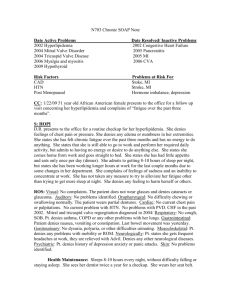
Name: Allan Z. MRN: 123456 DOB: 02/19/1954 Age: 58 CC: In
advertisement
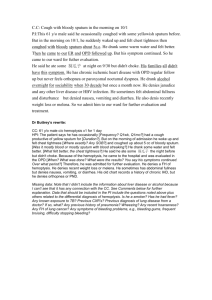
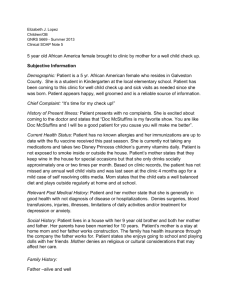
Name: Allan Z. MRN: 123456 DOB: 02/19/1954 Age: 58 CC: In-patient consult for hemoptysis. Began coughing up “clots” of blood last night in tissues and informed nursing staff. Subjective: Patient is a quiet 58 y/o Caucasian male with a complex history of depression. He presented to the ED on 7/1/12 after taking 10 Vicodin 10/500mg tablets in a suicide attempt. This was his second suicide attempt in two years and he has also admitted to abusing alcohol prior to his ingestion of Vicodin. He was admitted to the psychiatric unit of the hospital after he was released from the ED. He currently is being treated by the psychiatric service and is also receiving Electroconvulsive Therapy (ECT) as an inpatient. Yesterday he developed a cough and produced bloody sputum. He describes the sputum as more blood than mucus and showed his nurse, who sought the pulmonary service for a consultation. Patient was able to show a tissue with thebright red or brown??? bloody sputum which was found to be consistent with this description. He states that he produced bloody sputum “several” times through the night and early morning, but has not experience any additional coughing or sputum since this morning. Patient denies experiencing any pain associated with the cough, but does say his back and neck pain is a 5/10with 10 being…. This is the 1st mention of back and neck pain tell me moreHe denies shortness of breath, chest pain, nose bleeds, trauma and wheezing. He states that nothing made the coughing better or worse and that it “went away on its own.” Patient denies that the blood came from vomiting and denies any nausea. He denies ever having experienced a similar episode and cannot previously recall coughing up any blood. Patient also denies previous exposure to tuberculosis or travel. He had previously used Vicodin for his back and neck pain, but since his suicide attempt he is now prescribed Tylenol, 600mg TID. Patient states he does feel fatigued and depressed. He also admits to feeling nervous and anxious at times. Patient denies fever, chills, weight gain or weight loss, night sweats, and headaches. He also denies dysphagia, heartburn, diarrhea, hematochezia, or melena. Family Hx: Patient is married and lives with his wife in Lancaster; He has two adult step-sons who live in the area; Past family history is significant for alcoholism and diabetes on his mother’s side and cardiovascular disease on his father’s side. Social Hx: Works at the Presbyterian church in Lancaster where his wife also is employed; Admits to previous history of smoking for “several” years, but says he quit many years ago and was unable to remember exactly when or how much he smoked; Has a history of alcohol abuse and was a recovering alcoholic for three years until he relapsed on 7/1/12; Denies any use of illicit drugs. Allergies: Metformin, Oxycodone reaction??? Immunizations: Current Medications: Glipizide 10 mg PO daily; Lisinopril 20 mg PO daily; Ritalin 10 mg PO BID; Simvastatin 5 mg Q PM; Tylenol 600 mg TID; Fluoxetine 40 mg PO AM; Cymbalta 60 mg PO Q daily; Hydorchlorothiazide 25 mg PO Q daily PMH: Diabetes, Hypertension, Major Depressive Disorder, Sleep Apnea, MI, Prostate Cancerno mention of this above or in the assessment chronic back and neck pain or was it new??? PSH: Appendectomy (approximately 1969), Cervical arthrodesis (2001)is this the cause of his pain??? Objective: Vitals: Temperature: 98.8F (oral) P: 87 R: 16 BP: 154/93 SpO2: 95% Height: 71 inches Weight: 245lbs. BMI: 34.2 General Appearance: Flat affect, alert and oriented X3 Nose: No lesions, obstruction, redness or exudate found upon exam; no tenderness upon palpitation of frontal, maxillary, or ethmoid sinuses Throat: Erythematous gingiva noted, with multiple dental caries found; No gross blood, lesions, or ulcers found; tongue midline and symmetrical with no masses/ulcers noted; pharynx erythematous, no lesions/exudate; uvula symmetrical, no redness notedcontradicting Lymph nodes and thyroid?????? Chest: No scarring, asymmetry, striae, or ecchymosis of chest; No use of accessory muscles noted; Chest wall expansion is equal bilaterally without intercostal retractions; A:P ratio is 2:1; No tenderness or fremitus on palpation; Lung fields clear to percussion bilaterally; Upon auscultation dry breath sounds present and equal bilaterally in apices and bases, with no wheezing/rales/rhonchi/stridor appreciated Heart: Regular rate and rhythm; no murmurs or rubs; S1 and S2 appreciated Skin: No contusions, rashes, bleeding, or lesions noted; skin is warm and dry Peripheral Vascular: No edema of the upper or lower extremities noted; Radial and Dorsalis Pedis pulses palpated, present and equal bilaterally, +2/4 ABD????? Labs/Tests: CBC with differential: ordered Bronchoscopy: scheduled Chest X-ray: No infiltrates, atelectasis, or pneumothorax of the lungs. No cardiomegaly noted Assessment: 1) Major Depressive Disorder 2) Hemoptysis 3) Hypertension 4) Diabetes Mellitus 5) Sleep Apnea Differential Diagnosis: Infection of respiratory tract, Pneumonia, Neoplasm, Foreign body, Pulmonary embolism, Pulmonary hypertension, Tuberculosis, Idiopathic hemoptysis, Goodpasture’s syndrome, Wegener’s granulomatosis Plan: 1) Major Depressive Disorder: Hospital psychiatric service is currently working with Mr. Z in the inpatient setting where he is receiving counseling, adjustment of his antidepressant medications and is also receiving ECT treatments several times a week. Patient, family and psychiatry are currently investigating the option of an intensive outpatient program for Mr. Z upon his discharge. 2) Hemoptysis: Mr. Z is scheduled for a bronchoscopy to evaluate the bronchial tree tomorrow with Dr. Dolina. Patient initially was also scheduled to receive an ECT treatment early tomorrow morning, but because both procedures would require anesthesia, his ECT was rescheduled for next week. Patient expressed some disappointment that his ECT would be delayed, but upon further discussion agreed that the bronchoscopy should be performed as soon as possible. Written consent for the bronchoscopy was obtained and he was advised of the risks of the procedure including collapse of the lung, bleeding, damage to the bronchial tree and infection. He was also advised that he needed to be NPO after midnight. Patient is also scheduled for a CBC with differential to be collected tomorrow morning. 3) Hypertension: Continue patient on current medicine regimen and continue to monitor vitals. Vital signs are currently ordered for every 6 hours. 4) Diabetes Mellitus: Continue glipizide 10 mg PO daily and continue to monitor blood glucose levels. Patient is on a “consistent carb” diet in the hospital. 5) Sleep Apnea: Continue use of CPAP machine as directed. Machine is in patient’s room and he states he has been using it every night. Patient follows up annually with Dr. Jean in the pulmonology group for sleep apnea. In addition, Mr. Z is scheduled to follow up with his PCP following his discharge. Patient states that he does visit his PCP “at least” annually where he monitors his prostate cancer and obtains annual colonoscopies as well as “blood work.” Mr. Z denies any additional questions and agreed to comply with the pre-procedure protocol for the bronchoscopy. 25/30 Vanessa G Wittstruck, PA-S 7/12/12 11:22