Tumours of pituitary gland represent approximately
10% of diagnosed brain neoplasms.
Transsphenoidal resection of pituitary brain tumours
may account for as much as 20% of all intracranial
operations performed for primary brain tumours.
Page 2
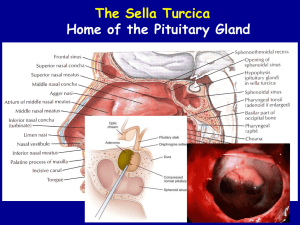
Anatomy and physiology
Pituitary pathology
Different approches for hypophysectomy
Perioperative cosiderations.
Page 3
Page 7
Antidiuretic
hormone(ADH)
Oxytocin
Pituitary adenomas can be classified into:
Microadenomas (<1 cm)
Macoadenomas(>1 cm)
Further classification :
Non functioning tumors
Functioning tumors
Page 10
More likely to be macroadenomas
Symptoms related to mass effect
Most common :
Chromophobe adenomas
Craniopharyngiomas
Meningiomas
Page 11
Excess of one or more of the anterior pituitary
hormones.
Prolactinomas followed by GH and ACTH secreting
adenomas.
Adenomas secreting thyrotropin or FSH and LH are
rare.
Page 12
Adenomas: Clinical Disease and Medical
Therapy
Page 13
Page 15
Visual function
Signs and symptoms of raised intracranial pressure
Endocrine studies; and the effects of hormonal
hypersecretion,hyposecretion
Co-morbidities, particularly
Cushing’s syndrome
CT & MRI
Page 16
in
acromegaly
or
Page 17
Mass effect
Page 18
Prolactinomas are the most frequently observed type
of hyperfunctioning pituitary adenoma
Represent 20%–30% of all clinically recognized
tumours.
More than 90% of patients respond to medical
therapy with a dopamine agonist such as
bromocriptine and thus few patients present for
surgery
Page 19
Affected area
Clinical features
Face
Increase in size of skull and supraorbital ridges; enlarged lower
jaw; increase in spacing between teeth/malocclusion
Hands and feet
Spade-shaped; carpal tunnel syndrome
Mouth/tongue
Macroglossia; thickened pharyngeal and laryngeal soft
tissues; obstructive sleep apnoea
Soft tissue
Thick skin; doughlike feel to palm
Skeleton
Vertebral enlargement; osteoporosis; kyphosis
Cardiovascular Hypertension; cardiomegaly; impaired left ventricular
function
Endocrine
Impaired glucose tolerance; diabetes
Other
Arthropathy; proximal myopathy
Page 20
Page 21
Affected area
Appearance
Clinical features
Redistribution of body fat ’moon face’ truncal obesity or buffalo
obesity
Muscloskeletal proximal myopathy, Osteoporosis (increases risk of
fractures during positioning),vertebral collapse.
Soft tissue
Skin fragility with easy bruising (cannulation difficult),
hirsutism ,acne.
Metabolic
Hypernatremia, hypokalemia, alkalosis.
Cardiovascular hypertensive; ischemic heart disease and left ventricular
hypertrophy are also common.
Endocrine
diabetes
Other
Sleep apnea; Immunosuppression and coexisting infection,
gastroesophageal reflux, renal stones, mental problems.
Page 22
Page 23
Low levels of peripheral hormones, not associated with high
pituitary tropic hormones.
Pituitary apoplexy: present with sudden headache, loss of
vision, loss of consciousness and panhypopituitarism,
requiring urgent surgery.
Requires glucocorticoid replacement
Thyroxine replacement is also required (50–150 ug daily).
Perioperatively, these patients are extremely sensitive to
anaesthetic agents, and pressor agents may be needed to
maintain blood pressure.
Page 24
Multiple endocrine neoplasia (MEN) syndromes
MEN I (Werner)
Parathyroid hyperplasia
Pituitary adenoma
Pancreatic islet cell tumors
MEN IIA
Parathyroid hyperplasia
Medullary thyroid carcinoma
Pheochromocytoma
MEN IIB
Parathyroid hyperplasia
Medullary thyroid carcinoma
Pheochromocytoma
Ganglioneuromatosis
Marfanoid habitus
Page 25
Page 26
General issues :
Optimization of cerebral oxygenation
Maintenance of hemodynamic stability
Provision of conditions that facilitate surgical exposure
Prevention and management of intraoperative complications
Rapid, smooth emergence.
Page 27
Surgical Approach
The pituitary fossa can be approached using
transsphenoidal, transethmoidal or transcranial route
the
The transsphenoidal route is preferred for all but not the
largest of tumours
Transsphenoidal access to the pituitary fossa is obtained
using a sublabial or endonasal approach
Page 28
Transsphenoidal Approach
Advantages
•Decreased diabetes insipidus.
• Magnified visualization.
•Decreased
frequency
of
transfusions
•For pituitary tumors that have
significant suprasellar extension
blood •Less surgical stimulation
Disadvantages
• CSF leakage and meningitis ,
• Inability to visualize neural structures
adjacent to a large tumor,
• Possibility of bleeding from cavernous
sinuses or carotid.
Page 29
Transcranial Approach
•Incidence of permanent diabetes
insipidus and anterior pituitary
insufficiency is increased.
•Damage to the olfactory nerves, frontal
lobe vasculature, and optic nerves and
chiasma
Hormone replacement
Preoperative hormone replacement therapy should be
continued into the operative period
In general, All patients with Cushing’s disease require
glucocorticoid cover.
Page 30
Pituitary adenoma for surgery
0800 hours cortisol and short ACTH 1–24 (synacthen)
Normal
Abnormal
(cortisol >550 nmol/L)
No Perioperative Glucocorticoid
Cover
The patient should be given
supraphysiological glucocorticoid cover
for 48 h
•Hydrocortisone 50 mg i.v. 8-hourly on day 0
• 25 mg i.v. 8-hourly on day 1
• 25 mg i.v. at 0800 hours on day 2
cortisol 0800 hours cortisol for 1-3 d
Page 31
0800 hours cortisol for 3-6 d
0800-h Cortisol level (nM)
<100
100–250
250–450
10–20 mg,
single morning dose
Stress only,
>450
0800-h Cortisol level
Day 7
<350 nM >350 nM
ITT or metyrapone
10-14 d or 4-6 wks
15–30 mg/d
Page 32
(maintenance)
Abnormal
Normal
No replacement
General Endotracheal Anesthesia
Is Indicated.
Airway management.
Anesthetic techniques
Operative techniques
Intraoperative complications.
Emergence and recovery
Page 33
Page 34
Four grades of airway involvement:
Grade 1-- no significant involvement
Grade 2-- nasal and pharyngeal mucosa hypertrophy but
normal cords and glottis
Grade 3-- glottic involvement including glottic stenosis or
vocal cord paresis
Grade 4-- combination of grades 2 and 3, i.e. Glottic and soft
tissue abnormalities
Page 35
Airway management and tracheal intubation proceed
uneventfully in the majority of patients if large face masks and
long-bladed laryngoscopes are used
Fibreoptic intubation should be considered in patients in
whom difficult airway management is predicted
Intubating laryngeal mask airway has also been used
successfully
Equipment for tracheostomy should be available if airway
changes are advanced (recommended for grades 3 and 4)
Page 36
Reinforced orotracheal tube is recommended.
Positioned in the left corner of the mouth
Throat pack is then inserted.
Prevent bleeding into the glottic region during surgery, but also
entry of blood and secretions into the stomach which may
precipitate postoperative vomiting
Page 37
Standard Monitors
Page 38
Supine
Head elevated
Patient closer to the right
hand side of the table
Neck tilted laterally to the
left, slightly extended and
secured in a mayfield clamp.
Page 39
Page 40
Agents: lignocaine with adrenaline
For suppressing the hemodynamic response to nasal
infiltration with adrenaline-containing solutions:
Labetolol,
Alpha-antagonists (such as phentolamine),
Beta-blockers
Vasodilators (such as nitroglycerin or sodium nitroprusside).
Deepening anesthesia or blousing a shortacting, potent
opioid (such as alfentanil or remifentanil)
Bilateral maxillary nerve blocks
Page 42
Transsphenoidal Approach to the Sella Turcica for
Pituitary Surgery
Anesthetic Technique
Inhaled agents sevoflurane, desflurane and isoflurane have
all been shown to increase lumbar CSF pressure.
Whether an inhalational or intravenous technique is
employed, short-acting agents should be utilised to facilitate
rapid recovery
Postoperative Airway Maintenance Is An Issue
Page 45
Analgesia
Short-acting, potent opioids, such as Remifentanil.
Longer acting opioids (towards the end of surgery).
Paracetamol
Non-steroidal anti-inflammatory drugs (postoperative
haematoma)
Tramadol (less effective and more sedation)
Page 46
Controlled hypercapnia (to a maximum PaCO2 of 60
mmHg). However, it is preferred to maintain highnormocapnia (40–45 mmHg).
Lumbar cerebrospinal fluid catheter. a forced
Valsalva can often be sufficient.
Typical neuroanesthetic maneuvers designed to reduce
ICP in these cases because they make the pituitary
retreat upward out of the sella
Page 47
Venous air embolism
Aspiration of air from a multi-orifice air aspiration catheter (if
in situ).
Administration of 100% oxygen
Application of internal jugular vein pressure bilaterally
Saline irrigation of the wound.
Haemostasis of open vessels are crucial
Page 48
Hemorrhage from carotid artery damage.
Pseudo-aneurysm and carotid-cavernous fistula
formation .
Page 49
Smooth and rapid emergence from anaesthesia is
essential to allow early neurological assessment and
maintenance of stable respiratory and
cardiovascular variables.
At the completion of surgery, the oropharynx should also be
suctioned meticulously.
Removal of pack
Page 50
Patients with a history of OSA
Oral airway to facilitate mouth breathing,
A nasopharyngeal airway can also be placed under direct
visualization by the surgeons before the nose is packed
patients prone to upper airway obstruction may
Tracheal extubation in a seated position.
Page 51
Page 52
Cranial nerve dysfunction
Immediate assessment of visual acuity, visual fields,
and extraocular motility.
CT and MRI.
Rexploration.
Page 53
CSF leakage
Rhinorrhea, continuous fluid leakage exacerbated by
leaning forward, associated with headache
τ-transferrin
Operative repacking of the defect with autologous fat
Page 54
Nausea and Vomiting
Prophylactic antiemetic
Page 55
Disorders of Water Balance
DI
Page 56
SIADH
Failure of ADH release from the posterior pituitary.
Hallmark of DI is dilute urine in the face of hypertonic plasma.
Aqueous vasopressin (5 units sc every 4h)
Vasopressin in oil (0.3 ml IM per day)(cause water
intoxication)
Desmopressin (DDAVP),
• A synthetic analogue of ADH
• 12-to 24-hour duration of action,
• intranasal preparation (5-10 mg qd or bid)
• Used both in the ambulatory and perioperative settings,
Page 57
Page 58
Page 59
Patients undergoing pituitary surgery can present a host of
anaesthetic challenges.
Transsphenoidal approach is associated with specific issues
the anaesthetist must anticipate and manage.
Page 61
Page 62
The following are features of Cushing’s syndrome:
Hypokalaemia
Osteoporosis
Hypertension
Peptic Ulceration
Muscle Weakness
Page 64
The following are features of Cushing’s syndrome:
Hypokalaemia
Osteoporosis
Hypertension
Peptic Ulceration
Muscle Weakness
Page 65
Concerning advantages of transphenoidal approach
over transcranial approach:
Decreased diabetes insipidus.
Magnified visualization.
Decreased frequency of blood transfusions
Less surgical stimulation
Page 66
Concerning advantages of transphenoidal approach
over transcranial approach:
Decreased diabetes insipidus.
Magnified visualization.
Decreased frequency of blood transfusions
Less surgical stimulation
Page 67
Hypophysectomy will result in:
Depressed Thyroid Function
Osteoporosis And Generalised Wasting
The Secretion Of Adrenal Glucocorticoid And Sex Hormones
To A Low Level
Diabetes Insipidus
Normal Aldosterone Secretion
Page 68
Hypophysectomy will result in:
Depressed Thyroid Function
Osteoporosis And Generalised Wasting
The Secretion Of Adrenal Glucocorticoid And Sex
Hormones To A Low Level
Diabetes Insipidus
Normal Aldosterone Secretion
Page 69
Diabetes inspidus results in
Hypernatremia
High plasma osmolarity
High urine flow
High urine osmolarity
Page 70
Diabetes inspidus results in
Hypernatremia
High plasma osmolarity
High urine flow
High urine osmolarity
Page 71
Page 72