General principles of decontamination and waste disposal
advertisement

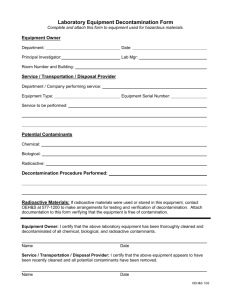
Transmissible Spongiform Encephalopathy Agents: Safe Working and the Prevention of Infection: Annex C ANNEX C General principles of decontamination and waste disposal Introduction C1. This annex has been updated to provide information on the general principles of decontamination and waste disposal for transmissible spongiform encephalopathies (TSEs). A list of selected guidelines and standards related to decontamination and waste disposal is included as Table C4. Guidance on decontamination and waste disposal in a healthcare setting can now be found in Part 4 of this guidance. Guidance on decontamination and waste disposal in a laboratory setting can now be found in Part 3 of this guidance. The Decontamination Cycle for reusable medical equipment C2. ACQUISITION 1. Purchase 2. Loan CLEANING TRANSPORT DISINFECTION At all stages: Location Facilities Equipment Management Policies/Procedures USE STORAGE INSPECTION PACKAGING TRANSPORT STERILISATION DISPOSAL 1. Scrap 2. Return to lender Decontamination and TSE agents C3. TSE agents are particularly resistant to standard physical and chemical methods of inactivation and decontamination. Therefore, effective cleaning is of great importance in the removal of these agents. 1 Published: November 2009 Transmissible Spongiform Encephalopathy Agents: Safe Working and the Prevention of Infection: Annex C C4. Details of chemical and gaseous disinfectants and physical processes commonly used for decontamination, and their effectiveness at reducing infectivity, are outlined below. It should be noted that combinations of some agents and/or processes could be effective, for example, physical/chemical combinations such as autoclaving with sodium hydroxide. Chemical decontamination C5. Most chemical disinfectants are ineffective at reducing infectivity and some, acting as protein fixatives, may stabilise the agent (see Table C1). Table C1: Ineffective chemical disinfectants Chemical disinfectants commonly INEFFECTIVE at reducing infectivity used for decontamination that are Alcohols1 Ammonia ß-propiolactone Chlorine dioxide Ethylene oxide Formaldehyde and related compounds1 Glutaraldehyde and related compounds1 (e.g. orthophthalaldehyde [OPA]) Hydrochloric acid (Not reliably effective for practicable use) Hydrogen peroxide Iodophors Peracetic acid Aqueous solutions of phenol (≤90% phenol) Sodium dichloroisocyanurate (e.g. ‘Presept’)2 10,000ppm sodium hypochlorite (Not reliably effective for practicable use) 1 These agents are strong fixatives, may stabilise infectivity and thereby decrease the efficiency of the decontamination process 2 The rate of release of chlorine from this product is insufficient to ensure complete inactivation of the agent C6. Sodium hypochlorite is considered to be effective at reducing infectivity but only at concentrations (20,000ppm available chlorine for 1 hour) that pose certain practical constraints. The following should be taken into account when considering the use of sodium hypochlorite: o It must not be used on open surfaces i.e. benches due to the possible release of chlorine gas 2 Published: November 2009 Transmissible Spongiform Encephalopathy Agents: Safe Working and the Prevention of Infection: Annex C C7. o It corrodes metal and steel o It is incompatible with formaldehyde, alcohols and acids o It is rapidly inactivated by protein residues o Concentrated stock dilutions last for only approximately 2-3 weeks o Diluted solutions are not stable and should be made up daily Sodium hydroxide (2M for 1 hour) has a substantial effect. An increase in temperature will increase effectiveness. The following should be taken into account when considering the use of 2M sodium hydroxide: C8. o It should not be used on aluminium or zinc o It will not cause fumes but is damaging to body tissue o It is an irritant and harmful as dust Formic acid (96% for 1 hour) may be used for histological samples of human or animal tissue that have previously been fixed in formalin. However, it should not be used on tissue that has previously been exposed to phenol, as this interacts deleteriously with formic acid. C9. Phenol (≥ 90% phenol) is highly effective at eliminating infectivity. Phenol is a toxic, corrosive and irritant chemical which can be absorbed through mucous membranes, wounds and intact skin, and should be used cautiously and with the appropriate personal protective clothing. Physical processes Incineration C10. Incineration is effective at removing the infectious agent and eliminating infectivity. Temperatures over 600ºC are likely to be practically effective, and 850ºC is commonly used in practice. Temperatures ≥1000 ºC can produce sterility. The particle size of material to be combusted should be suitably small to ensure efficient heat penetration to the centre. Autoclaving C11. Autoclaving remains an important method of reducing infectivity. Different strains of TSE are also known to vary in their sensitivity to heat. C12. The following holding times will reduce infectivity but cannot be relied upon to completely eliminate infectivity (either porous load or gravity displacement): • 121°C for 15 minutes 3 Published: November 2009 Transmissible Spongiform Encephalopathy Agents: Safe Working and the Prevention of Infection: Annex C C13. • 134-137°C for 3 minutes • 134-137°C for 18 minutes • Six successive cycles of 134-137°C for 3 minutes The ‘Prion Cycle’ found on some benchtop vacuum autoclaves will also reduce infectivity but will not eliminate infectivity entirely. See MHRA Safety Notice ‘SN 2002(11): Benchtop vacuum steam sterilizers – the ‘prion cycle’: http://www.mhra.gov.uk/Publications/Safetywarnings/MedicalDeviceAlerts/Safetynoti ces/CON008791 Radiation C14. Ionising, UV or microwave radiation at conventional doses are not effective at reducing infectivity. Other processes C15. A number of anti-prion technologies are currently in development. The Engineering and Science Advisory Committee into the Decontamination of Surgical Instruments including Prion Removal (ESAC-Pr) produced a report on prion inactivating agents, written by their New Technologies Working Group, in August 2008. This report provides advice on various anti-prion technologies that are on, or close to coming on, the market, their applicability to the current decontamination process for reusable medical equipment, and the direction of future research needs. The report can be accessed here. 4 Published: November 2009 Transmissible Spongiform Encephalopathy Agents: Safe Working and the Prevention of Infection: Annex C Table C4: Selected guidelines and standards related to decontamination and waste disposal Name 93/42/EEC The Medical Devices Directive Date published 1993 UK law since 1998 Brief description This Directive under European Law covers the placing on the market and putting into service of Medical Devices (other than active implantable and in vitro diagnostic devices). Available here. Essential requirements in the Directive are listed under Annex 1. Two essential requirements under section 8 – Infection and microbial contamination – are particularly relevant: “8.4: Devices delivered in a sterile state must have been manufactured and sterilised by an appropriate validated method.” “8.5: Devices intended to be sterilised must be manufactured in appropriately controlled (e.g. environmental) conditions.” Medical Devices Regulations 2002 These UK Regulations are drawn from the Medical Devices Directive 93/42/EEC DH Estates and Facilities (formerly NHS Estates) Health Building Notes (HBN) HBN provide advice to project teams designing and planning new buildings and adapting/extending existing buildings. HBNs are available free to NHS staff who register with the DH Knowledge and Information Portal http://estatesknowledge.dh.gov.uk/ HBN 13 2004 Design of Sterile Service Departments This HBN provides guidance to help health planners, estates and facilities managers, sterile services managers and capital planning and design teams to plan and design a sterile services department. It supersedes HBN 13 ‘Sterile services departments’, published in 1992. In Scotland, the relevant document is SHBN 13. DH Estates and Facilities (formerly NHS Estates) Engineering Health Technical Memoranda (HTM) HTMs provide guidance for the design, installation and running of specialised building service systems. HTMs are available free to NHS staff who register with the DH Knowledge and Information Portal http://estatesknowledge.dh.gov.uk/ HTM 2010 Sterilization 1995 This HTM provides guidance on choice, specification, purchase, installation, validation, periodic testing, operation and maintenance of clinical and laboratory sterilizers. It is intended primarily as a guide for technical personnel who are specialists in sterilizing processes and procedures and for those responsible for maintenance and testing. It is also for staff who have responsibility for the day-to-day running of sterilizers. In Scotland, the relevant document is SHTM 2010. 5 Published: November 2009 Transmissible Spongiform Encephalopathy Agents: Safe Working and the Prevention of Infection: Annex C HTM 2031 1997 HTM 2031 covers the nature of contamination in steam supplies, regulatory requirements for steam quality, the new “clean steam” specification, engineering measures for the generation of clean steam, validation and periodic testing of clean steam supplies and guidance on the analysis of steam samples. It supplements the guidance on steam quality in HTM 2010 ‘Sterilization’. In Scotland, the relevant document is SHTM 2031. 1997 HTM 2030 gives guidance on the choice, specification, purchase, installation, validation, periodic testing, operation and maintenance of washer-disinfectors in use in the National Health Service for processing medical devices, laboratory ware and sanitary products. In Scotland, the relevant document is SHTM 2030. Part A 2007 This HTM, once fully published, will replace HTM 2010, HTM 2031 and HTM 2030, amongst others. The HTM is in four parts: Clean Steam HTM 2030 Washer Disinfectors HTM 01-01 Decontamination of Medical Devices Part A – Management and Environment Part B – Equipment Part C – Sterilizers Part D – Washer disinfectors Parts B, C and D are currently in preparation and due to be published in late 2009. HTM 01-02 In preparation Pathology Decontamination HTM 01-04 In preparation Laundry Decontamination HTM 01-05 Dental Decontamination 2009 This guidance has been produced to reflect a reasonable and rational response to emerging evidence around the effectiveness of decontamination in primary care dental practices, and the possibility of prion transmission through protein contamination of dental instruments. Available here. HTM 01-06 In preparation, due to be published in late 2009 Endoscope Decontamination HTM 01-07 In preparation Primary Care Decontamination 6 Published: November 2009 Transmissible Spongiform Encephalopathy Agents: Safe Working and the Prevention of Infection: Annex C HTM 07-01 2006 Safe management of healthcare waste This document is a best practice guide to the management of healthcare waste. Healthcare waste refers to any waste produced by, and as a consequence of, healthcare activities. For the purposes of this document, this guidance also applies to offensive/hygiene and infectious waste produced in the community from non-NHS healthcare sources. The document replaces the Health Services Advisory Committee’s (1999) guidance document ‘Safe disposal of clinical waste’ and takes into account the changes in legislation governing the management of waste, its storage, carriage, treatment and disposal, and health and safety. This guidance document was produced by DH, supported by the Environment Agency, Defra, HSE, the Department for Transport, Welsh Health Estates and Health Facilities Scotland. Device Bulletins (DB) The Medicines and Healthcare Products Regulatory Agency (MHRA) produce Device Bulletins that contain guidance and information on medical devices of a more general management interest. They are written as a result of experience gained from adverse incident investigations, contacts with manufacturers and users, and other sources of information. DB 2002(05) 2002 This Bulletin (due for update and revision) is intended to offer advice and guidance to both users and manufacturers of devices and reprocessing equipment. It draws together existing advice, with particular reference to disinfectant contact times. Personnel with responsibility for decontamination and infection control may base their processing procedures on this information. Available here. 2002 This Bulletin (due for update and revision) provides guidance on the purchase, operation and maintenance of all types of benchtop steam sterilizers. The guidance is intended for potential purchasers, and all current owners and users of benchtop steam sterilizers. Available here. Decontamination of Endoscopes DB 2002(06) Benchtop steam sterilizers: guidance on purchase, operation and maintenance Other relevant guidance The Glennie framework 2001 The first report from the Sterile Services Provision Review Group, NHS Scotland. This Group, led by John Glennie, Chief Executive of Borders General Hospital NHS Trust, undertook a review of sterile service provision across NHS Scotland. Available here. Infection control in dentistry 2003 This advice sheet condenses current knowledge and recommendations on infection control for the dental practitioner. It was developed with the DH in England and is consistent with current infection control policies in the NHS. Its production and distribution to dentists in the UK has been financed by the DH. It is commonly known as the A12 document. Available here. British Dental Association advice sheet A12 7 Published: November 2009 Transmissible Spongiform Encephalopathy Agents: Safe Working and the Prevention of Infection: Annex C “MAC Manual” Sterilization, Disinfection and Cleaning of Medical Equipment: Guidance on Decontamination from the Microbiology Advisory Committee to the Department of Health Part 1 – 2002 Part 2 – 2005 Part 3 – 2006 This publication, known as the MAC Manual, has been prepared and endorsed by the MHRA's Microbiology Advisory Committee to provide advice on all aspects of decontamination. Available here. Part 1 – Principles (2002 revision currently under review) this part provides the general principles of decontamination, illustrated by some examples of basic decontamination equipment. Part 2 – Protocols – this part contains the protocols for decontamination using cleaning, disinfection and sterilization processes. The introduction provides general guidance on the need for systems of work for the decontamination of medical devices and equipment both prior to clinical use and before inspection, service or repair. A general protocol for handling items to be maintained or repaired is then provided, and detailed protocols for cleaning, disinfection and sterilization follow this. Part 3 – Procedures – Section 1 provides an overview of what the European Directives for medical devices mean for users. Section 2 provides general procedures to be followed for particular groups of equipment including: Standards and Practice 2007 • Endoscopes • Dental equipment • Ophthalmic instruments • Surgical instruments • Ventilators • Miscellaneous items The Institute of Decontamination Sciences (IDSc), formerly the Institute of Sterile Services Management, has produced a revised third edition of this guidance, which sets out in detail the operational, technical and managerial requirements of decontamination services and provides a useful resource for anyone working in or around decontamination. The revised 3rd edition has been extensively updated to include the latest legislative framework referencing the work of the Healthcare Commission, ISO 13485 and the revised HBN13. A hardcopy of ‘Standards and Practice’ is free to full members of the Institute. Non-members can purchase hardcopies of the guidance. More information available here. 8 Published: November 2009