Menstrual Cycle: Ovarian & Uterine Phases Explained
advertisement
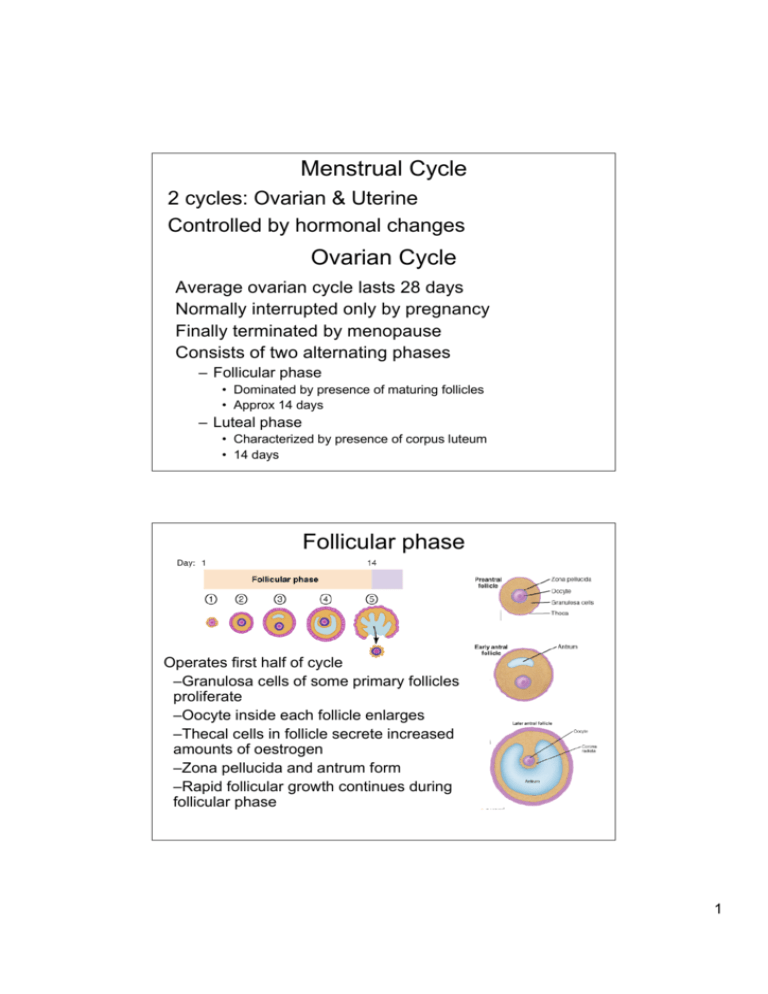
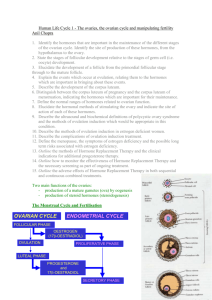
Menstrual Cycle 2 cycles: Ovarian & Uterine Controlled by hormonal changes Ovarian Cycle Average ovarian cycle lasts 28 days Normally interrupted only by pregnancy Finally terminated by menopause Consists of two alternating phases – Follicular phase • Dominated by presence of maturing follicles • Approx 14 days – Luteal phase • Characterized by presence of corpus luteum • 14 days Follicular phase Operates first half of cycle –Granulosa cells of some primary follicles proliferate –Oocyte inside each follicle enlarges –Thecal cells in follicle secrete increased amounts of oestrogen –Zona pellucida and antrum form –Rapid follicular growth continues during follicular phase 1 Follicular phase One follicle usually grows more rapidly & matures about 14 days after onset of follicular development - Graafian or mature follicle - Oocyte surrounded by zona pellucida and single layer of granulosa cells Follicular phase: hormonal control FSH and oestrogens stimulate follicle growth and development Flow chart shows production of oestrogen by follicle 2 Ovulation – Wall of Graffian follicle ruptures – Antral fluid with oocyte flows to ovarian surface – Fluid and oocyte released – Oocyte enters uterine tube – Hormonal control: LH surge is trigger – 2 or more follicles may become dominant and released at ovulation – If both are fertilized – fraternal twins – Also called dizygotic twins (develop from 2 zygotes) Ovarian Cycle: Luteal phase – Last 14 days of ovarian cycle – Old follicular cells undergo structural transformation to form corpus luteum (gland) – Becomes highly vascularized – Fully functional within four days after ovulation – Continues to increase in size for another 4-5 days – If released ovum is not fertilized and does not implant, corpus luteum degenerates within about 14 days after formation – Hormonal control: LH causes development of corpus luteum from empty Graafian follicle 3 Ovarian cycle: summary Uterine Cycle • Reflects hormonal changes during ovarian cycle • Averages 28 days • Consists of three phases – Menstrual phase (decreased oestrogen & progesterone) • Uterine lining is shed. 5-7 days – Proliferative phase (oestrogen) • Endometrium renewed in preparation for possible pregnancy – Secretory or progestational phase (progesterone) • Coincides with luteal phase. Endometrium develops 4 Menstrual phase – Characterized by discharge of blood and endometrial debris from vagina – First day of menstruation is considered start of new cycle – Coincides with end of ovarian luteal phase and onset of follicular phase – Triggered by decreased oestrogen and progesterone: hormones decrease when CL degenerates – Release of uterine prostaglandin • Causes vasoconstriction of endometrial vessels – Disrupts blood supply – Causes death of endometrium • Stimulates mild rhythmic contractions of uterine myometrium – Helps expel the menstrual flow Proliferative phase Begins concurrent with last portion of ovarian follicular phase Uterus prepares for fertilized ovum: Endometrium starts to repair itself and proliferate under influence of oestrogen from newly-growing follicles Oestrogen-dominant proliferative phase lasts from end of menstruation to ovulation Peak oestrogen levels trigger LH surge responsible for ovulation 5 Secretory phase Endometrium prepared for implantation – Blood supply increased – Glands enlarge and secrete glycogen-rich fluids – Secretory phase conditions promoted by progesterone – Uterus enters this phase after ovulation when new corpus luteum is formed – Corpus luteum secretes large amounts of progesterone and oestrogen • Progesterone converts endometrium to highly vascularized, glycogen-filled tissue – Endometrial glands actively secrete glycogen – If fertilization and implantation do not occur • Corpus luteum degenerates • New follicular phase and menstrual phase begin again Timing of ovarian and uterine cycles 6 Hormonal control of the cycle GnRH Gonadotropins (FSH and LH) Oestrogen and progesterone FSH: follicle stimulating hormone growth and development of follicles LH: luteinising hormone causes ovulation development of corpus luteum Inhibin: decreases FSH, not LH Hormonal control of the cycle Oestrogens Progesterone Stimulate oogenesis and follicle development Promotes secretory-phase uterine conditions Promote proliferative-phase uterine conditions Suppresses uterine during pregnancy Induce expression of progesterone receptors Promotes growth of glandular breast tissue but suppresses milk production uterine contraction Induce expression of granulosa cell LH receptors Secondary sexual characteristics Breast growth during pregnancy 7 – Oestrogen secreted first from the follicle, then from the corpus luteum – Progesterone secreted from the corpus luteum – LH and FSH secreted from the anterior pituitary – Oestrogen and progesterone inhibit LH and FSH secretion Regulation of Hormone Secretion: Mid-Follicular Phase Permissive Effects of Hormones during Mid-Follicular Phase – FSH •Granulosa cells theca cells •Theca cells have LH receptors – Oestrogens •LH receptors on granulosa cells •Progesterone receptors on endometrial cells 8 Regulation of Hormone Secretion – Late Follicular Phase Oestrogens stimulate LH secretion (opposite of usual effect) This is one of the rare examples of positive feedback in Physiology Hormonal control: ovulation 9 Regulation of Hormone Secretion: Luteal Phase Long-Term Regulation of Female Reproductive Function Puberty • Oestrogen – secondary sex characteristics Reproductive years • Oestrogen levels high to maintain secondary sex characteristics Menopause • Cessation of woman’s menstrual cycle • Age 45 to 55 • Preceded by period of progressive ovarian failure – Increasingly irregular cycles – Dwindling oestrogen levels • Loss of oestrogen primarily affects skeleton and cardiovascular system (increased risk of heart disease and osteoporosis) 10