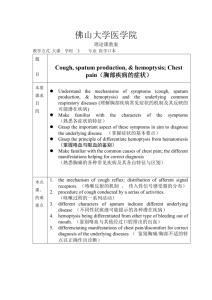
胸腔內科標準病歷範本
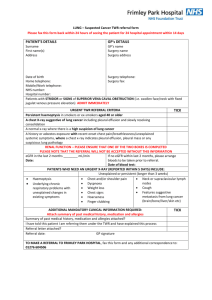
advertisement

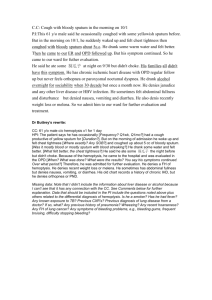
胸腔內科標準病歷範本 Case 1 1.主述:Non productive cough and intermittent fever for 3 weeks. 2. Present illness This 32 years old man of no systemic disease suffered nonproductive cough and intermittent fever for 3 weeks. The associated symptoms and onset were heralded by a flu-like illness with fever, malaise and fatigue. Dyspnea was light activity-aggravated but not sitting up-ameliorated. It sometimes associated with chest tightness, might last for more than half an hour but was not cold sweating-accompanied or resting-relieved. He lost about 6 kg within recent 3 weeks. His laboratory data disclosed leukoctyosis and elevated CRP level; physical examination, bilateral inspiratory rales; CXR, bilateral diffuse alveolar process over the lung fields. Under tentative diagnosis of community-acquired pneumonia, he was admitted to the chest ward for further appraisement and management. 3.住院主要臆斷:Community-acquired pneumonia, bilateral. 4.鑑別診斷:: Congestive heart failure with pulmonary edema Meatastatic lung cancer Pulmonary tuberculosis Chronic bronchitis with acute exacebation 5.住院診療計劃: Diagnosis plan: Sputum culture, Gram’s stain, AFS + TB culture,blood culture, Mycoplasma , follow up, pulmonary function test, cardiac echo, lung biopsy as needed. Therapeutic plan: Antibiotic treatment with Moxifloxacin 400mg qd ivd. O2 supply, symptomatic relief of supportive medication. Education plan: Mask wearing. 執行護理照護計畫. 住院診療計劃. Case 2 1.主述:Progressive hemoptysis for 10 days 2. Present illness This 78 years old woman of previous bronchiectasis for more than 15 years had pulmonary non-tuberculous mycobacterial (NTM) infection about 2 years. Anti-TB agents were prescribed for 2 months since Aug. to Oct. 2009. Besides, she was intubated in Aug. 2009 due to hemoptysis with acute respiratory failure. Intermittent dyspnic attacks and bloody phlegm were complaints for a long time. This time, the increased hemoptysis in recent 10 days was dyspnea-accompanied. Otherwise, there was no fever, chill, chest pain, or recent 6-month travel history. For the above hemoptysis, she was sent to our chest outpatient clinic. Serially, the taken CXR showed the more alveolar process surrounding the previous bronchiectatic area. For bronchiectasis with secondary infection and hemoptysis, she was to be admitted for further appraisement and management. 3.住院主要臆斷: Bronchiectasis with hemoptysis 4.鑑別診斷: Pneumonia 5.住院診療計劃: Diagnosis plan: Sputum microbial studies, including bacterial and mycobacterial cultures. Therapeutic plan: O2 therapy with nasal cannula to keep SpO2 greater than 90%, Antimicrotial therapy with pitamycin 3 gm IV q6h, Inhaled bronchodilators, including terbutaline (Bricanyl®) and ipratropium (Atrovent®) were given, Parenteral tranexamic acid (Transamin®) for hemoptysis, Anti-tussive and mucolytic agents for symptom control. Education plan: Surgical mask wearing. 執行護理照護計畫. 住院診療計劃. Case 3 1.主述:Right chest pain for 1 month 2. Present illness This 76 years old man suffered progressive right side chest pain about one month. The pain was worse with the deep inspiration and cough, besides mild dry cough noted. He denied recent dyspnea, fever or weight loss. For the chest pain, he was sent to our ER. Consecutively, chest radiograph revealed a huge mass lesion over the right upper lung field and moderate amount of right side pleural effusion; after thoracentesis for the pleural effusion performed at ER, the straw colored fluid was sent for analysis. The data denoted lymphocytosis (80%); chest CT, a mass lesion about 7.7*5.4*8.0 cm in RUL, and multiple nodules in RUL, RML, and RLL, in favor of lung-to-lung metastases. For lung cancer, RUL with lung-to-lung metastases and right malignant pleural effusion, he was admitted for further appraisement and treatment. 3.住院主要臆斷: Lung cancer, right upper lobe, with lung-to-lung metastases and malignant pleural effusion 4.鑑別診斷: 1).pulmonary tuberculosis with hematogenic spreading of lung, bilateral. and pleural effusion, right. 2) Pneumonia with pleural effusion, right. 5.住院診療計劃: Diagnosis plan: Pleural drainage with pig-tail catheter, Cytologic study of the pleural effusion specimen, Bronchoscopy for histological confirmation, Bone scan and brain contrasted CT scan for staging Therapeutic plan: Analgesics (e.g., Panadol) and antitussives (e.g., Medicon-A) for symptom control. Education plan: Explain risk and complication of pig-tail catheter insertion. 執行護理照護計畫. 住院診療計劃. Case 4 1.主述:Shortness of breath for one week 2. Present illness The 53 y/o female of antecedent asthma suffered shortness of breath for one week prior to admission, beside productive cough with yellowish, tenacious sputum and generalized soreness, and denied fever or chills. She was sent to our ER. Sequently, chest radiograph showed significant infiltrates over the right lower lung field; lab data, WBC: 10700/ul; CRP: 76.4 mg/L; glucose: 287 mg/dL. There were no chest pain, no hemoptysis, no recent 6-months-travel history, no weight loss, or no animal contact history. For bronchial asthma with acute exacerbation and secondary infection, she was admitted for further appraisement and treatment. 3.住院主要臆斷: Bronchial asthma with acute exacerbation and secondary infection 4.鑑別診斷: Pneumonia, right lower lobe. Congestive heart failure with cardiac asthma 5.住院診療計劃 Diagnosis plan: Sputum culture, Gram’s stain, AFS, TB culture, blood culture, lung function test. Therapeutic plan: Antibiotic treatment with Moxifloxacin 400mg qd ivd. O2 supply, symptomatic relief of supportive medication. Education plan: Surgical mask wearing. 執行護理照護計畫. 住院診療計劃. Case 5 1.主述:Fever off and on for 3 days 2. Present illness The 58 y/o woman suffered intermittent fever up to 38.8 °C for 3 days, beside productive cough with whitish sputum; her son, upper respiratory tract symptoms and fever at the same time. She visited LMD which certified common cold. Because her fever persisted, she was sent to our ER. Afterwards, chest radiograph revealed consolidative lesion in RUL; lab data depicted CRP 145.4 mg/L; WBC 8200 /ml; glucose 339 mg/dL. There was no chest pain, no hemoptysis, no dyspnea, no diarrhea, no abdominal pain, no travel history or no animal contact history. For RUL pneumonia and poor control DM, she was admitted for further appraisement and management. 3.住院主要臆斷 (1).Pneumonia, right upper lobe. (2).Hyperglycemia, suspect DM, por control. 4.鑑別診斷(for 1.) 1) Pulmonary tuberculosis 2) Obstructive pneumonitis, suspect endobrochial leison. 3) Lung abscess 5.住院診療計劃 Diagnosis plan: Sputum culture, Gram’s stain, AFS+ TB culture, cytology,HbA1c Chest CT scan , brochoscopy if necessory. Therapeutic plan: Antibiotic treatment with Augmentin ivd,mucolytic agent with Flumucil, symptomatic relief of supportive medication. Education plan: Surgical mask wearing. 執行護理照護計畫. 住院診療計劃. Case 6 1.主述:Hemoptysis for 10 days. 2. Present illness This 79 y/o male who denied any systemic disease suffered hemoptysis for 10 days. Cough with sputum in recent days was demonstrated, but no shortness of breath, no fever, no chills, no weight loss or no chest pain. So he came to our chest OPD. Successively, CXR projected perihilar infiltration with enlarged right hilum; the lab. data denoted: CBC/DC [10^3/uL]; R.B.C. [3.67 10^6/uL]; Hb [13.2 g/dL]; Hct [38.8 %]; platelet count [280 10^3/uL]; BUN [20 mg/dL]; glucose (random) [83 mg/dL]; creatinine [1.33 mg/dL]; Na [139.7 mEq/L]; K [4.08 mEq/L]; Cl [104.8 mEq/L]; S-GOT (AST) [21 IU/L]; S-GPT (ALT) [13 IU/L]. For the suspicious right lung tumor, he was recommended to be admitted for further appraisement and treatment. 3.住院主要臆斷 Lung tumor, right, suspect malignacy. 4..鑑別診斷: 1)Pulmonary tuberculosis 2)Bronchietasis 5.住院診療計劃 Diagnosis plan: Collect sputum for cytology, AFB+ ulture, Gram’s stain and bacteral culture, Bronchoscopy and /or Chest CT scan if necessory. Therapeutic plan: antitussives (e.g., Medicon-A) and Transamin for symptoms control. Education plan: Explain the possibility of lung malignacy or tuberculosis and the necessory of following study including of CT scan and bronchoscopy. 執行護理照護計畫. 住院診療計劃. Surgical mask wearing before negative sputum AFB report.