Presentations of hypothalamic and pituitary disease
advertisement

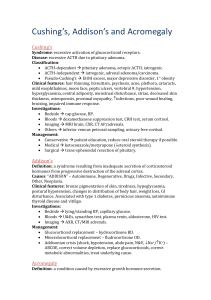
Presentations of hypothalamic and pituitary disease Pituitary space-occupying lesions and tumours Pituitary tumours (Table 16.6) are the most common cause of pituitary disease. Problems may be caused by excess hormone secretion, by local effects of a tumour, or as the result of inadequate production of hormone by the remaining normal pituitary – hypopituitarism. The great majority of pituitary tumours are benign pituitary adenomas. INVESTIGATIONS The investigation of a possible or proven tumour follows three lines. Is there a tumour? If there is, how big is it and what local anatomical effects is it exerting? Pituitary and hypothalamic spaceoccupying lesions, hormonally active or not, can cause symptoms by infiltration of, or pressure on: • the visual pathways, with field defects and visual loss • the cavernous sinus, with III, IV and VI cranial nerve lesions • bony structures and the meninges surrounding the fossa, causing headache • hypothalamic centres: altered appetite, obesity, thirst, somnolence/wakefulness or precocious puberty • the ventricle, causing interruption of cerebrospinal fluid (CSF) flow leading to hydrocephalus • rarely, the sphenoid sinus with invasion causing CSF rhinorrhoea. Investigations •Lateral skull X-ray. This may show enlargement of the fossa (Fig 16.8). Although an X-ray is now rarely requested as a definitive investigation, this remains a common incidental finding and requires further investigation. •Visual fields. These should be plotted formally by automated computer perimetry or Goldmann perimetry after confrontation at the bedside using a small red pin as target. Common defects are upper-temporal quadrantanopias and bitemporal hemianopias (see p. 1014). Subtle defects may also be revealed by delay or attenuation of visual evoked potentials (VEPs). •MRI of the pituitary. MRI is superior to high-resolution CT scanning with reconstruction (Fig 16.9). Is there a hormonal excess? There are three major conditions that may be caused by tumour or hyperplasia: • GH excess, leading to acromegaly or gigantism – these are usually acidophil adenomas, and a proportion are due to specific G-protein mutations Gs (see p. 126) • prolactin excess (prolactinoma or hyperprolactinaemia) – histologically, prolactinomas are chromophobe adenomas • Cushing’s disease and Nelson’s syndrome (excess ACTH secretion) – basophil adenomas. Occasional tumours produce both GH and prolactin. The clinical features of acromegaly and Cushing’s disease or hyperprolactinaemia are usually (but not always) obvious, and are discussed below (see pages 928, 946 and 922). Hyperprolactinaemia may be clinically ‘silent’. Tumours producing LH, FSH or TSH are very rare. Some pituitary tumours cause no clinically apparent hormone excess and are referred to as ‘nonfunctioning’ tumours, which are common and usually chromophobe adenomas. Laboratory studies such as immunocytochemistry show that these tumours may often produce LH and FSH or the subunit of LH, FSH and TSH (see Table 16.5). Studies have shown that pituitary adenomas of all types are usually monoclonal in origin. Is there a deficiency of any hormone? Clinical examination may give clues; thus, short stature in a child with a pituitary tumour is likely to be due to GH deficiency. A slow, lethargic adult with pale skin is likely to be deficient in TSH and/or ACTH. Milder deficiencies may not be obvious, and require specific testing (see Table 16.9). Differential diagnosis of apparent pituitary adenomas additionally includes craniopharyngioma, or a usually cystic hypothalamic tumour arising from Rathke’s pouch that often mimics an intrinsic pituitary lesion. Although presenting at any age, it is the most common tumour in children and is often calcified. Less common are meningiomas, gliomas, chondromas, pinealomas and carotid artery aneurysms masquerading as tumours. Secondary deposits occasionally present as apparent pituitary tumours, often presenting as diabetes insipidus. TREATMENT Treatment depends on the type and size of tumour (Table 16.7) and is discussed in more detail in the relevant sections (acromegaly, see p. 928; prolactinoma, see p. 922). In general, therapy has three aims: Removal/control of tumour Surgery via the trans-sphenoidal route is usually the treatment of choice. Large tumours are occasionally removed via the open transfrontal route. Radiotherapy is given if the tumour is incompletely removed. Radiotherapy may be by an external three-beam technique, stereotactic or rarely via implant of yttrium needles. It is usually employed when surgery is impracticable or incomplete as it rarely abolishes tumour mass. The standard regimen involves a dose of about 45 Gy, given as 20–25 fractions. Octreotide or dopamine agonists such as bromocriptine sometimes cause shrinkage of specific types of tumour. Reduction of excess hormone secretion Reduction is usually obtained by surgical removal but sometimes by medical treatment (e.g. bromocriptine or octreotide alone). Prolactinomas respond with significant tumour shrinkage to dopamine agonists (see p. 922). Acromegaly, however, responds less well (see p. 929). ACTH secretion usually cannot be controlled by medical means. Replacement of hormone deficiencies Replacement of hormone deficiencies is detailed in Table 16.10. Small tumours producing no significant symptoms, pressure or endocrine effects are observed with regular clinical, visual field, imaging and endocrine assessments. Lateral skull X-ray, showing double floor (arrows) and enlargement of the pituitary fossa in a patient with acromegaly Image loading here: a) MR image of pituitary fossa, showing tumour with suprasellar extension (b) CT scan (sagittal reconstruction), showing a pituitary tumour with suprasellar extension (arrows show upper border) Image loading here: Hypopituitarism PATHOPHYSIOLOGY Deficiency of hypothalamic releasing hormones or of pituitary trophic hormones are either selective or multiple. There are, for example, rare isolated deficiencies of LH/FSH and ACTH, some of which may be congenital, autoimmune or idiopathic in nature. Multiple deficiencies usually result from tumour growth or other destructive lesions. With the latter there is generally a progressive loss of anterior pituitary function in the order shown from left to right in Fig 16.7. GH and gonadotrophins, LH before FSH, are usually first affected. Rather than prolactin deficiency, hyperprolactinaemia occurs relatively early because of loss of tonic inhibitory control by dopamine. TSH and ACTH are usually last to be affected. Panhypopituitarism refers to deficiency of all anterior pituitary hormones; it is most commonly caused by pituitary tumours, surgery or radiotherapy. Vasopressin and oxytocin secretion will be significantly affected only if the hypothalamus is involved, either by a hypothalamic tumour or by major suprasellar extension of a pituitary lesion. CAUSES Disorders causing hypopituitarism are listed in Table 16.8. Pituitary and hypothalamic tumours, and surgical or radiotherapy treatment, are the most common. CLINICAL FEATURES Symptoms and signs depend upon the extent of hypothalamic and/or pituitary deficiencies, and mild deficiencies may not lead to any complaint by the patient. Loss of libido, amenorrhoea and impotence are symptoms of gonadotrophin and thus gonadal deficiencies, while hyperprolactinaemia may cause galactorrhoea and hypo-gonadism. GH deficiency is relatively clinically ‘silent’ except in children, though recent evidence suggests that it may cause markedly impaired well-being in adults. Secondary hypothyroidism and adrenal failure lead to tiredness, slowness of thought and action, and mild hypotension. Long-standing panhypopituitarism may give the classic picture of pallor with hairlessness (‘alabaster skin’). Particular syndromes related to hypopituitarism are considered below. Kallmann’s syndrome This syndrome is isolated gonadotrophin deficiency, which leads to hypogonadism, usually associated with anosmia (see p. 916). One sex-linked form has been shown to be due to an abnormality of a cell adhesion molecule. Sheehan’s syndrome This situation, now rare, is pituitary infarction following postpartum haemorrhage. Pituitary apoplexy A pituitary tumour may occasionally infarct or haemorrhage into itself. This may produce severe headache sometimes followed by acute life-threatening hypopituitarism. The ‘empty sella’ syndrome An ‘empty sella’ is sometimes reported on pituitary imaging. This is sometimes due to a defect in the diaphragma and extension of the subarachnoid space (cisternal herniation) or may follow spontaneous infarction of a tumour. All or most of the sella turcica is devoid of apparent pituitary tissue, but, despite this, pituitary function is usually normal, the pituitary being eccentrically placed and flattened against the floor or roof of the fossa. INVESTIGATIONS Each axis of the hypothalamic–pituitary system requires separate investigation. However, the presence of normal gonadal function (ovulatory/menstruation or normal libido/ erections) suggests that multiple defects of anterior pituitary function are unlikely. Tests range from the simple basal levels (e.g. T 4 or free T4 for the thyroid axis), to stimulatory tests for the pituitary, and tests of feedback for the hypothalamus (Table 16.9). The insulin tolerance test is now less widely used, as basal 0900h cortisol levels above 500 nmol L–1, and probably even above 400 nmol L–1, reliably indicate an adequate reserve, while levels below 100 nmol L–1 predict an inadequate response. The Synacthen test, though an indirect measure, has been advocated as an adequate indicator of hypothalamic– pituitary–adrenal status, but this remains controversial. Overall the assessment of adrenal reserve is best left in the hands of a specialist endocrinologist. TREATMENT Steroid and thyroid hormones are essential for life. Both may be given as oral replacement drugs, aiming to restore the patient to clinical and biochemical normality (Table 16.10). Sex hormone production may be replaced with androgens and oestrogens for symptomatic control; if necessary, human chorionic gonadotrophin (HCG, mainly acting as LH) and purified or biosynthetic gonadotrophins can be given if fertility is desired. Pulsatile GnRH (luteinizing hormone releasing hormone, LHRH) therapy is sometimes used where there is residual pituitary function, but it is expensive and time-consuming. GH therapy should be given if necessary in the growing child under appropriate specialist supervision. In the adult, GH therapy also produces substantial improvements in body composition, work capacity and psychological well-being in acquired GH deficiency, together with reversal of lipid abnormalities carrying a high cardiovascular risk. Although now licensed for such use in many countries, the long-term safety and efficacy of GH therapy is not yet fully established, and its cost is £2500–6000 per annum. Two important points should be noted: • Thyroid replacement should not commence until normal glucocorticoid function has been demonstrated or replacement steroid therapy initiated, as an adrenal ‘crisis’ may otherwise be precipitated. • Glucocorticoid deficiency may mask impaired urine concentrating ability, diabetes insipidus only becoming apparent after steroid replacement, the steroids being necessary for excretion of a water load. Hypothalamic releasing hormones and the pituitary trophic hormones. See the text for abbreviations and an explanation Image loading here: Weight, exercise and stress Anorexia nervosa, the ‘slimming disease’ commonly affecting young females, is associated with major functional hypopituitarism (see p. 1142). This often presents as amenorrhoea, without which the diagnosis is extremely unlikely. Anorexia is an extreme example, but more marginal degrees of underweight are a cause of secondary amenorrhoea and oligomenorrhoea, and are often unrecognized as a cause of subfertility. Similar effects are seen in female athletes undergoing heavy training with menstrual irregularity that invariably reverts to normal when training stops. Stress, though difficult to define, also affects endocrine function, especially menstruation. Emotional deprivation in childhood is an important cause of growth retardation and may be mediated by reduced GH secretion.