Wellott, Jennie
advertisement
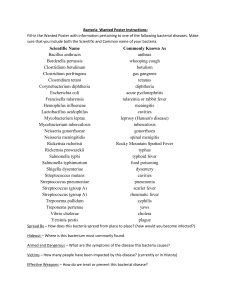
Wellott-J-6 Group B strep (GBS) …“Baby Strep” I will be focusing on the effects this disease has on pregnancy. Group B Streptococcus is a bacteria that causes illness in persons of any age, but it typically found in the vagina or rectum of healthy women. It is found in most of its cases to target newborns with life-threatening conditions. Group B Strep is a bacteria known as Streptococcus Agalactiae. This is a gram positive, Beta-hemolytic streptococci; meaning that when placed on a blood agar plate, results show large, clear areas surrounding the bacterial colonies. The cleared area indicates that the blood cells that were initially on the agar have completely ruptured. Once in the host, it uses polysaccharides as well as surface proteins to adhere itself to the host’s epithelial cells and harm the defense system. It is a mesophile, and its optimal temperature is 37°C, making the human body the perfect environment for growth and reproduction. However, the source of infection for adults is currently unknown… The bacteria likes to make itself home in the intestine, vagina, or rectal areas. Therefore, this raises major concern for pregnant women. About 1 in 4 women already carry the bacteria, and for most of those women symptoms go unknown. So, if a woman is positive for GBS without knowing, the baby passes through the birth canal and is now at very high risk for hosting the disease. Luckily, the CDC recommends routine screening for the bacteria in all pregnant women. The scary part for adults is that symptoms usually go unnoticed, the most common problems are bone/tissue/skin/joint/urinary and bloodstream infections. In some serious cases pneumonia can develop. If the disease is indeed suspected, then the care practitioner will take a sterile fluid sample, or swab the vagina or rectum. If a woman is tested and found positive, then an antibiotic (penicillin or ampicillin) will be given through IV during labor to prevent the passing of the disease from mother to baby. What is even scarier, is that even if a woman is found positive early in the pregnancy, antibiotics are not given. This is because they naturally live inside of the GI tract, therefore, even if treated with antibiotics early on, there is still a great chance for the bacteria to make itself present again. So, if not tested early on, they are tested late in their third trimester (35-37 weeks). So, if you are found to be a carrier, you MUST inform your midwife/doctor so that you can be given antibiotic during labor. If a newborn does in-fact contract the disease, there can be early-onset factors (noticeable at birth) as well as late-onset (one week to 3 months of life). If newborns host the disease, it is a life-threatening situation because of their small bodies, and not yet developed immune systems, as well as seldom antibodies to try and fight off the infection. These SERIOUS symptoms include difficulty breathing, difficulties feeding, pneumonia, sepsis (infection of the blood), and meningitis (infection of the fluid and lining surrounding the brain), or even worse, still birth. The newborns are treated with antibiotics, but if a more sever case resides then other measures/procedures may be needed. Resources http://www.cdc.gov/groupbstrep/about/index.html http://www.womenshealth.gov/pregnancy/you-are-pregnant/pregnancy-complications.html http://americanpregnancy.org/pregnancycomplications/groupbstrepinfection.html http://microbewiki.kenyon.edu/index.php/Streptococcus_agalactiae