5_HAP
advertisement

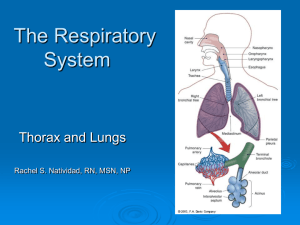
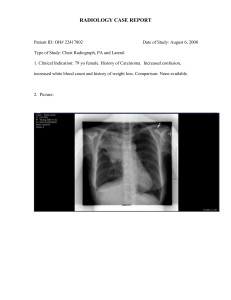
Patient Presentation Chief Complaint “My chest hurts, I can't catch my breath, and this cough is getting worse.” HPI Justin Case is a 60-year-old man with a past medical history significant for myocardial infarction who was admitted to the hospital 5 days ago to undergo a scheduled surgical procedure following a recent diagnosis of colorectal adenocarcinoma with metastatic lesions to the liver. The patient was taken to the operating room (OR) on hospital day 2 and underwent an exploratory laparotomy, diverting ileostomy, and Hickman port placement in preparation for chemotherapy. Postoperatively, the patient was transferred to the progressive intensive care unit (PICU) for his recovery without complication. The patient had no new complaints until hospital day 5 when he complained of retrosternal crushing chest pain radiating to the left shoulder and left jaw, shortness of breath, and a worsening cough with sputum production. The patient was noted to be in respiratory distress with a RR of 43, HR 153, BP 162/103, and O2 saturation of 87%. The patient was then transferred to the medical ICU and underwent endotracheal intubation due to worsening respiratory status. Cardiac markers were obtained, given the patient's symptoms and history of MI. Blood and sputum cultures were obtained after patient transfer. PMH Coronary artery disease, S/P MI 3 years ago for which he did not undergo any surgical intervention SH Lives with his wife Smokes one ppd × 40 years Denies alcohol or illicit drug use Meds Patient states that he did not take any medications at home. Hospital medications include (ICU medication list): Aspirin 325 mg po daily Enoxaparin 70 mg subcutaneously every 12 hours Esomeprazole 40 mg po daily Fentanyl 25 mcg/h IV continuous infusion Lorazepam 2 mg/h IV continuous infusion Metoprolol 25 mg po every 12 hours Morphine 1–2 mg IV every 1–2 hours as needed for chest pain Nicotine patch 21 mg per day applied daily All NKDA ROS Patient is experiencing significant chest pain, shortness of breath, and a cough with sputum production. He denies nausea, vomiting, or difficulty urinating. He complains of mild abdominal pain near his ostomy and incision sites. Physical Examination Gen WDWN Caucasian man, initially anxious, ill-appearing, and in moderate respiratory distress; now, S/P endotracheal intubation and in NAD VS BP 162/103, P 147, RR 42, T 38.5°C; Wt 70 kg, Ht 5′6″ Skin Warm; no rash; no skin breakdown HEENT PERRLA; moist mucous membranes Neck/Lymph Nodes Supple; no lymphadenopathy Lungs/Thorax Scattered rhonchi with expiratory wheezing; diffuse bilateral crackles; decreased breath sounds in bilateral bases; right IJ port-acath intact without erythema CV Tachycardic with regular rhythm; no MRG Abd Soft; mildly distended; hypoactive BS; large liver palpated in RUQ; ileostomy in RLQ is pink and functioning; surgical incision is C/D/I. Genit/Rect Deferred MS/Ext 1+ pitting edema; 2+ pulses bilaterally; good peripheral perfusion Neuro Prior to intubation, A & O × 3; CN II–XII intact; patient is now intubated and sedated. Labs Lab Parameter Admission Hospital Day 5 Na (mEq/L) 130 141 K (mEq/L) 4.1 5.1 Cl (mEq/L) 92 110 CO2 (mEq/L) 24 19 BUN (mg/dL) 22 34 SCr (mg/dL 1 1.1 Glu (mg/dL 113 148 Ca (mg/dL 9.4 9.2 WBC (mm− 3) 9.5 × 103 17 × 103 Neutros (%) 89 88 Bands (%) 0 5 Lymphs (%) 5 4 Monos (%) 6 3 Eos (%) 0 0 11.9 12.4 Hgb (g/dL) Hct (%) 35 37 Plts (mm− 3) 448 × 103 584 × 103 Cardiac Markers CK 871 IU/L, troponin-I 1.23 ng/mL ABG pH 7.39; PaCO2 30; PaO2 51 with 87% O2 saturation on room air (preintubation) pH 7.44; PaCO2 29; PaO2 89 with 100% O2 saturation on 40% inspired oxygen (postintubation) Chest X-Ray New bilateral opacities are noted in the left upper lobe and right middle lobe; likely infectious process. Some increased alveolar infiltrates in the perihilar location and involving the lower lobes. Chest CT Scan with IV Contrast No evidence of pulmonary embolism. The heart size is normal. There are small mediastinal and axillary lymph nodes; none are pathologically enlarged. There are small bilateral pleural effusions with adjacent atelectasis. There are pleural-based airspace opacities within the left upper lobe and right middle lobe; this is most consistent with an acute infectious process. EKG Sinus tachycardia, low voltage QRS, septal infarct (age undetermined); ST- and T-wave abnormality; consider inferior ischemia. Inverted T waves noted in the inferior leads. Sputum Gram Stain >25 WBC/hpf, <10 epithelial cells/hpf, 1+ (few) gram-positive cocci, 3+ (many) gram-negative rods Sputum Culture Pending Blood Cultures × Two Sets Pending Assessment Presumed bilobar HAP involving the LUL and RML Postoperative NSTEMI