Bronchiectasis
advertisement

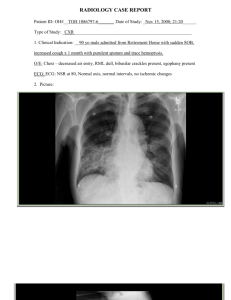
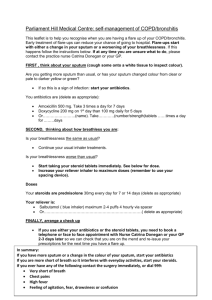
Pre referral checklists RESPIRATORY BRONCHIECTASIS General points: Chronically inflamed and damaged airways Typical features: o Chronic cough o sputum production o recurrent LRTIs CXR can be NORMAL diagnosis SECONDARY CARE by High resolution CT ( HRCT) causes- see appendix 1 Are there RED FLAGS Symptoms? = consider 2 week wait referral y/n Weight loss/anorexia (unintentional) Haemoptysis smokers Dyspnoea Chest Pain Hoarseness abnormal CXR fatigue clubbing supraclavicular lymphadenopathy Consider REFERRAL for DIAGNOSIS: Chronic (persistent) productive cough Daily expectoration of large volumes of purulent sputum Frequent lower respiratory tract infections Young age at presentation Absence of smoking Hx Sputum colonisation with Pseudomonas Aeruginosa or Staph aureus Recurrent haemoptysis (see above-may require 2ww referral) Persistent course crackles o/e For: Consideration for High Resolution CT for diagnosis Assessment of underlying cause Self-management advice Consideration for long term abs Elective intravenous antibiotics Chest physiotherapy y/n 1 Consider REFERRAL in established BRONCHIECTASIS y/n Recurrent exacerbations (> 3/yr) Worsening exacerbation frequency or respiratory symptoms Declining lung function New haemoptysis (see above- may require 2-week wait referral) New Pseudomonas, opportunistic mycobacterium or MRSA isolation in sputum Patients with associated rheumatoid arthritis, inflammatory bowel disease or immune deficiency Consideration for, or already on, long term antibiotics Advanced disease, consideration for transplantation Other diagnostic considerations: y/n Does the patients have COPD or Asthma? The conditions may coexist Consider coexistent bronchiectasis if: o Recovery from LRTIs is slow o Recurrent infections o Pseudomonas isolated from sputum o Worsening disease control despite optimal therapy If so, has their COPD or asthma management been optimised? PRIMARY CARE MANAGEMENT: patient education: smoking, when to seek help encourage adherence to chest physiotherapy pneumococcal vac and annual flu vac consider coexistent asthma or COPD and optimise treatment spirometry to assess for severity and deterioration Exacerbations: o sputum culture advised prior to commencing treatment (and encouraged at each review) to guide antibacterials for future chest infections – do not delay antibiotics whilst waiting for sputum result o antibiotics 14 days o use antibiotics based on previous positive sputum cultures or as directed in patient’s self-management plan o if NO previous sputum microbiology available treat empirically: o co-amoxiclav 625MG TDS or if penicillin allergic Doxycycline 200mg od https://www.brit-thoracic.org.uk/document-library/clinicalinformation/bronchiectasis/bts-guideline-for-non-cf-bronchiectasis/ Thanks to Dr John Steer and Dr Les Ashton, November 2015 2 APPENDIX 1 ATEIOLOGY INCIDENCE Idiopathic Up to 53% Post infection Up to 42% Immune defect 8% allergic bronchopulminary aspergillosis Aspiration / GORD 7% Hx asthma 4% Hx aspiration / reflux RA 3% Hx RA Cystic Fibrosis 3% Ciliary Dysfunction 1.5% Ulcerative Colitis <1% Age < 40, malabsorbtion, male infertility, diabetes Situs inversus, productive cough, deafness, infertility Diarrhoea . malabsorption, wt loss, joint pain Congenital <1% HX/ SIGNS Hx pneumonia, pertussis, measles, TB Ix Diagnosis of exclusion CXR or CT scan evidence of previous infection Decreased immunoglobulin levels or functional ab deficiency Eosinophilia Raised IgE Foreign body or mucus plugging on bronchoscopy Positive immune screen Positive sweat test Abnormal ciliary beat pattern Colonoscopic biopsies suggestive of IBD 3