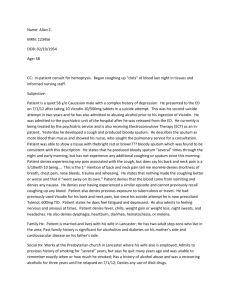
This 61 y/o male said he ocassionally coughed with some yellowish
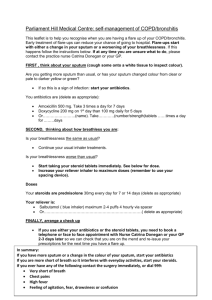
advertisement

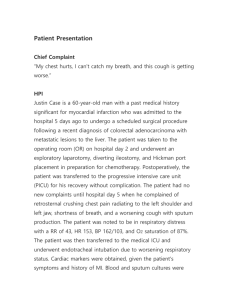
C.C: Cough with bloody sputum in the morning on 10/1 P.I:This 61 y/o male said he ocassionally coughed with some yellowish sputum before. But in the morning on 10/1, he suddenly waked up and felt chest tightness then coughed with bloody sputum about 5c.c. He drank some warm water and felt better. Then he came to our ER and OPD follewed up. But his symptom continued. So he came to our ward for futher evaluation. He said he ate some 葵瓜子 at night on 9/30 but didn't choke. His families all didn't have this symptom. He has chronic ischemic heart disease with OPD regular follow up but never feels orthopnea or paroxysmal noctumal dyspnea. He drank alcohol evernight for sociability when 30 decade but once a month now. He denies janudice and any other liver disease or HBV infection. He sometimes felt abdominal fullness and disturbance but denied nausea, vomiting and diarrhea. He also denis recently weight loss or melena. So we admit him to our ward for further evaluation and treatment. Dr Buttrey’s rewrite: CC: 61 y/o male c/o hemoptysis x1 for 1 day HPI: The patient says he has occasionally [Frequency? Q1wk, Q1mo?] had a cough productive of yellow sputum for [Duration?]. But on the morning of admission he woke up and felt chest tightness [Where exactly? Any SOB?] and coughed up about 5 cc of bloody sputum. [Was it mostly blood or mostly sputum with blood streaking?] He drank some water and felt better. [What felt better, the chest tightness?] He said he ate some 葵瓜子 the night before but didn't choke. Because of the hemoptysis, he came to the hospital and was evaluated in the OPD [When? What was done? What were the results? You say his symptoms continued. Over what period?] Therefore, he was admitted for further evaluation. He denies a FH of hemoptysis. He denies recent weight loss or melena. He sometimes has abdominal fullness but denies nausea, vomiting, or diarrhea. His old chart records a history of chronic IHD, but he denies orthopnea or PND. Missing data: Note that I didn’t include the information about liver disease or alcohol because I can’t see that it has any connection with the CC. See Comments below for further explanation. Data that should be included in the PI include the questions noted above plus others related to the differential diagnosis of hemoptysis. Is he a smoker? Has he had fever? Any known exposure to TB? Previous CXR’s? Previous diagnosis of lung disease from a doctor? If so, what? Any previous history of pneumonia? Wheezing? Any recent hoarseness? Any FH of lung cancer? Any symptoms of bleeding problems, e.g., bleeding gums, frequent bruising, difficulty stopping bleeding? Comments Content: The HPI should focus on the CC, so I’m not sure why the comments about heart disease and liver disease are included here. Tight mitral stenosis can result in hemoptysis, but I don’t think that’s what you thought he had. You might have included the comment about IHD because of the chest tightness. That’s important because we need to consider angina or an acute coronary syndrome as the cause of the chest tightness. However, you need much more information about that, either in the PI or in the PMH. If the latter, then you should write in the PI “see PMH.” Then we’ll know the information is available elsewhere. As it is, we don’t know what to think about the chest tightness. It’s good to know that he doesn’t have obvious CHF, but if we’re worried about acute coronary syndrome, there are other more important things to note. (Also note that the statement, “He has chronic ischemic heart disease with OPD regular follow up” doesn’t tell us very much. What symptoms does he have? How well controlled are they? What medication is he on? Does he take it as directed? This sort of data belongs in the PMH.) Liver disease with a resulting coagulation defect could also be manifested by hemoptysis, but again, I don’t think you were thinking of that. The information about alcohol is difficult to assess because it’s not clear how much he actually drank. “Social drinking” has different definitions for different people. As you have written it, it doesn’t help us assess the hemoptysis. If he had a history of getting drunk and may have had aspiration pneumonia in the past, we need to know that. He might then, for example, have bronchiectasis accounting for his hemoptysis. The PI should contain data that helps us sort through the differential diagnosis of hemoptysis in this patient. Common causes that immediately come to mind include: lung CA, TB, bronchiectasis, chronic bronchitis, laryngeal pathology, or a general bleeding diathesis. The fact that he only occasionally has yellowish sputum makes bronchiectasis and chronic bronchitis less likely, but the details need to be spelled out carefully before we can eliminate them from consideration. It’s clear that you were thinking about the possibility of aspiration, which is good! Overall, however, you need more specific details that relate to each of the diagnostic possibilities. The HPI in this sort of case is unlikely to give us the definitive diagnosis. However, it should point us in the right direction and at least help us have some idea of the probability of the various differential diagnoses. English: coughed with bloody sputum about 5c.c.: I would write “coughed up about 5 cc of bloody sputum. “Cough with sputum” is also called “productive cough.” These are terms describing a symptom and sign complex, but when describing the history, we should simply describe what happened. Then he came to our ER and OPD follewed up.: Then he came…for follow up. (And note that you need to say what happened at the ER and OPD. This is a content problem, not an English error.) His families all didn't have this symptom.: None of his family had this problem. Don’t use “all did not.” Instead, write “none did.” alcohol evernight for sociability: The commonly used term is “social drinking.” So this sentence could be written He drank socially every night when he was in his thirties but now only once/month. (Note again, from the content point of view, “social drinking” is too non-specific. We need to know exactly what and how much he drank in order to assess its possible impact on his health.) when 30 decade: Alternatives: in his thirties, or in his fourth decade. The former is more commonly used.