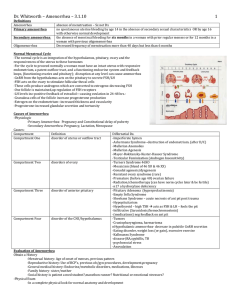
Secondary Amenorrhea
advertisement

Secondary Amenorrhea Case 1: Large Flying Birds Delivering Gifts Case 1: • A 25 yo female presents to your clinic with the co having missed her period the past couple of months. – Is this secondary amenorrhea? – What is secondary amenorrhea? Case 1: • Secondary Amenorrhea: – “absence of menses for more than three cycles or six months in a woman who previously had menses” • (stolen un-gratuitously from UpToDate and our notes from last year) – Does she have secondary amenorrhea? Case 1: • She has been having her period regularly since she was 14. Her cycle is normally 28 days. The last time she had her period was 90 days ago. – Is this secondary amenorrhea? – Yes. What could be causing it? Case 1: • Frequency of causes: – Chronic anovulation (ex: PCOS) – 39% – Hypothyroid/Hyperprolactin – 20% – Weight Loss/Anorexia – 16% Case 1: • Approach to amenorrhea (of any type): • Compartment 1: – Disorders of the outflow tract or uterus. • Compartment 2: – Disorders of the ovary. • Compartment 3: – Disorders of the pituitary. • Compartment 4: – Disorders of the hypothalamus. • 1) History and Physical – Ask about the different compartments/common causes of secondary amenorrhea • • • • • Stress, change in weight, diet, exercise, illness? Acne, hirsutism, deepening of voice? Rx? Pmhx? Headaches, visual field defects? Fatigue, polyuria, polydypsia, etc. ? • Hot flashes, vaginal dryness, poor sleep, decreased libido? Thyroid, Functional AI disease, Hypothalamus/pituitary? • Galactorrhea? Hyperprolactinemia? Asherman? Estrogen PCOS Deficiency Sheehan? • Obstetric hx. renal hypothalamic failure, genetic Danazol, OCP, etc. amenorrhea anti-psychotics? Case 1: • Physical – – – – BMI? Galactorrhea? Vagina/uterus? Etc. • 2) PREGNANCY TEST!!!!! • 3) TSH and PRL levels – PRL (and TRH) inhibit FSH and LH • 4) Progestin Challenge – Is there withdrawal bleeding after progesterone? – Is their body making estrogen, and can they respond to it? – Positive suggests the problem is a “progesterone deficiency. “ • Ie: they are anovulatory (PCOS, Danazol, etc.) – Negative could mean any number of things. Need to narrow down… • 5) FSH level – Low/normal suggests ovaries are good. – High suggests ovarian failure. • 6) Give progesterone and Estrogen. – Bleeding suggests the problem is due to the pituitary/hypothalamus – No bleeding suggests the problem is the endometrium. Case 1: • Physical and history are unremarkable… though… – Her husband and herself use condoms as their only method of contraception. • A urine test for b-HCG is positive… Physical Exam Anatomic abnormality bleeding Normal Pregnancy Test Positive Est/prog Negative High PRL and TSH Elevated Normal Progestin Challenge bleeding Low/normal FSH No blood No blood Case 1: • You recommend she use an additional method other than just condoms to avoid pregnancy in the future. Case 2: She’s back Case 2: • The same patient comes back to see you 10 months later. • Concerned as she’s 4mo pp and still no period. She’s been breast-feeding. • Is this normal? What do you tell her? Case 2: • During pregnancy, estrogen made by the placenta stimulates PRL secretion (but inhibits the effects of PRL on breast tissue) • After birth, no more placenta decreased estrogen. • Suckling decreased PRL-IF produced by the hypothalamus. • Maintained elevated PRL – And therefore, decreased FSH and LH. Case 2: • Reassure her this is normal. • Luckily, she’s on Micronor (progesterone only) for birth control. – (why?) • Plans to switch to a combined OCP after finished breast-feeding. You give her a 5 yr rx for a C-OCP. Case 3: 5 years later… Case 3: • The same patient comes to your office again, 5 years later, and has brought her 5 year old daughter with her. • Her husband and herself have been trying for another child, but she hasn’t been able to get pregnant since they started trying 3ma. Case 3: • She stopped her C-OCP which she had used religiously since her first pregnancy, 2 months ago. • She also hasn’t had a period since she stopped them. • Is this normal? Case 3: • Post-pill amenorrhea – Not that common • ~1 % of women. – Shouldn’t last more than 6 mo. (12mo for depo) Case 3: • You reassure her, and tell her to keep trying. • She comes back in, 7 months after having stopped the OCPs. Still not pregnant. Still no periods either. Case 3: • You get a more complete history. • In her first pregnancy, she suffered a large postpartum bleed, due to retained products of conception. • Needed to be manually removed, via D+C. • Also suffered acute kidney failure at the time due to blood loss, but has had no problems since. • Never had menses since, but thought that was because she had always been on the pill since then. Case 3: • What are you worried about based on this history? – Asherman? – Sheehan? – Chronic Kidney Failure?!?!?!?! • Investigations? – (Cr is normal) Physical Exam Anatomic abnormality bleeding Normal Pregnancy Test Positive Est/prog Negative High PRL and TSH Elevated Normal Progestin Challenge bleeding Low/normal FSH No blood No blood Case 3: • You diagnose her with Asherman Syndrome. – Because you like wasting health care resources, you also order a U/S and a hysteroscopy. – U/S showed lack of normal uterine stripe. – Hysteroscopy confirmed too. • Can she have another baby? Case 3: • Probably – Lysis of adhesions via hysteroscopy – To prevent reformation of adhesions, either • High dose estrogen for 30d followed by progesterone for 10d • Stick a Foley in for 10d • Outcome – Restoration of menstruation in 73-92% of patients – Live delivery rates in up to 76% • Lower in px with more severe adhesions. • In our patient, the surgery was successful, and she was eventually able to conceive another child Case 4: Just to be ridiculous… Case 4: • You meet your patient again, 10 years down the road, but under different circumstances. • Her past medical history is now more extensive: – GERD – Hypertension Case 4: • You also find out that after her second pregnancy, she developed post-partum psychosis, and has been on anti-psychotics since. • Over the years since, she has also been diagnosed with depression for which she is taking a TCA. • She has also been abusing cocaine. Case 4: • Her medications she takes regularly are: – Pepcid (famotidine): 20mg BID – Verapamil: 80mg TID – Risperidone: 6mg OD – Clomipramine: 100mg OD • And guess what? She has amenorrhea again. Case 4: • She had been having her menses consistently until relatively recently, when she had some of her medications adjusted. • On exam, you note that she has galactorrhea… • Pregnancy test is negative. • What’s going on? What do you do next? Physical Exam Anatomic abnormality bleeding Normal Pregnancy Test Positive Est/prog Negative High PRL and TSH Elevated Normal Progestin Challenge bleeding Low/normal FSH No blood No blood Case 4 • Hyperprolactinemia – Tends to only cause amenorrhea when elevated to > 4x normal value (> 100microg/L ) – When associated with amenorrhea, 34% will have a pituitary mass. – Can also be caused by medications, kidney failure, increased estrogen… (endocannabinoids) Rimonabant Exogenous cannabinoids /THC Case 4: • You check her PRL and it is 104 microg/L • • • • You switch her Risperidone to Seroquil You switch her TCA to a SSRI You switch her Verapamil to HCTZ You switch her Famotidine to Omeprazole. (But only because it is associated with a better prognosis for GERD) • She still abuses cocaine though. • And her amenorrhea disappears (along with the galactorrhea). – A repeat PRL is 22 microg/L