Amenorrhea
advertisement

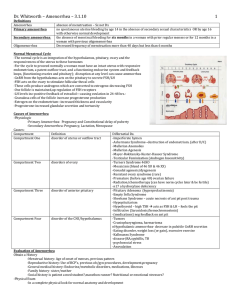
Amenorrhea Yousef R.Badran Amenorrhea • Amenorrhea is the absence of menstruation. • Primary: – Absence of menses by age 16 with normal secondary sexual characteristics. – Absence of menses by age 14 without secondary sexual development. • Secondary – Absence of menses for 3 cycles or 6 months in a previously menstruating females. • Oligomenorrhea – Interval of more than 35 days between periods Events of Puberty • Thelarche (breast development) – Requires estrogen • Pubarche/adrenarche (pubic hair development) – Requires androgens Events of Puberty • Menarche Requires: – GnRH from the hypothalamus – FSH and LH from the pituitary – Estrogen and progesterone from the ovaries – Normal outflow tract P1 P2 P3 P4 P5 Epidemiology Estrogen Production Adrenal Hormones Pathophysiology Inadequate hormonal stimulation of the endomerium “Anovulatory amenorrhea” - Euestrogenic - Hypoestrogenic Inability of endometrium to respond to hormones “Ovulatory amenorrhea” - Uterine absence - Utero-vaginal agenesis - XY-Females ( e.g T.F.S) - Damaged endometrium ( e.g Asherman’s syndrome) Causes of 1ry Amenorrhea • 1- Hypergonadotropic hypogonadism (48.5% of cases) • 2- Hypogonadotropic hypogonadism (27.8%) • 3- Eugonadism (pubertal delay with normal gonadotropins; 23.7%). Uptodate • Chromosomal abnormalities causing gonadal dysgenesis (ovarian failure due to the premature depletion of all oocytes and follicles) — 50 % • Hypothalamic hypogonadism including functional hypothalamic amenorrhea — 20 % • Absence of the uterus, cervix and/or vagina, müllerian agenesis — 15 % • Transverse vaginal septum or imperforate hymen — 5 percent • Pituitary disease — 5 % Causes of 2ry Amenorrhea • 1-Disorders associated with a low or normal FSH, which account for 66% • 2-Disorders in which the FSH is high (12%) • 3-Disorders associated with a high prolactin level comprise 13% of cases • 4- Anatomic disorders (ie, Asherman syndrome) account for 7%. • 5- Hyperandrogenic states as a cause of secondary amenorrhea (2%) Classification of Amenorrhea • Outflow Tract Anomalies • Ovarian amenorrhea • Central Disorders: – Hypothalamic amenorrhea – Pituitary amenorrhea Which is which??? Only 3 diagnoses are unique to primary amenorrhea and never cause secondary amenorrhea. 1- vaginal agenesis 2- androgen insensitivity syndrome 3- Turner syndrome (45,Xo) Etiology: Outflow Tract Anomalies • Mullerian Anomalies: – Imperforate hymen – Transverse vaginal septum – Cervical Stenosis (2ry) • Asherman syndrome (2ry) • Mullerian Agensis: – Vaginal and uterine aplasia-MayerRokitansky-Küster-Hauser • Testicular feminization Imperforate Hymen • Intermittent abdominal pain • Possible difficulty with micturition • Possible lower abdominal swelling • Bulging bluish membrane at the introitus or absent vagina (only dimple Transverse Vaginal Septum Mayer-Rokitansky-Kuster-Hauser Syndrome (utero-vaginal agenesis) • Mullerian Agenesis or Dysgenesis • Complete vaginal agenesis and absence of a uterus or partial vaginal agenesis with rudementary uterus and distal vagina. • Karyotype 46-XX • Ovaries present Androgen Insensitivity • Karyotype 46, XY • X linked recessive • Loss-of-function mutation in the androgen receptor (AR) gene. This AR gene has been localized to the long arm of the X chromosome (ie, Xq11-13). • Undervirilization • Normal breasts but no sexual hair Androgen Insensitivity • Phenotypical female • Absent uterus and upper vagina • Male range testosterone level • 25% chance of developing benign testicular tumors and a 4-9% chance of malignancy. • Treatment : gonadectomy after puberty + HRT Asherman Syndrome Photograph of the hysteroscopic view of a uterine cavity with severe intrauterine synechiae (Asherman’s syndrome) that occupied the bulk of the cavity. The midline fundal location of the abnormal tissue is similar to that seen with a uterine septum (the eccentric rotation of the scar tissue is not characteristic of a uterine septum). Ovarian Amenorrhea • Hypergonadotrophic hypogonadism Hypergonadotrophic Hypogonadism – Variants of Ovarian Dysgenesis • Turner's Syndrome (XO) – Gonadal Toxins (Chemotherapy/Radiation) • Cytotoxic drugs (e.g. Chemotherapy) • Glucocorticoids – Enzyme defects • 17 alpha hydroxylase deficiency Hypergonadotrophic Hypogonadism – Miscellaneous • Mumps • Pelvic radiation • autoimmune – Gonadal failure (in adults) • Hypogonadism in Women – Menopause – Premature Ovarian Failure – Savage Syndrome: failure of response to FSH and LH due to receptor defect Turner’s Sexual infantilism and short stature. • High FSH and LH levels. • Bilateral streaked gonads. • Karyotype - 80 % 45, X0 - 20% mosaic forms (46XX/45X0) • Treatment: HRT Turner’s Syndrome (Classic 45-XO) Mosaic (46-XX / 45-XO) Typical features of Turner Syndrome Gonadal Dysgenesis • Progressive loss of primordial germ cells. This loss leads to hypoplastic and disfunctioning gonads mainly composed of fibrous tissue, streak gonads. • Absence of MIF and testesterone • Regression of Wolffian ducts due to absence of testosterone. • Absence of MIF will allow Mullerian ducts to differentiate into oviducts and uterus • Genotypically male yet will with female like internal and external reproductive characteristics Pure Gonadal dysgenesis • Swyer syndrome:46 XY, no functional gonads. • Mutation of SRY gene • Absence of breasts • Presence of uterus and pubic hair. • High risk of malignancy(eg.Gonadoblastoma) • Surgical removal,HRT Enzyme deficiencies, tricky tricky!! Central Disorders Hypothalamic amenorrhea • GnRH release: – Kallmann syndrome • GnRH transport: compression or destruction of pituitary stalk or arcuate nucleus – – Tumor mass effect trauma – Sarcoidosis – Tuberculosis – Irradiation Central Disorders Hypothalamic amenorrhea GnRH Pulsatility: – Psychological stress – Anorexia nervosa, weight loss – Increased exercise levels – drug-induced amenorrhea – Hyperprolactinemia – Hypothyroidism – Space-occupying lesion of CNS Central Disorders Pituitary amenorrhea • Tumors • Infiltration • Surgery/Irradiation • Empty sella syndrome • Sheehan syndrome • Hemosidrosis Important notes for Diagnosis • Breast development depends on:estradiol • Uterus Presence: Absence of MIF Diagnosis • History • Physical examination – Physical examination begins with vital signs, including height and weight, and with sexual maturity ratings • Laboratory evaluation Hormonal Assays • Estrogen • FSH/LH level • Thyroid function tests • Karyotype • Bone age • Prolactin • Testosterone, DHEAS,17-OHPRog, androstenedione • Pelvic US, imaging • Routine blood work looking for chronicillness Hormonal Assays • Prolactin: prolactinoma, Psychotropic drugs, hypothyroidism, stress, and meals • FSH, ovarian insufficiency • LH, 17,20 lyase deficiency, 17hydroxylase deficiency, and premature ovarian failure. • Estradiol, • Thyroid hormones • Androgens. Diagnostic Evaluation • When to investigate? • No menarche by 15.5-16 years • Investigate earlier if: – Galactorrhea – Short stature – Dysmorphic features – Virilisation – Abnormal pubertal development – Out of keeping with family historyof menarche – Symptoms or signs of hypothalamic-pituitarydisease – Parent/adolescent concerned Evaluating 1ry Amenorrhea Amenorrhea-Galactorrheahyperprolactenemia Progesterone Challenge rationale 2ry Amenorrhea/Progesterone Challenge The 2-Question approach • Has puberty occurred? • “No” then, normal stature or short? “yes”, then Feminizing or virilizing Has puberty occurred? • No • Normal or tall • GnRH deficiency ( FSH low) • Pure FSH deficiency (FSH low) • Pure gonadal dysgenesis (High FSH) Has puberty occurred? • No • Short=something else is going on – Hypopituitarism – Turner’s – Hypothyroidism – FSH slightly high, TSH high Has Puberty occurred? • Yes • Virilizing • 46 xx ( Virlizing female intersex, congenital adrenal hyperplasia) • 46 xy (Virilizing male intersex , Partial androgen insensitivity syndrome, Leydig cell hypoplasia) Has Puberty occurred? • Yes • Feminizing • 46,xx: Idiopathic delay, Mullerian agenesis • 46, xy : Complete androgen insensitivity syndrome Has Puberty occurred? • Uterovaginal agenesis • Low transverse vaginal septum • Complete androgen insensitivity • All the entities of secondary amenorrhea Treatment • treatment varies depending upon the causes of the amenorrhea. Treatment options include: – Dietary changes, including an increase in fat and calories in order to stimulate estrogen production. – Counseling for eating disorders. – Using stress reduction techniques to help regulate the period. – Hormonal supplements, like the birth control pill or patch, or hormone replacement therapy. – Surgery to remove cysts, fibroids or tumors