MHNMI submission on Maintaining Five points of entry to the
advertisement

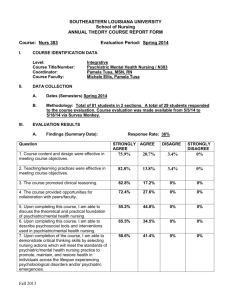
Mental Health Nurse Managers Ireland MENTAL HEALTH NURSE MANAGERS, IRELAND. Submission re: An Examination of the rationale for and Impact of Maintaining Five points of entry to the register of Nurses. Introduction Mental Health Nurse Managers Ireland (MHNMI) acknowledge the increasing pressure on the Psychiatric Nursing Profession in attracting nursing students onto the pre registration nursing programme. This is a challenge that the profession continues to address. We see this problem primarily as one of misunderstanding in relation to the non-quantifiable primary functions of the Psychiatric Nurse. Indeed research in mental health nursing has experienced difficulty conforming to the norms of traditional quantitative research, (Baier 1989). In order for this challenge to be addressed we believe that the separate register for the registration of psychiatric nurses is an important aspect of the professional status of psychiatric nursing in Ireland. We have set out below a number of arguments and related literature to support this position and we would hope that these would be considered carefully in any future decisions on the registration of nurses in Ireland. In Europe, Ireland, the United Kingdom and Belgium differ from other countries in that entry to pre-registration nurse education exists for discrete branches of nursing. Currently in Ireland there are five points of direct entry to pre-registration education, including psychiatric nursing. Elsewhere, the integration of pre-registration nurse education into the third level sector has resulted in the wide-scale adoption of a generalist approach. However, the evidence to support which model, whether specialist or generalist, best serves the public and profession in preparing safe and competent practitioners, is lacking. 2 Education Currently, the majority of countries in the developed world have adopted the generalist approach to pre-registration nursing education, thereby following the World Health Organizations recommendation that; “all basic programs of nursing education be restructured, reoriented, and strengthened, in order to produce generalist nurses” (WHO 1988). However, the use of a generic model while advantageous in some respects, has been identified as flawed in that its use in psychiatric nursing has resulted in many insurmountable difficulties in providing students with adequate theoretical and practice experiences (Delacour and Curry 1991, p.155). The MHNMI believe that an educational course can be committed to the knowledge, skills and attitudes required by the psychiatric nurse. A course that is dedicated to a single registration can be more focused better equipped to produce nurses that can meet the needs of this group within society. In the UK, the Report of the Mental Health Nursing Review Team, (1994) argues that the essential focus of the mental health nurse must lie in working with people with serious or enduring mental illness in secondary and tertiary care, regardless of setting. Belcher and Fish, (1995) argue that a “therapeutic healing ethos grounded in the interpersonal” is the essence of psychiatric nursing while Barker, (1989) advocates the active engagement of the nurse with the raw human material as fundamental. There is an argument that nurses’ training has not helped because it failed to provide nurses with the skills to engage patients in therapeutic relationships. The ‘Review Group On Community Psychiatric Nursing’ (Local Government Staff Negotiations Board, 1983) recommended that all nurse training be community orientated and in 1984 An Bord Altranais established a special 3 committee to prepare a new programme of training. The new programme was introduced in 1986, aimed at enabling the student psychiatric nurse to be competent to practice as a psychiatric nurse, in acute care areas, long stay areas, and in the community (Gilheaney and Farrelly, 1993). The preregistration training Programme for Psychiatric Nurses (An Bord Altranais, 1986) had a fourteenweek allocation to Community Nursing Services and following this development the post registration orientation courses to community psychiatric nursing were discontinued (Treacy, 1987). This was reflective of under-investment in nurse education at a post-graduate level and many nurses in the field of psychiatry had to seek other avenues of post-graduate education that was not necessarily focused on therapeutic interventions. McCardle (2003) noted a wide range of postgraduate education and skills development among community mental health nurses in Ireland and concluded that the size of the nurse’s caseload and the lack of focused post-graduate development had a greater effect on the level of therapeutic intervention than the initial nurse training. Savage (1998) voices concern about the diverse systems of nurse education, which she maintains compare unfavourably with other professions. Her major concern is the absence of a unified system of nurse education that is grounded in the disciplinary knowledge of nursing. Furthermore she argues that the traditional option of providing four points of entry to the nurses Register is declining throughout Europe and is obsolete in the USA, Canada, Australia and New Zealand. This argument is based on the assumption that a single point of entry can best meet the needs of the profession and the community. The supportive argument that we should move to a unified entry system because other places are doing so is a poor rationale and merely highlights the dearth of available evidence to support such a change of system. Indeed there is some evidence from elsewhere to suggest that the single registration system has been detrimental to psychiatric nursing. 4 According to Delacour and Curry (1991) since the commencement of generic programs in Australia; “psychiatric and mental handicap nursing have been devalued and seriously marginalised; in general terms, they operate currently with impossibly conflated and unworkable curricula; the benefits in regard to division of curricular hours have been conferred, in the main, on general nursing…Generally, psychiatric nursing tends to attract less than 15% of theoretical nursing hours, compared with the common 75% conferred on general nursing…general nursing clinical hours tend to exceed psychiatric nursing clinical hours by more than 5 fold” (Delacour & Curry 1991, p.153). Burdekin (1993) claims that the outcome of this is a loss of speciality skills and an inability of graduates to function satisfactorily in psychiatric practice areas. This would have major impacts in relation to patient care. It would appear that this problem exists due to over loading within the curriculum, and to an on going problem of defining and placing psychiatric content in the curriculum. This is according Hipps (1981), because integration involves focusing on generalizations, as opposed to specifics (Hipps, 1981, p.976). Furthermore, there appears to be a lack of understanding about the differences between psychosocial and psychiatric aspects of patient care. A survey of Universities in New South Wales, by Baume (1992), found that some generic programs were non-specific in identifying the psychiatric nursing components of their course resulting in students being primarily exposed to nonpsychiatrically ill patients, and focused on psychosocial, rather than psychiatric, concepts of 5 practice. Emphasis upon psychosocial concepts, whilst effective in learning aspects of care such as empathy, communication and observational skills, will do little however to identify psychiatric disorders. Nor, will this allow students to gain experience in developing interventions to help the person with active psychopathology (Delacour and Curry 1991, p.156). The MHNMI take the view that having a separate register does not negate the delivery of common core modules within a curriculum as much of the subject area that is common to the various nursing disciplines may also be common to other health professionals such as occupational therapists or social workers. Indeed it could be argued that psychiatric nursing has more in common with other health care disciplines in areas such as the behavioural sciences and psychology than it has with general nursing since the latter is still heavily dependent on the biological sciences. There is little evidence to suggest that a generic model of nursing education will enhance the patient care of the more marginalized groups in our society. Assumptions underpinning the generic model are 1. That as students have the capacity to learn to differentiate, integrate and generalize from knowledge, concepts of practice can be taught in any setting. Therefore, it is asserted that psychiatric nursing can be taught in non-psychiatric settings (Delacour and Curry 1991, p.154). 2. That upon graduation, generic nurses will be able to transfer skills acquired in nonpsychiatric areas to psychiatric settings should they choose to do so. This assumption also implies that mental health problems in medical or surgical populations differ only in degree from the mental health problems experienced by the psychiatric population. 6 3. That discipline maturity occurs post registration and that generic preparation will enable graduates to emerge sufficiently well equipped to withstand the pressures applied, when they embark upon a post registration course in psychiatric nursing. These assumptions are made despite a paucity of research addressing the nature and extent of emotional disturbance experienced by patients in general settings, or the similarities and differences between counselling and interpersonal skills in psychiatric and general nursing settings. Neither has the transfer of knowledge and skills between settings been fully researched. It is difficult then to imagine how an over-reliance on general environments for exposure to psychiatric aspects could possibly compensate for the potential benefits of a separate psychiatric course supported by specialist clinical experience. The few studies which have been done confirm that the ‘any concept in the any setting’ principle is easier to discuss theoretically than to operationalise in practice. Functional Difficulties It could be argued that having five registers creates the possibility of an individual being removed from practicing on one register (e.g. RPN) but allowed to remain on another (e.g. RGN) as no misdemeanor occurred in relation to the latter. One solution to this possibility would be reducing the register to one with five branches but an alternative solution may be to link the registers within legislation to clarify that removal from one register automatically also applies to all five registers. The same would apply to anyone removed from one register not being allowed to train within another discipline of the register. An Bord Altranais is empowered with internal control of nursing through self-regulation and therefore is obliged to assure high quality nursing care through the continual formulation and updating of standards of practice and education. Consequently it is incumbent upon An Bord Altranais to put mechanisms in place to effectively manage this scenario 7 and the MHNMI do not feel that the single register option is necessarily the best mechanism to achieve this. Career Choices. A single nursing register with separate specialist branches allows for the possibility of a common core curriculum whereby the students could make their career choice after some initial experience. The logistics of allowing a group of students (100) commence a generic nursing course with the option of branching to specific registration after a period of time (18-24mths) are extremely difficult. Different registration options in a particular college will have a different and finite number of places available due to issues such as placement opportunities. How will it be managed if all 100 wish to enter the same register and the places are unavailable? The generic scenario is also open to influence whereby tutors from different registers attempt to attract the better quality students to their specialism or clinical staff are unpleasant towards students that are perceived unfavourably in the hope that they will join an alternative register. This is an issue that seems implausible but one that some members of the MHNMI have experienced personally while working in the UK. An argument progressed in support of this option is that the students are making better informed choices as they will have more information. This argument holds two assumptions, firstly they have more information, which is true to a point and secondly that they are better informed. The problem with the latter assumption is that a little knowledge is a dangerous thing and the students are basing their decisions on one or two placements and the theory up to that point. The pleasant or otherwise experience of one or two placements may well be an unrealistic perception on which to base a career path but this is the likely outcome of this approach to entering the register. Breust, 8 (1989) indicates that many countries have reported a drop in the enrolment of student nurses at basic level and an even greater reduction in the number of students indicating a preference for psychiatric nursing either immediately upon graduating from basic programmes or choosing to study it at higher level. In addition, he extrapolates from available data and concludes that; changes in the mental health services and treatments and the placement of patients in the community setting have led to role diffusion, creating uncertainty about what the future will hold for the psychiatric nurse, unpleasant student experiences in the clinical setting, remaining social prejudice and fearful, lack of effective psychiatric nurse role models discourage students from choosing the career, health personnel shortages with understaffed units in the institution and large client case loads in the community setting resulting in difficulties in maintaining standards of nursing care leading to professional frustration and burn out, students become aware that the career structure and other incentives in the field are inadequate or lacking, continuing education opportunities are limited. Recruitment There was a recruitment difficulty within psychiatric nursing during the mid to late1990s that has been well documented. This was due in no small part to the reduction in student numbers throughout the 1980s and early 1990s effectively removing psychiatric nursing as a career option over much of the country. The inevitable effect of this policy was a steady decline in the numbers of applicants for psychiatric nurse training as noted by Wells et al, (2000) who predict serious implications for service provision and work force planning, as the workforce matures. Appleby and Brewins, (1992) also highlighted the traditional pattern of male recruits into psychiatric nursing 9 appeared to be in decline, a trend supported by other papers (Commission on Nursing, 1998, Wells et al, 2000, Wells and McElwee,2000). This situation is not explained by imperfect information given to school-leavers or the inability of school-leavers to differentiate between psychiatric and general nursing according to Wells and McElwee, (2000). The observation that the sustained decline in the recruitment to psychiatric nursing programmes in the 1990’s appeared to parallel a robust increase in applicants to social care courses was made by Wells and McElwee, (2000). The MHNMI would note that this is a difficulty that we have been able to address effectively. The maintenance of the separate register has allowed us to approach the issue as an individual group and promote psychiatric nursing at grass roots level. Anecdotal evidence from the nursing careers centre in An Bord Altranais would suggest that the competition for places in psychiatric nursing has increased since the 2000 intake with an increase in the points required for entry in almost all courses of psychiatric nursing nationally. The workforce planning difficulties are also being addressed as the number of places in the same period has increased from 256 to 343. This amounts to an increase of 33% which is larger than any other nursing cohort. Maintaining separate registers to date has had the advantage that the different disciplines have been able to adjust the entry criteria to suit the needs of the discipline. For example psychiatric nursing has been able to lower the points and increase the mature student proportion of the intake to fill the places and there is evidence to suggest that this has worked well for this discipline. Higher social skills and an increased level of maturity have been qualities that have been promoted within psychiatric nursing as opposed to a high points entry reflecting a high academic ability but with perhaps a reduced social skills or maturity. 10 Identity Nolan, (1993) argues that the history of a discipline is important because it brings clarity to a social phenomenon and confers legitimacy to the services provided by that discipline. The MHNMI feel that the individual distinctiveness of a group of staff with identity in common is an important issue within an organisation. A strong identity can be a driving force when issues required to be progressed. A strong identity also allows cohesive groups to form and provide leadership and defense of the professional field of practice. A strong identity provides a clarity of role and practice and is an important basis for issues such as recruitment and specialisation. Nolan, (1993) argues that the history of a discipline is important because it brings clarity to a social phenomenon and confers legitimacy to the services provided by that discipline. Psychiatry has developed a diverse group of specializations such as CBT, Family therapists, Addiction counselors, Generic counselors etc. that have not occurred in other fields. These specializations are different from many of those in other disciplines in that they are not medically based and dominated in the way that CNS in renal or CNS in respiratory etc. are within the field of general nursing. This has created a psychosocially diverse basis to the curriculum model within psychiatric nursing that is not available in the other disciplines with their heavy emphasis on the biological sciences and attachment to the medical model. Legitimate Practice The discourse from the literature appears to suggest that confusion exists between the skills of the psychiatric nurse and those of other professionals Nolan, (1993), Burnard, (1989). However, McCardle (2003) noted that the CMHN and the medical staff were the two disciplines that existed in all mental health teams nationally. Other health professionals such as social workers or occupational therapists have not been easy to replace and when a vacancy existed in an area for a 11 social worker or an occupational therapist the legitimate role boundary of the CPNs expanded to meet the needs created by the vacancy. It would be easy to be critical of this practical support and multi agency adaptability as being beyond the boundary of legitimate professional nursing practice or falling within non-nursing duties. Alternatively, this aspect of patient care could be a good example of the whole being greater than the sum of the parts. The action of undertaking practices that could be deemed beyond the legitimate role boundary may have little direct therapeutic value but significantly impact upon the building of a trusting relationship and delivering patient centred care, (McCardle 2003). Barker, (1989) claimed that psychiatric nursing was not therapeutically active until comparatively recently and his conclusion that it remained in the shadows of a medical model of care is a credible deduction given the historical evidence. Cusack, (2001) analysed the role of the advanced practitioner of psychiatric nursing and confirmed that for the most part of the twentieth century custodial care in large institutions was the preferred treatment modality. The medical model proscribed independent nursing actions and restricted nurses from developing therapeutic relationships with patients Canavan,( 2002), which it deemed the preserve of the medical staff and the psychiatrist. Hence it is not surprising that many psychiatric nurses feel disenfranchised and alienated within the institutional setting. The mental health service in Ireland, as a consultant led service, differs markedly from many other services reported in the literature, as many of these appear to have moved to a CMHT service wherein the consultant is a senior clinician and the service is led by a manager, from any of the health professions (McCardle 2003). However, the MHNMI would argue that this model of care is changing. Bannon and McDonald (2003) noted that a CMHT approach was set up in Cavan, Ireland in early 2000 with the aim of delivering home-based treatment to replace hospital care. Within this 12 model, patients come through a team co-ordinator and were accepted for home-based treatment following joint assessment with the psychiatrist (Bannon and McDonald, 2003). Overall Bannon and McDonald (2003) noted that the service users positively appraised home-based treatment and studies of this nature are likely to strengthen the argument for a CMHT approach to care in Ireland. The MHNMI believe that if the role of psychiatric nurses in Ireland is to be maintained and expanded then the register must be preserved. Canavan, 2002) proposed that the challenge for the profession is to determine whether the knowledge base can be considered suitably credible as a blueprint for the delivery of nursing care in the 21st century. With a separate register affords the possibility of asking ‘What is psychiatric nursing and how can the role be developed?’ as opposed to asking ‘What is nursing?’ and developing practice from a more generic basis. Conclusion The MHNMI feel that the separate register of psychiatric nursing must be maintained if we are to progress and develop as a professional discipline within the field of mental health. It in not sufficient to argue that we in Ireland should change our structures merely because other countries are doing so. This would amount to change for changes sake and we believe that change should be based on empirical evidence and in the interests of both the patient and the profession. The maintenance of the psychiatric nursing register affords the profession independence in relation to future recruitment, educational developments and practice developments. This independence has and will continue to allow the profession to adapt to changes in national policy and legislation and the MHNMI would argue that the discipline of psychiatric nursing has been capable of meeting such challenges in a positive manner an will continue to do so. 13 References An Bord Altranais (1986) A Training Programme for Psychiatric Nurses. Dublin, An Bord Altranais. An Bord Altranais 1991 Nurse education and training consultative document. Interim report of the review committee. An Bord Altranais, Dublin An Bord Altranais 1994 The future of nurse education and training in Ireland. An Bord Altranais, Dublin. Appleby, J, Brewins, L. (1992) Profile of a profession. Nursing Times, 88.24-29 Audit Commission Report (1994) Finding A Place: A Review Of Mental Health Services For Adults. London, HMSO. Bannon, H. and McDonald, B. (2003) Satisfaction with home-based treatment in mental health. Irish Nurse, 5(10), 24-25. Barker,P. (1989) Reflections on the Philosophy of Caring in Mental Health International Journal of Nursing Studies. Vol 26,2,131-141. Baier M 1989 Why research doesn’t yield treatment. Journal of Psychosocial Nursing and Mental Health Services. 26, 5, 29-33 Baume P 1992 Response to draft paper on mutual recognition of nurses – proposed implementation arrangement. Australia College of mental health nurses, Griffith University. 14 Burdekin B (1993) Human rights and mental illness, volume 1. Report of the national inquiry into the human rights of people with mental illness. Australia government publishing service, Canberra Belcher, P. Fish L (1995) Hildegard E. Peplau. In George J. Nursing Theories; The base for Professional Practice. London; Prentice Wall Bruest,M. (1989) Institutionalisation versus living in the community: psychiatric deinstitutionalisation and nursing in New South Wales. In: Issues in Australian Nursing 2 G. Gray and R. Platt (eds). Melbourne; Churchill Livingstone. Canavan, J. (2002) An analysis of how theories have effected the practice of nursing at present and how their changing nature may effect the practice of nursing in the future with particular reference to psychiatric nursing care Irish Nurse.5, (4), 26-28 Cowman, S. Farrelly, M, Gilleaney, P. (1997) The Role and Function of the Psychiatric Nurse in Clinical Practice. Dublin; Cahill Printers. Cowman, S. Farrelly, M, Gilleaney, P. (2001) An examination of to role and function of psychiatric nurses in clinical practice in Ireland Journal of Advanced Nursing, 34, (6), 745-753. Delacour S and Curry G 1991 Proceedings of the A.C.M.H.N. Inc Convention. From the ‘Deep regions’: Marginalisation of psychiatric mental health nursing in tertiary curricula. Sydney Australia, 151-171 Department of Health and Children (1998) The Commission on Nursing Report. Dublin, Government Publication Office. Gilheaney, P. and Farrelly, M. (1993) Psychiatric Nursing; Origins and development. An Bord Altranais News. 5(1), 4-8. Griffith O 1961 Contrasting patterns in nurse training. International Nursing Review 9 (5): 62-65 15 Hipps OS 1981 The integrated curriculum: the emperor is naked. American Journal of Nursing, May, 976-980 Local Government Staff Negotiations Board (1983) Community Psychiatric Nursing –Report of Review Group, Local Government Staff Negotiations Board. McCardle, J. (2003) The Exploration Of The Nature Of Community Psychiatric Nursing Practice And The Role Of Community Psychiatric Nurses (Cpns) In Ireland. University of Ulster / An Bord Altranais Unpublished D/Phil. Thesis. Nursing Education Forum 2001 Summary of final report. Newsletter issue 4 Nolan, P. (1993) A History of Mental Health Nursing. London: Chapman Hall. O’ Brien A 1995 Measuring graduated attitudes to educational preparation for practice in mental health nursing. Australia and New Zealand Journal of Mental Health Nursing 4 (3): 132-142 Savage, E. (1998) An Examination of the Changes in the Professional Role of The Nurse outside Ireland: A report prepared for the Commission on Nursing. Dublin; Stationery Office. Sheridan, A. (2000) Psychiatric Nursing. In J. Robins (eds) Nursing and Midwifery in Ireland in The Twentieth Century. Dublin; An Bord Altranais p. 163 –177. Treacy, C. (1987) Community psychiatric nursing in the community psychiatric catchment area 1 of the Eastern Health Board. University of Dublin. Unpublished M.Sc. dissertation. Wells, J.S. McElwee, C.N. (2000) The recruitment crisis in nursing: placing Irish psychiatric nursing in context—a review Journal of Advanced Nursing, 32 (1), 10-18. 16 Wells, J.S.G., Ryan, D., McElwee, C.N. (2000) I don’t want to be a psychiatric nurse: an exploration of factors inhibiting recruitment to psychiatric nursing in Ireland. Journal of Psychiatric and Mental Health Nursing. 7,79-87. 17