden gain (1.53),
this difference is not statistically significant. Thus, the decrease in panic
attacks between sessions one and two cannot be considered a full sudden gain. No other between-session changes on the PAR met the sudden
gain criteria.
Adolescents’ belief in their most salient probability overestimation
dropped from a mean belief rating of 49.00 (SD = 35.12) at session five
to 13.05 (SD = 25.73) at session 11. The mean between-session decrease in adolescents’ belief ratings was 5.99 percentage points (SD =
14
CHILD & FAMILY BEHAVIOR THERAPY
FIGURE 2. Mean change in panic attack frequency, as measured by the PAR,
across treatment sessions.
Average # of Weekly Panic Attacks
3.5
3
2.5
2
1.5
1
0.5
0
Pre
1
2
3
4
5
6
Session
7
8
9
10
11
6.59; range = 0.55-18.83). One between-session change was greater
than two standard deviations from the mean (13.18); between sessions
five and six, the average decrease in adolescents’ belief ratings was
18.83. Because belief ratings were recorded beginning at session five,
the change between sessions five and six cannot be compared to belief
ratings at earlier sessions. However, the belief rating at session five
(49.00) is higher than the average belief rating of the three sessions following the sudden gain (26.15). This sudden change in probability
overestimation belief came after the second session of cognitive restructuring (see Figure 3). At the individual level, eight out of 21 participants (38.1%) experienced a rapid decrease in their belief ratings
between sessions five and six (i.e., a decrease that exceeded two standard deviations from the individual’s mean change in belief ratings
from sessions five through 11).
Adolescent’s coping ratings (i.e., belief in how well they could cope
if a feared outcome did occur) increased from an average of 56.57 (SD =
30.70) at session five to 78.14 (SD = 29.56) at session 11. The mean between-session increase in coping ratings was 3.60 percentage points
(SD = 3.44; range = ⫺1.20-9.48). The average increase in coping ratings between sessions five and six was 9.48, which is higher than two
Micco et al.
15
FIGURE 3. Mean change in probability overestimation belief ratings and catastrophic cognition coping ratings across treatment sessions.
90
80
70
60
50
Belief Rating
Coping Rating
40
30
20
10
0
5
6
7
8
9
10
11
Session
standard deviations from the mean (6.88). The mean coping rating at
session five (56.57) is lower than the average coping ratings at the two
sessions following the sudden gain (69.59). Of the 21 participants,
seven (33.3%) experienced an individual marked increase in their coping ratings (i.e., greater than two standard deviations from their individual mean change in coping ratings from sessions five to 11). No other
between-session changes in coping ratings met criteria to be considered
a sudden gain (see Figure 3).
Adolescents’ Perceptions of Treatment
Adolescent participants were asked to give a free response to the following question on the PTQ: “What was most helpful about the treatment?” Of the 19 participants who completed the PTQ, seven (36.8%)
described cognitive restructuring as most helpful, while six (31.6%) felt
the psychoeducational component of treatment was most helpful. Three
(15.8%) listed breathing retraining and two (10.5%) listed situational
exposure. One participant (5.3%) said that she found “having someone
to talk to” was most helpful to her.
16
CHILD & FAMILY BEHAVIOR THERAPY
DISCUSSION
The present study is a preliminary examination of the relative efficacy of PCT-A treatment components with the aim of generating hypotheses for additional controlled studies of this treatment. Our results
suggest that over the course of PCT-A, adolescents experienced periods
of rapid improvement in panic-relevant symptoms. At pre-treatment,
adolescents in this study experienced an average of 2.63 panic attacks
per week, which is higher than the average weekly frequency of 0.92
experienced by “severe” non-clinical adolescent panickers (calculated
from the three-week frequency of panic attacks), as reported by
Macaulay and Kleinknecht (1989). After adolescents in the present
study received their first session of treatment, they experienced an average of one-and-a-half fewer unexpected, full-blown panic attacks than
they did the previous week. Although this decrease did not meet our
third criterion to be termed a “sudden gain” (likely the result of only
having only two sessions pre-gain on which to conduct the t-test), adolescents continued to experience fewer than two panic attacks per week
on average after session one, an improvement that is clinically meaningful. While this decrease in frequency of panic attacks may well be
the result of relief from initiating treatment, it is also possible that the
decrease is related to the first session of psychoeducation regarding
anxiety and panic, which emphasizes the interrelationship between
thoughts, physical sensations, and avoidance. Between sessions one
and two, each adolescent evaluated his/her own panic attacks in the context of the “cycle of panic” they learned at the first session. They were
also oriented to the treatment model by their therapist, which likely
resulted in an expectation of greater control over panic symptoms; this
sense of control, in turn, may have led to a decrease in panic attacks.
Adolescents also experienced improvement in their ratings of average anxiety between sessions four and five, as measured by the WRAD.
This sudden gain occurred after the first session of cognitive restructuring (CR), during which adolescents learn how to gather evidence
against and challenge probability overestimations. Similarly, there
were significant cognitive improvements between sessions five and six
on two variables: how much adolescents believed their most salient
probability overestimation was true, and how confident they were in
their ability to deal with feared outcomes. These improvements occurred after the second session of CR, during which adolescents identify catastrophic cognitions and determine ways that they could cope
with feared outcomes if they actually occurred.
Micco et al.
17
Thus, it appears that psychoeducation and CR are two treatment
components after which sudden symptom improvements were observed, although further studies are essential to determining if these are
indeed active treatment ingredients. Interestingly, these were the same
two treatment components that adolescents reported as being most helpful to them on the PTQ. However, given the limitations of our data, it is
difficult to determine if each treatment component led to improvement
in the specific symptom of panic disorder it intended to target, mainly
because of the overlap in the presentation of different treatment components. Nevertheless, our impression is that CR appeared to precede a
significant decrease in intensity of cognitive errors, as measured by the
belief and coping ratings, suggesting that there is specificity to this
treatment component. On the other hand, BR and IE did not result in
sudden decreases in panic attacks as would be expected, although the
frequency of panic attacks continued to decline steadily after both
treatment components were fully introduced.
There are a number of limitations of this study that prevent us from
drawing definitive conclusions about the relative importance of each
treatment component. First, because of the overlap in the presentation
of treatment components (for example, clients are still working on BR
when they begin CR) and the lack of a control group, we cannot say
with certainty that the sudden gains we found were the direct result of
one particular treatment component. It was especially difficult to examine what effect SE had on the adolescents’ symptoms of panic and agoraphobia because this component was an active part of every session
beginning at session two and because the measure of avoidance in the
overarching study (the Fear and Avoidance Hierarchy) was not collected weekly over the course of the protocol. Also, while we can say
that there was a sustained decrease in cognitive errors on the belief rating measure after session five, we cannot be certain that there were no
changes in adolescents’ belief ratings before the introduction of CR, as
this measure was not collected before session five (it was originally
conceived as a treatment tool).
A second limitation is the small sample size of 21 adolescents, all of
whom were Caucasian. Most of the adolescents came from intact families and had well-educated parents. These characteristics of our sample
may limit the generalizability of the findings to other populations. In addition, all participants in the present study were treatment completers;
we may have found that some treatment components were less effective
if participants who did not complete the full treatment had been included in the analyses. A third limitation is that there is no standard defi-
18
CHILD & FAMILY BEHAVIOR THERAPY
nition of a “sudden gain” across group averages on a measure; the
definition that we used was modeled after that of Tang and DeRubeis
(1999), who looked at individual sudden gains, but our criterion that
sudden gains had to be larger than two standard deviations from the
mean on each measure was somewhat arbitrary, selected to ensure that
the sudden gains we found were large compared to changes across treatment. However, this criterion may have missed between-session
changes that fell short of the two standard deviation criterion but were
still clinically significant. For future studies examining session-by-session changes, a standard definition of a mean “sudden gain” should be
established so that the criteria are not reinvented with each study, which
limits uniform interpretation of the results. Treatment outcome researchers seeking an established but conservative definition of sudden
treatment gains may wish to employ the sudden gains criteria used in
the present study.
Finally, despite the fact that daily self-monitoring of anxiety and
panic attack records are widely used in cognitive-behavioral treatment
for anxiety, there have been few studies of their psychometric properties and none of the two measures designed particularly for the study of
PCT-A’s efficacy (the belief ratings and the PTQ). Nevertheless, it has
been shown that even children younger than the adolescents in this
study can reliably complete self-monitoring forms of anxiety symptoms
(Beidel et al., 1991). Furthermore, the portion of the PTQ used in the
present study for a qualitative analysis of what adolescents thought was
most helpful during treatment was intended as a supplement to their
quantitative ratings. However, future studies of cognitive-behavioral
treatment components may wish to include well-validated self-report
measures that are collected on a weekly basis in addition to weekly
self-monitoring and in-session belief ratings.
While a number of controlled studies comparing CBT ingredients
for panic disorder have been conducted with adults (i.e., Craske et al.,
1997; Hecker et al., 1998), there have been no studies for CBT of adolescent panic, and very few studies in the child CBT literature in general, that have looked at the contribution of individual treatment
components to a treatment manual as a whole. In a discussion of mechanisms of change in cognitive-behavioral treatments for anxious children and adolescents, Hudson (2005) stresses the importance of future
research examining the differential efficacy of individual treatment
components. Along these lines, we recommend that the “active ingredients” of PCT-A be examined more closely through controlled dismantling studies. For example, the efficacy of SE in PCT-A can be
Micco et al.
19
established by comparing panic-disordered adolescents who receive
standard PCT-A to those who participate in PCT-A without the inclusion of SE.
The degree to which BR contributes to the overall efficacy of PCT-A
is of particular interest in light of Schmidt and colleagues (2000) finding that this treatment component may put adults with panic disorder at
risk for relapse, and Craske et al.’s (1997) finding that IE is superior to
BR. Meuret, Wilhelm, Ritz, and Roth (2003) suggest that at this point,
arguments for or against the inclusion of BR in treatment for panic disorder are premature given the significant variability in studies that have
examined this treatment component (i.e., type of BR used, patient selection, study design). The authors argue that BR appears to correct
maladaptive breathing patterns that increase vulnerability to panic attacks and that further research is necessary to clarify the role of BR in
the treatment of panic disorder (Meuret et al., 2003).
In addition, given our finding that psychoeducation may have contributed to a significant reduction in average frequency of panic attacks,
future research might examine if psychoeducation alone leads to the
prevention of panic disorder and agoraphobia in adolescents at risk for
developing the disorder, such as adolescents who have parents with
panic disorder or adolescents who have previously experienced limited-symptom panic attacks.
CONCLUSION
The fact that as many as 10% of children and adolescents presenting
to outpatient clinics meet criteria for panic disorder emphasizes the importance of developing and honing efficacious treatments for this population. Evidence suggests that PCT-A results in significant treatment
improvements in adolescents with panic disorder and agoraphobia
(Mattis et al., 1996), although which components of this treatment contribute to its efficacy remain to be seen. Our session-by-session analysis
of treatment gains on panic-relevant measures suggests that psychoeducation may contribute to a reduction in the frequency of panic attacks, while cognitive restructuring appears to play a role in decreasing
adolescents’ self-report of overall anxiety and the degree to which adolescents engage in cognitive errors. As clinical researchers develop increasingly helpful treatments for childhood anxiety disorders, it is
particularly important to obtain more definitive evidence of the treatment components (individually and/or in combination) that are neces-
20
CHILD & FAMILY BEHAVIOR THERAPY
sary and sufficient to produce lasting treatment gains. Thus, we
recommend that future research extend our findings by further elucidating the role of each treatment component of PCT-A in reducing adolescents’ panic symptoms.
REFERENCES
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental
disorders (4th ed., text revision). Washington, DC: Author.
Arntz, A. (2002). Cognitive therapy versus interoceptive exposure as treatment of panic
disorder without agoraphobia. Behaviour Research and Therapy, 40, 325- 341.
Barlow, D.H. & Craske, M.G. (2000). Mastery of your anxiety and panic: Client Workbook for anxiety and panic. San Antonio, TX: Graywind Psychological Corporation.
Barlow, D.H., Craske, M.G., Cerny, J.A., & Klosko, J.S. (1989). Behavioral treatment
of panic disorder. Behavior Therapy, 20, 1-26.
Barlow, D.H., Gorman, J.M., Shear, M.K., & Woods, S.W. (2000). Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized
control trial. Journal of the American Medical Association, 283, 2529-2536. doi:
0.1001/jama.283.19.2529
Barrett, P.M. (2000). Treatment of childhood anxiety: Developmental aspects. Clinical
Psychology Review, 20, 479-494. doi: 10.1016/S0272-7358(99)00038-0
Beidel, D.C., Neal, Angela, M., & Lederer, A.S. (1991). The feasibility and validity of
a daily diary for the assessment of anxiety in children. Behavior Therapy, 22,
505-517. doi:10.1016/S0005-7894(05)80342-9
Biederman, J., Faraone, D.V., Marrs, A., Moore, P., Garcia, J., Ablon, S., Mick,
E., Gershon, J., & Kearns, M.E. (1997). Panic disorder and agoraphobia in consecutively referred children and adolescents. Journal of the American Academy
of Child and Adolescent Psychiatry, 36, 214-223. doi: 10.1097/00004583199702000-00012
Bouchard, S., Gauthier, J., Laberge, B., French, D., Pelletier, M., & Godbout, C.
(1996). Exposure versus cognitive restructuring in the treatment of panic disorder
with agoraphobia. Behaviour Research and Therapy, 34, 213-224. doi: 10.1016/
0005-7967(95)00077-1
Calamari, J.E., Hale, L.R., Heffelfinger, S.K., Janeck, A.S., Lau, J.J., Weerts,
M.A., Taglione, P.A., & Schisler, R.L. (2001). Relations between anxiety sensitivity and panic symptoms in nonreferred children and adolescents. Journal of
Behavior Therapy and Experimental Psychiatry, 32, 117-136. doi: 10.1016/
S0005-7916(01)00026-X
Clark, D.M. (1988). A cognitive model of panic attacks. In S. Rachman, & J.D. Maser
(Eds.), Panic: Psychological Perspectives (pp. 71-89). Hillside, NJ: Lawrence
Erlbaum.
Clark, D.M. (1989). Anxiety states: Panic and generalized anxiety. In K. Hawton, P.
Salkovakis, J. Kirk, & D.M. Clark (Eds.), Cognitive behavior therapy for psychiatric problems: A practical guide (pp. 52-96). Oxford, UK: Oxford University Press.
Micco et al.
21
Clark, D.M., Salkovakis, P.M., Hackmann, A., Middleton, H., Anastasiades, P., &
Gelder, M. (1994). A comparison of cognitive therapy, applied relaxation, and
imipramine in the treatment of panic disorder. British Journal of Psychiatry, 164,
759-769.
Clark, D.M., Salkovakis, P.M., Ost, L.-G., Breitholtz, S., Koehler, K.A., Westling,
B.E., Jeavons, A., & Gelder, M. (1997). Misinterpretations of body sensations in
panic disorder. Journal of Consulting and Clinical Psychology, 65, 203-213. doi:
10.1037/0022-006X.65.2.203
Craske, M.G., Brown, T.A., & Barlow, D.H. (1991). Behavioral treatment of panic disorder: A two-year follow-up. Behavior Therapy, 22, 289-304. doi: 10.1016/S00057894(05)80367-3
Craske, M.G., Rowe, M., Lewin, M., & Noriega-Dimitri, R. (1997). Interoceptive exposure versus breathing retraining in cognitive-behavioural therapy for panic disorder with agoraphobia. British Journal of Clinical Psychology, 36, 85-99.
Ginsburg, G.S., & Drake, K.L. (2002). Anxiety sensitivity and panic attack symptomatology among low-income African-American adolescents. Journal of Anxiety Disorders, 16, 83-96. doi: 10.1016/S0887-6185(01)00092-5
Hayward, C., Killen, J.D., & Hammer, L.D. (1992). Pubertal stage and panic attack history in sixth- and seventh-grade girls. American Journal of Psychiatry, 149, 12391243.
Hayward, C., Killen, J.D., Kraemer, H.C., & Taylor, C.B. (2000). Predictors of panic
attacks in adolescents. Journal of the American Academy of Child and Adolescent
Psychiatry, 39, 207-214. doi: 10.1097/00004583-200002000-00021
Hayward, C., Killen, J.D., and Taylor, C. B. (1989). Panic attacks in young adolescents. American Journal of Psychiatry, 146, 1061-1062.
Hayward, C., Killen, J.D., & Taylor, C.B. (2003). The relationship between agoraphobia symptoms and panic disorder in a non-clinical sample of adolescents. Psychological Medicine, 33, 733-738. doi: 10.1017/S0033291702006955
Hecker, J.E., Fink, C.M., Vogeltanz, N.D., Thorpe, G.L., & Sigmon, S.T. (1998). Cognitive restructuring and interoceptive exposure in the treatment of panic disorder: A
cross-over study. Behavioural and Cognitive Psychotherapy, 26, 115-131.
Hoffman, E C. & Mattis S.G. (2000). A developmental adaptation of panic control
treatment for panic disorder in adolescence. Cognitive and Behavioral Practice, 7,
253-261. doi: 10.1016/S1077-7229(00)80081-4
Hudson, J.L. (2005). Mechanisms of change in cognitive behavioral therapy for anxious youth. Clinical Psychology: Science and Practice, 12, 161-165. doi: 10.1093/
clipsy/bpi019
Ito, L.M., Noshirvani, H., Basoglu, M., & Marks, I.M. (1996). Does exposure to internal cues enhance exposure to external cues in agoraphobia with panic? Psychotherapy and Psychosomatics, 65, 24-28.
Kearney, C. A., Albano, A., Eisen, A. R., Allan, W. D., and Barlow, D. H. (1997). The
phenomenology of panic disorder in youngsters: An empirical study of a clinical
sample. Journal of Anxiety Disorders, 11, 49-62. doi: 10.1016/S08876185(96)00034-5
22
CHILD & FAMILY BEHAVIOR THERAPY
King, N. J., Ollendick, T. H., Mattis, S. G., Yang, B., and Tonge, B. (1996). Nonclinical
panic attacks in adolescents: Prevalence, symptomatology, and associated features.
Behaviour Change, 13, 171-183.
Last, C. G., and Strauss, C. C. (1989). Panic disorder in children and adolescents. Journal of Anxiety Disorders, 3, 87-95. doi: 10.1016/0887-6185(89)90003-0
Lau, J.J., Calamari, J.E., & Waraczynski, M. (1996). Panic attack symptomatology and
anxiety sensitivity in adolescents. Journal of Anxiety Disorders, 10, 355-364. doi:
10.1016/0887-6185(96)00016-3
Ley, R. (1985). Blood, breath, and fears: A hyperventilation theory of panic attacks and
agoraphobia. Clinical Psychology Review, 5, 271-285. doi: 10.1016/02727358(85)90008-X
Macaulay, J.L., & Kleinknecht, R.A. (1989). Panic and panic attacks in adolescents.
Journal of Anxiety Disorders, 3, 221-241. doi: 10.1016/0887-6185(89)90016-9
March, J.S. (1997). The Multidimensional Anxiety Scale for Children (MASC). North
Tonawanda, NY: Multi-Health Systems, Inc.
Masi, G, Favilla, L., Mucci, M., & Millepiedi, S. (2000). Panic disorder in clinically referred children and adolescents. Child Psychiatry and Human Development, 31,
139-151. doi: 10.1023/A:1001948610318
Mattis, S.G., Cohen, E.M., Hoffman, E.C., Pincus, D.P., Choate, M.L., & Micco, J.A.
(2001, March). Cognitive-Behavioral Treatment of Panic Disorder in Adolescents.
Symposium conducted at the 21st annual meeting of the Anxiety Disorders Association of America. Atlanta, GA.
Mattis, S.G., & Ollendick, T.H. (2002). Panic Disorder and Anxiety in Adolescents.
Oxford, UK: Blackwell Publishing.
Mattis, S.G. & Pincus, D.B. (2004). Treatment of SAD and panic disorder in children
and adolescents. In P. Barrett & T. Ollendick, (Eds), Handbook of interventions that
work with children and adolescents: Prevention and treatment. West Sussex, England: Wiley.
Mattis, S.G., Pincus, D.P., Ehrenreich, J.T., & Barlow, D.H. (2006). Cognitive Behavioral Treatment of Panic Disorder in Adolescents. Manuscript submitted for publication.
Meuret, A.E., Wilhelm, F.H., Ritz, T., & Roth, W.T. (2003). Breathing retraining for
treating panic disorder: Useful intervention or impediment? Behavior Modification,
27, 731-754. doi: 10.1177/0145445503256324
Nelson, W.A., & Clum, G.A. (2002). Assessment of panic frequency: Reliability and
validity of a time-line follow-back method. Journal of Psychopathology and Behavioral Assessment, 24, 47-54. doi:10.1023/A:1014053224844
Ollendick, T. H. (1995). Cognitive behavioral treatment of panic disorder with agoraphobia in adolescents: A multiple baseline design analysis. Behavior Therapy, 26,
517-531. doi: 10.1016/S0005-7894(05)80098-X
Papp, L.A., Martinez, J.M., Klein, D.F., Coplan, J.D., Norman, R.G., Cole, R., deJesus,
M.J., Ross, D., Goetz, R., & Gorman, J.M. (1997). Respiratory psychophysiology
of panic disorder: Three respiratory challenges in 98 subjects. American Journal of
Psychiatry, 154, 1557-1565.
Micco et al.
23
Pham, T.D., Tang, T.Z., Zinbarg, R., & Andrusyna, T. (2004, November). Sudden gains
in cognitive-behavioral therapy for panic disorder. In T.Z. Tang (Chair), Sudden
Gains and Therapy Mechanism. Symposium conducted at the 38th annual meeting of
the Association of the Advancement of Behavior Therapy, New Orleans, LA.
Rapee, R.M., Brown, T.A., Antony, M.M., & Barlow, D.H. (1992). Response to hyperventilation and inhalation of 5.5% carbon dioxide-enriched air across DSM-III-R
anxiety disorders. Journal of Abnormal Psychology, 101, 538-552. doi: 10.1037/
0021-843X.101.3.538
Rapee, R.M., Craske, M.G. & Barlow, D.H. (1990). Self-described features of panic
attacks using self-monitoring. Journal of Anxiety Disorders, 4, 171-181. doi: 10.1016/
0887-6185(90)90009-X
Reed, V., & Wittchen, H.U. (1998). DSM-IV panic attacks and panic disorder in a
community sample of adolescents and young adults: How specific are panic attacks? Journal of Psychiatric Research, 32, 335-345. doi: 10.1016/S00223956(98)00014-4
Reynolds, C.R., & Richmond, B.O. (1978). What I think and feel: A revised measure of
children’s manifest anxiety. Journal of Abnormal Child Psychology, 6, 271-280.
Roth, W.T., Wilhelm, F.H., & Trabert, W. (1998). Voluntary breath holding in panic
and generalized anxiety disorders. Psychosomatic Medicine, 60, 671-679.
Schmidt, N.B., Woolaway-Bickel, K., Trakowski, J., Santiago, H., Storey, J., Koselka,
M., & Cook, J. (2000). Dismantling cognitive-behavioral treatment for panic disorder: Questioning the validity of breathing retraining. Journal of Consulting and
Clinical Psychology, 68, 417-424. doi: 10.1037/0022-006X.68.3.417
Silverman, W.K., & Albano, A.M. (1997). Anxiety Disorders Interview Schedule for
DSM-IV, Child and Parent Versions. San Antonio, TX: Psychological Corporation.
Silverman, W.K., Fleisig, W., Rabian, B., & Peterson, R.A. (1991). Childhood Anxiety
Sensitivity Index. Journal of Clinical Child Psychology, 20, 162-168. doi: 10.1207/
s15374424jccp2002_7
Stiles, W.B., Leach, C., Barkham, M., Lucock, M., Iveson, S., Shapiro, D.A., Iveson,
M., & Hardy, G.E. (2003). Early sudden gains in psychotherapy under routine clinic
conditions: Practice-based evidence. Journal of Consulting and Clinical Psychology, 71, 14-21. doi:10.1037/0022-006X.71.1.14
Tang, T.Z., & DeRubeis, R.J. (1999). Sudden gains and critical sessions in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology, 67, 894-904. doi: 10.1037/0022-006X.67.6.894
Telch, M.J., Schmidt, N.B., Jaimez, T.L., Jacquin, K.M., & Harrington, P.J. (1995).
Impact of cognitive-behavioral treatment on quality of life in panic disorder patients. Journal of Consulting and Clinical Psychology, 63, 823-830. doi: 10.1037/
0022-006X.63.5.823
RECEIVED: 8/18/06
REVISED: 11/10/06
ACCEPTED: 11/20/06
doi:10.1300/J019v29n04_01