SBS Objectives 1/13/05
Sexual Disorders
Dr.Racy
1. Two requirements for DSM-IV diagnosis of sexual disorder:
a. Disorder must interfere with social or occupational functioning, or other
areas.
b. Disorder must be identified as life-long and enduring, or acquired
*Diagnosis should indicate whether the disorder is generalized (occurs on all
occasions) or situational (happens only under certain circumstances) and whether
it is due to psychological factors or to combined psychological and medical
factors.
2. Hypoactive desire: a persistent or recurrent deficiency in desire (as perceived by
the patient and/or partner, which recognizes the fact that there is a large, normal
spectrum for desire. If the patient and partner are happy with a “low” desire, then
it would not be considered hypoactive). Hypoactive desire is usually acquired,
transient and situational. Common causes of hypoactive desire: childrearing,
decreased intimacy in the relationship, social or religious teachings, unresolved
conflict in relationship, trauma/abuse. Hypoactive desire afflicts 30-40% of
women at some time in life and 15% of men. The most common probleminequality of desire between partners. More easily resolved than sexual aversion.
Sexual aversion: an extreme persistent or recurrent avoidance of sexual contact,
which is usually lifelong and generalized. Common causes: medical, substance
abuse, severe early trauma. More difficult to resolve than hypoactive desire.
*This brought up the question in lecture as to the existence of “sexual addiction”.
Dr. Racy stated that although the DSM-IV does not recognize sexual addiction as
a diagnosis, there does exist a population of people who suffer from a
“hyperactive desire”-a constant need or persistent desire for sex. There are even
groups directed at their support (sex addicts anonymous?). There is research
being done in this field regarding the psychological aspects and also the active
chemicals involved-dopamine, epinephrine, testosterone.
3. Major arousal disorders
Men:
Erectile dysfunction: inability to attain/maintain an erection to the satisfaction of
both partners. Most common complaint from men, representing ½ of all
complaints).
Primary=lifelong and generalized=never had an erection (rare)
Etiology: medical, physiological or chemical
Secondary=acquired and situational=used to have them, or still can in
some situations such as masturbation or morning erections (most
common)
Etiology: usually psychological. Very common for a temporary erectile
dysfunction to escalate into a more generalized dysfunction due to the
cycle of spectatoring and anxiety.
Women:
Female sexual arousal disorder: inability to maintain vaginal lubrication until the
sex act is completed despite adequate physical stimulation
(Dr.Racy mentioned the term “frigidity” in passing as an outdated term).
Treatment: Viagra, Cialis work for men, but not necessarily for women
Psychotherapy aimed at decreasing spectatoring and anxiety, focus on
sensation and enjoyment
4. Major orgasmic disorders
Men:
Premature ejaculation: ejaculating too soon for the satisfaction of both partners
(recognizing that this is a subjective time frame) due to a lack of voluntary
control. The second most common complaint from men (second to erectile
dysfunction). Treatment: (control tends to improve with age) behavioral changes
such as the squeeze, stop and go to gain awareness of the physical sensations of
ejaculatory inevitability and the withdrawal/pressure on the glans to inhibit
ejaculation, can also treat with SSRI’s.
Women:
Anorgasmia: inability to orgasm. More common in women (affecting 30-35% of
women) but also affects men. Common causes: childrearing, trauma, poor
relationship, poor progression (not enough foreplay), communication problems,
disease, medications (SSRI’s inhibit orgasm)
5. Two major forms of sexual pain disorder in women:
Vaginismus: painful spasm of the outer third of the vagina. Makes intercourse or
pelvic exam difficult
Dyspareunia: persistent pain associated with sexual intercourse. Much more
common in women, but can occur in men
*Dr.Racy skipped these and Dr. Moher will cover later
6. Three groups of medical conditions which lead to sexual disorders:
Heart disease: erectile dysfunction, decreased desire
Diabetes: erectile dysfunction
Spinal cord injuries: erectile dysfunction, orgasmic dysfunction, retrograde
ejaculation (into bladder)
*These will be covered by Dr. Moher later
7.
Exhibitionism: sexual gratification is obtained by revealing ones genitals to
unsuspecting women-shocking unsuspecting women
Fetishism: sexual gratification is obtained by contact with certain inanimate
objects, such as shoes or rubber sheets.
Voyeurism: sexual gratification is gained by secretly watching other people (often
with binoculars) undressing or engaging in sexual activity
Tranvestitism: Transvestic fetishism (exclusive to heterosexual men): sexual
gratification is obtained by wearing women’s clothing, particularly underclothing
Frotteurism: sexual gratification is obtained by rubbing the penis against a woman
who is not consenting or not aware
Masochism: sexual gratification is achieved by receiving physical pain or being
humiliated
Sadism: sexual gratification is achieved by giving physical pain or humiliation
Pedophilia:sexual gratification is obtained by engaging in fantasies or actual
behavior with children under the age of 14 yrs, same or opposite sex. Pedophiles
must be at least 16 years old and 4-5 yrs older than the victim. **Most common
paraphilia.
Gender identity disorder: commonly called transgender or transsexual. Patients
are physically normal with respect to their biological sex, but have a persistent
and pervasive feeling of having been born in to the wrong body-wrong sex.
Patients may take sex hormones and seek sex change surgery to correct this
mismatch. Could be caused by decreased availability of androgens in male fetus
and increased availability of androgens in female fetus. Men with GID are more
likely to have older brothers. More common for an XY to feel they are a woman
than for an XX to feel they are a man.
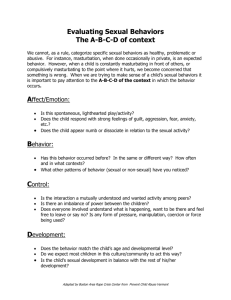
8. One way to obtain a sexual history:
Establish a comfortable relationship with patient
Allow questions to arise in the course of the clinical interview
Ask patients questions about current and past relationships
Start with general questions and proceed to specifics
Don’t be judgemental
Don’t make assumptions about sexuality
Ask “are you sexually active with men, women or both?”