Hasan AYDIN, MD
Endocrinology and Metabolism
Yeditepe University Medical Faculty
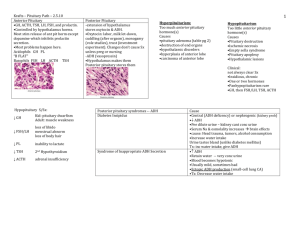
The
deficiency (hypo) of one or more hormones
of the pituitary gland
Deficiency of one or multiple hormones of the
anterior pituitary …….-hypopituitarism
Deficiency of the posterior lobe …..-central
diabetes insipitus
Deficiency of all pituitary hormones….panhypopituitarism
Either result from hypothalamus or pituitary
Symptoms and signs frequently protean and
nonspecific
Abnormalities in electrolyte levels,
Altered mental status,
Abnormal glucose levels,
Altered body temperature,
Increased heart rate
Patients at risk of developing hypopituitarism
Traumatic brain injury (TBI),
Cocaine use,
Subarachnoid hemorrhage,
Postpartum hypotension (Sheehan syndrome).
76% tumor or treatment of tumor
Mass effect of adenoma on other hormones
Surgical resection of non-adenomatous tissue
Radiation of pituitary
13% extrapituitary tumor
Craniopharyngioma
8% unknown
1% sarcoidosis
0.5% Sheehan’s syndrome
In
US
Prevelance of pituitary adenoma 10-20%
Hypopituitarism 2-8/100,000 persons/year
World
Incidence of 4.2 cases per 100,000 per year
Prevalence of 45.5 per 100,000 without gender
difference
Missed or delayed diagnosis could potentially lead to
permanent disability or death
Female patients with hypopituitarism have more
than a 2-fold increase in cardiovascular mortality
Cardiovascular disease is significantly higher among
hypopituitary patients (incidence ratio, 3.7; 95%
confidence interval)
Hypopituitary patients have lower high-density
lipoprotein cholesterol and higher low-density/highdensity lipoprotein ratio
Primary pituitary disease
Tumors
Pituitary surgery
Radiation treatment
Hypothalamic disease
Functional suppression of axis
Exogenous steroid use
Extreme weight loss
Exercise
Systemic Illness
Interruption of the
pituitary stalk
Extrasellar disorders
Craniopharyngioma
Rathke pouch
Developmental and
genetic causes
Dysplasia
Septo-Optic dysplasia
Developmental
hypothalamic dysfunction
Kallman Syndrome
Laurence-Moon-BardetBiedl Syndrome
Frohlich Syndrome (Adipose
Genital Dystrophy)
Acquired causes:
Infiltrative disorders
Cranial irradiation
Lymphocytic hypophysitis
Pituitary Apoplexy
Empty Sella syndrome
Hypothalamic dysfunction and hypopituitarism
may result from dysgenesis of the septum pellucidum or
corpus callosum
Affected children have mutations in the HESX1 gene
These children exhibit variable combinations of:
cleft palate
syndactyly
ear deformities
optic atrophy
micropenis
anosmia
Pituitary dysfunction
Diabetes insipidus
GH deficiency and short stature
Occasionally TSH deficiency
Defective hypothalamic gonadotropin-releasing
hormone (GnRH) synthesis
Associated with anosmia or hyposmia due to olfactory
bulb agenesis or hypoplasia
May also be associated with: color blindness,
optic atrophy, nerve deafness, cleft palate,
renal abnormalities, cryptorchidism
GnRH deficiency prevents progression
through puberty
Characterized by
low LH and FSH levels
low concentrations of sex steroids
Males patients
Delayed puberty and hypogonadism, including micropenis
Long-term treatment:
human chorionic gonadotropin (hCG) or testosterone
Female patients
Primary amenorrhea and failure of secondary sexual
development
Long-term treatment:
cyclic estrogen and progestin
Repetitive GnRH administration restores normal puberty
Fertility may also be restored by the administration of
gonadotropins or by using a portable infusion pump to
deliver subcutaneous, pulsatile GnRH
Rare autosomal recessive disorder
Characterized by mental retardation; obesity;
hexadactyly, brachydactyly, or syndactyly
Central diabetes insipidus may or may not be
associated
GnRH deficiency occurs in 75% of males and half of
affected females
Retinal degeneration begins in early childhood
most patients are blind by age 30
A broad spectrum of hypothalamic lesions
hyperphagia, obesity, and central hypogonadism
Decreased GnRH production in these patients results in
attenuated pituitary FSH and LH synthesis and release
Deficiencies of leptin, or its receptor, cause these clinical
features
Infiltrative disorders
Cranial irradiation
Lymphocytic hypophysitis
Pituitary Apoplexy
Empty Sella syndrome
Etiology
Presumed to be autoimmune
Clinical Presentation
Women, during postpartum period
Mass effect (sellar mass)
Deficiency of one or more anterior pituitary hormones
Diagnosis
ACTH deficiency is the most common
MRI - may be indistinguishable from pituitary adenoma
Treatment
Corticosteroids – often not effective
Hormone replacement
Patoloji
Radyoloji
Hemorrhagic infarction of a pituitary
adenoma/tumor
Considered a neurosurgical emergency
Presentation:
Variable onset of severe headache
Nausea and vomiting
Meningismus
Vertigo
+/ - Visual defects
+/ - Altered consciousness
Symptoms may occur immediately or may develop
over 1-2 days
Risk factors:
Usually resolve completely
Transient or permanent hypopituitarism is possible
Diabetes
Radiation treatment
Warfarin use
undiagnosed acute adrenal insufficiency
Diagnose with CT/MRI
Differentiate from leaking aneurysm
Treatment:
Surgical - Transsphenoid decompression
Visual defects and altered consciousness
Medical therapy – if symptoms are mild
Corticosteroids
Radiology
Infarction of pituitary after substantial blood loss
during childbirth
Incidence: 3.6%
No correlation between severity of hemorrhage and
symptoms
Severe: recognised days to weeks PP
Lethargy, anorexia, weight loss, unable to breast feeding
Typically long interval between obstetric event and
diagnosis
Of 25 cases studied:
50% permanent amenorrhea
The rest had scanty-rare menses
Most lactation was poor to absent
Dx: MRI empty sella turcica
Often an incidental MRI finding
Usually have normal pituitary function
Implying that the surrounding rim of pituitary tissue is fully
functional
Hypopituitarism may develop insidiously
Pituitary masses may undergo clinically silent infarction
with development of a partial or totally empty sella by
cerebrospinal fluid (CSF) filling the dural herniation.
Rarely, functional pituitary adenomas may arise within
the rim of pituitary tissue, and these are not always
visible on MRI
Can present with features of deficiency of one or
more anterior pituitary hormones
Clinical presentation depends on:
Age at onset
Hormone affected, extent
Speed of onset
Duration of the deficiency
Radiology
Women
Oligomenorrhea or
amenorrhea
Men
Loss of libido
Erectile dysfunction
Infertility
Loss of secondary sex
characteristics
Atrophy of the testes
Gynecomastia (testosterone
deficiency)
Loss of libido
Vaginal dryness or
dyspareunia
Loss of secondary sex
characteristics (estrogen
deficiency)
Results in hypocortisolism
Pale complexion
Malaise
Anorexia
Weight-loss
Gastrointestinal disturbances
Hyponatremia
Unable to tan or maintain a tan
No features of mineralocorticoid deficiency
Aldosterone secretion unaffected
Hypothyroidism
Atrophic
thyroid gland
Inability
Often
to lactate postpartum
1st manifestation of Sheehan syndrome
Adults
Often asymptomatic
May complain of
Fatigue
Degrees exercise tolerance
Abdominal obesity
Loss of muscle mass
Children
GH Deficiency
Constitutional growth delay
Biochemical
insufficiency
diagnosis of pituitary
Demonstrating low levels of trophic hormones in
the setting of low target hormone levels
Provocative
tests may be required to assess
pituitary reserve
Basal
ACTH secretion
Cortisol < 3 μg/dL, cortisol deficiency
Cortisol > 18μg/dL, sufficient ACTH
Cortisol > 3 μd/dL but < 18 μg/dL - test ACTH reserve
ACTH
Metyrapone test (750 mg q 4hr for 24 hrs)
Cortisol < 7 μg/dL, 11-deoxycortisol > 10 μg/dL
ITT ( 0.1 U/kg BW)
reserve
Cortisol > 18 μg/dL, normal
Cosyntropin stimulation test
Cortisol > 18 μg/dL, normal
Serum
TSH
T4 should be measured
may not be helpful
MEN
Testosterone low, LH normal or low
Sperm count
WOMEN
LH-FSH, E2, vaginal cytology, response to
medroxyprogesterone 10 mg qd for 10 days
Peak
GH response < 5 ng/ml
ITT
Arginine ( 0.5 g/ kgBW i.v.)
L-DOPA ( 0.5 g orally )
Clonidine ( 0.15 mg orally )
Glucagon ( 0.03 μg/kg BW s.c. + 40 mg propranolol )
Cortisol deficiency ( 5 - 2.5 mg prednisone qd)
Levothyroxine ( 0.075 -0.15 mg qd )
Gonadal steroids (E2 ,P, Testosterone)
Growth hormone
Vasopressin (desmopressin 10 μg x 2)
Hormone
replacement therapy
usually free of complications
Treatment
regimens that mimic physiologic
hormone production
allow for maintenance of satisfactory clinical
homeostasis
Trophic Hormone Deficit
Hormone Replacement
ACTH
Hydrocortisone (10-20 mg A.M.; 10 mg P.M.)
Cortisone acetate (25 mg A.M.; 12.5 mg P.M.)
Prednisone (5 mg A.M.; 2.5 mg P.M.)
TSH
L-Thyroxine (0.075-0.15 mg daily)
FSH/LH
Males
Testosterone enanthate (200 mg IM every 2 wks)
Testosterone skin patch (5 mg/d)
Females
Conjugated estrogen (0.65-1.25 mg qd for 25days)
Progesterone (5-10 mg qd) on days 16-25
Estradiol skin patch (0.5 mg, every other day)
For fertility: Menopausal gonadotropins, human
chorionic gonadotropins
GH
Adults: Somatotropin (0.3-1.0 mg SC qd)
Children: Somatotropin [0.02-0.05 (mg/kg per
day)]
Vasopressin
Intranasal desmopressin (5-20 ug twice daily)
Oral 300-600 ug qd