Rapid Programme Review report for Mongolia
advertisement

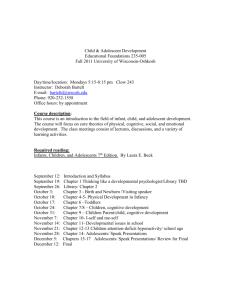
WPR/DHP/MCN(1)/2010.1 Report series number: RS/2010/GE/__(MOG) English only REPORT RAPID PROGRAMME REVIEW OF SELECTED NATIONAL PUBLIC HEALTH PROGRAMMES ADDRESSING ADOLESCENT HEALTH IN MONGOLIA Convened by: WORLD HEALTH ORGANIZATION REGIONAL OFFICE FOR THE WESTERN PACIFIC Ulaanbaatar, Mongolia 20–26 June 2010 Not for sale Printed and distributed by: World Health Organization Regional Office for the Western Pacific Manila, Philippines August 2010 NOTE The views expressed in this report are those of the participants in the Rapid Programme Review of Selected Public Health Programmes addressing Adolescent Health in Mongolia and do not necessarily reflect the policies of the World Health Organization. This report has been prepared by the World Health Organization Regional Office for the Western Pacific for the governments of Member States in the Region and for those who participated in the Rapid Programme Review of Adolescent Health in Mongolia, which was held in Mongolia from 20 to 26 June 2010. -2- TABLE OF CONTENTS ACRONYMS AND ABBREVIATIONS ................................................................... - 3 INTRODUCTION AND METHODS 4 BACKGROUND 4 Preparations to undertake the rapid review in Mongolia Methods of the review FINDINGS OF THE REVIEW 4 5 7 1. Mental Health 7 2. Alcohol Abuse ........................................................................................... - 8 3. Tobacco Use ............................................................................................. - 9 4. Nutrition 11 5. Sexual/Reproductive Health (SRH) and HIV/STIs ................................... - 12 6. Adolescent Friendly Health Services (AFHS) .......................................... - 14 General Conclusions of the Rapid Programme Review 15 . Limitations of the Review ............................................................................. - 15 Recommendations of the Rapid Programme Review ................................... - 15 Recommendations ............................................................................................... General Recommendations................................................................................. - 16 Specific Recommendations 17 Action Steps ................................................................................................. - 20 GROUP 1: PARENTS ........................................................................................ - 21 GROUP 2: TEACHERS...................................................................................... - 21 Group 3. SOCIAL WORKERS: 22 Group 4. NGOs/CIVIL SOCIETY BODIES 22 Group 5. INSPECTORATE AGENCIES: 23 Group 6. HEALTH WORKERS 23 Group 7. PEERS 24 REFERENCES ... - 25 - ANNEXE 27 -2- -3- ACRONYMS AND ABBREVIATIONS ADH Adolescent Health and Development Bag feldshers Village-level health care workers AFHS Adolescent Friendly Health Services GSHS Global School-based Student Health Survey GYTS Global Youth Tobacco Survey HE Health education HP Health promotion HSSMP Mongolian Health Sector Strategic Master Plan INGO International non-governmental organisation MARA Most at risk adolescents MCH Maternal and child health MoH Ministry of Health MoSWL Ministry of Social Welfare and Labour NCD Non-communicable disease NGO Non-governmental organisation RPR Rapid Programme Review SRH Sexual and reproductive health STIs Sexually transmitted infections UNICEF United Nations Children’s Fund UNFPA United Nations Fund for Population Activities WHO World Health Organization WHO CCS WHO Country Cooperation Strategy WPRO Western Pacific Regional Office (WHO) -3- -4- 1. 1.1 INTRODUCTION AND METHODS Background Mongolia is a young country. Half the population of Mongolia are under the age of 19 years, with about 20% in the adolescent age group (10-19 years). With a breakdown of traditional norms and nomadic way of life, increasing mobility, improved purchasing power for some, and in the context of uptake of some risk practices, it is important to consider ways to promote the health of young people. Tobacco and alcohol use are of increasing concern in Mongolia, as are sexual and reproductive health (SRH), STIs and the potential spread of HIV which is currently at low prevalence. Adolescents are explicitly recognised as an important population subset within many Mongolian health policy and strategy documents. Mongolia is seen as a country with achievements in some domains of adolescent health. It was among the first to set up models of Adolescent Friendly Health Services (AFHS) with support from WHO, United Nations Population Fund (UNFPA) and others, and about 18 such facilities operate. National standards were developed in 2001. Nonetheless, there is a lack of information regarding programme outputs and outcomes. Mongolia’s Ministry of Health requested WHO to provide technical support to carry out a programme review for adolescent health and development (ADH) in 2009. Due to an outbreak of H1N1 this was postponed until 21 to 25 June 2010. Preparations to undertake the rapid review in Mongolia A teleconference between the Ministry of Health, WHO Mongolia, WHO/WPRO and WHO/HQ was held in April 2010 to develop a shared understanding about the review. Leadership would remain with Ministry of Health, with support from WHO in conjunction with other partners and stakeholders. The scope and process of the review were agreed. SRH, HIV/STI and Mental Health were short-listed for focus and tobacco, alcohol and nutrition were candidates. A desk review would be undertaken and background papers prepared on each issue prior to the review. Dr Gochoo Soyolgerel from Ministry of Health led a working group of stakeholders established by Ministerial decree to plan the organisation of the review. This group held a retreat in April 2010, during which specific technical support for the review from WPRO was requested. Consequently, Dr Patanjali Dev Nayar, Technical Officer of the Maternal, Child Health and Nutrition, WHO/WPRO, visited Ulaanbaatar from 19 to 24 May to agree final focal areas and the process of the field review. The focus areas agreed included: Mental Health Alcohol Abuse Tobacco Use Nutrition Sexual and Reproductive Health (SRH) HIV/AIDS and STIs Adolescent Friendly Health Services (AFHS) -4- -5- 1.2 Objectives The specific objectives of the review were agreed as follows: (1) to assess progress made by selected national public health programmes in addressing adolescents; 1.3 (2) to identify challenges and opportunities to strengthen these programmes; and (3) to make recommendations for programmes and propose next steps for action. Participants The core review team comprised the following individuals: Dr Gochoo Soyolgerel (Ministry of Health), Dr Salik Govind (WHO Mongolia), Dr Tsogzolmaa Bayandorj (WHO Mongolia), Ms Tuul Dorjderem (National Consultant), Dr Martha Morrow (WHO consultant), Dr Patanjali D Nayar (WHO/WPRO), Dr Venkatraman Chandra-Mouli (WHO Geneva, team leader). The list of participants is included in Annex 1. 2. 2.1 PROCEEDINGS Methods of the review The review process was guided by an assessment tool for a Rapid Programme Review (RPR) (v 2) designed by WHO, which has been used elsewhere to support the collection, synthesis and interpretation of available documents and views of key informants. The RPR tool is organized to generate evidence relating to the following: Epidemiology (scope of the problem) and programmatic priorities Policies to guide the work of all sectors to be involved in implementing the strategies The response of the health sector The response of sectors other than health Leadership and management. 2.1.1 Document review A national consultant, Ms Tuul Dorjderem, utilised the RPR template and met widely with key informants prior to the field review to obtain relevant policies, strategies, plans, reports, academic publications and other documents. She then prepared extensive background reports according to the template for all areas, including NCDs, which were shared and commented on -5- -6- by members of the core review team. The background papers formed an essential data source throughout the review. 2.2.2 Field review period (19-26 June 2010) Team meetings were held on the weekend of 19-20 June to discuss process and areas of responsibility. The period of 21-25 June involved active engagement over the bulk of working days between the team and key programme directors/managers and other stakeholders, whose knowledge and views were essential to the collection and interpretation of information, and the development of conclusions and recommendations. 2.2.3 Key informant interviews During the field review, additional information, perspectives and clarifications were sought from directors and managers of programmes, local and international organizations working in areas relating to the scope of the review. An additional opportunity was afforded through a field visit to four health facilities in Ulaanbaatar. 2.2.4 Workshop Two full days of the review were spent in a countryside location (Terelj Bumban) about two hours from the capital to enable discussion, clarification and suggestions to be elicited from public health directors and managers, health and education providers, university-based experts and several adolescents (chosen by convenience). (See ANNEXE for a list of workshop participants). Some participants came from distant regions of the country, although most are based in the capital. The format was interactive and iterative, with opportunities for all participants to consider the strengths, weaknesses, gaps and opportunities for their programme to respond to ADH needs. 2.2.5 Presentations to stakeholders and refinement of findings On 24 June the core team presented initial findings to a group primarily composed of those who attended the workshop outside of Ulaanbaatar. This group was supplemented by several key government decision-makers. This presentation enabled stakeholders to correct and clarify emerging findings. 2.2.6 Age bands The potential for misunderstanding of terminology was addressed during presentations. It was noted that definitions from UN agencies and others overlap age bands, eg, adolescents (10 19 years), youth (15-24 years), and young people (10-24 years). The review has examined responses to all three groups. Where appropriate we have used the term ‘young people’ or ‘youth’; otherwise we have used the term ‘adolescent’. 2.2.7 Final Presentation to Ministry of Health and other stakeholders A presentation of revised findings and draft conclusions was made on 25 June to workshop participants, senior Ministry of Health officials and several representatives of other relevant agencies in Mongolia, including Save the Children and UNFPA. Once again, emerging findings and conclusions were discussed. -6- -7- All inputs were utilized by the core team during the afternoon of 25 June and (without the external consultant) on 26 June to identify recommendations and next steps for action. 2.2 Findings of the review In accordance with the objectives of the Rapid Programme Review, we have organized a summary of key findings under each area reviewed as follows: Scope of the problem in adolescents Policies to guide the national response to adolescents Implementation (strategic actions) – by the health sector and other sectors Programme management Conclusions It also should be noted that we have combined two areas, Sexual and Reproductive Health (SRH) and HIV/STIs, because of the high degree of overlap in determinants, policies and management. The final set of findings relates to Adolescent Friendly Health Services, which is distinct from other areas insofar as it is an intervention – and one with current application to SRH and HIV/STIs – rather than a health problem. 2.2.1 Mental health (1) Scope of the problem (a) Data on increase in mental disorders – not age disaggregated The Second National Mental Health Programme (2010–2019) [1] notes steep increases in mental disorders from 77.4 to 112.9 per 10 000 people in 2007. However, data have not been disaggregated by age, so prevalence among youth is not known. (b) Suicide and mental health promotion in youth a concern The Global School-based Student Health Survey Mongolia (GSHS) (2010) [2] (age 13-15) found 15.3% of boys and 22.6% of girls had considered suicide in the past 12 months. Bullying was also found, reported on at least one day in previous 30 days by 37% of boys and 20% of girls. In terms of protective factors, the GSHS found just 30% of boys and 31% of girls felt parents/guardians ‘understood their problems … most of the time or always’ in the past 30 days. Smaller studies have found school drop out was linked to bullying, many youth felt parents did not care about them, and teachers were considered authoritarian. Other studies found evidence of poor mental health in youth, including cases of acute intoxication, joblessness, poor relationship with parents and teachers, lack of coping skills, homelessness and violence ([3-5]). (2) Policy as relevant to adolescents: Second National Mental Health Programme 2010– 2019 Adolescents are separately identified in the policy as a population of interest, with components for appropriate capacity building for doctors and specialists, as well as teachers, health promoting schools, and collective support of adolescent health. It is explicitly multisectoral, calling for support on adolescent mental health from ministries including: Social Welfare and Labour; Education, Science and Culture; and governors, NGOs and National Authority for Children. It calls for the Human Rights Commission to evaluate implementation of laws to protect rights of the mentally ill. -7- -8- (3) Implementation (a) Health sector Efforts have been made to build capacity (e.g., postgraduate training and refresher training on mental health were conducted) and to prepare guidelines, but focus was weak on adolescents in the previous national programme. No specialised units for adolescent mental health exist [6]. The 2009 Mental Health Progress Review found there are just 0.9 mental health doctors per 10 000 population (but only 0.2 per 10 000 in rural and remote areas) [7]. (b) Other sectors According to the Second National Mental Health Programme, 20% of secondary schools undertook mental health prevention activities in 2009. However, key informants indicated that while these activities are part of the curriculum, they have not been addressed in a comprehensive manner. The 2009 Review of the programme [7] noted WHO had supported training of teachers and social workers that includes mental health, but there was a lack of materials and supplies. (4) Programme Management The programme director recognizes the importance of addressing adolescents, but notes the inadequacy of action and resources. (5) Conclusions Most focus is on in-patient services and doctors and there are insufficient funds for preventive and community based services for adolescents (64% of expenditure is spent on in-patient care. Additional surveillance on depression and common youth disorders is needed, disaggregated by sex/age/location to enable identification of groups with special needs. 2.2.2 Alcohol abuse (1) Scope of the problem in adolescents: harmful to adolescents through exposure and direct use. Alcohol is widely used in Mongolia by both sexes, which means that adolescents – along with other population groups – suffer some of the second-hand consequences of this environment. Many adolescents themselves use alcohol (including to excess), which means they suffer direct impacts of this behaviour. (a) Alcohol abuse has doubled since 1997 [8] Alcohol is now a leading cause of mortality and morbidity in Mongolia (including, eg, 84% of road accidents). Some of the negative effects on youth include family violence, child abuse/ neglect, divorce, school drop out and running away from home. Evidence suggests alcohol is a major explanatory factor for 82% of children who end up on the streets [9-10]. (b) Youth drinking widespread, especially (but not only) among boys, with insufficient knowledge on harms of alcohol. -8- -9- The GSHS (2010) [2] reported that, among students aged 13-15, 70% of boys and 65% of girls had tasted alcohol before age 14. A joint MoH and UN agency study found consumption two times higher in urban areas than in rural (cited in [10]). Research also found poor knowledge about alcohol’s dangers among youth [11]. Among youth aged 15-24, binge drinking (4+ drinks on one occasion) was practised at times by 24% of males and 9% of females [12]. Intoxication is known to be linked to violence, crime, injuries and risky sex. (2) Policy as relevant to adolescents: National Programme on Prevention and Control of Alcoholism 2003–2012 [10] The policy addresses both demand and supply side, covering all internationally recommended actions, including: restrictions on sales near schools and after midnight and sponsorship of youth events; raising legal age of drinking to 21; gradual increase in taxation; and education and life skills programmes to discourage risky drinking. (3) Implementation (a) Health sector and other sectors Overall, there has been very little progress in implementing alcohol control policies, including in relation to adolescents. A mid-term evaluation of the current programme [13] found implementation almost at a standstill, with a progress rate of 0.3%. Marginally better progress occurred in terms of general health education and promotion for school children, but actual time focusing on alcohol (and other health topics) was very small (around an hour per year for just 39% of students). Training of teachers and health professionals has been undertaken at 20% of the desired level. Challenges for law enforcement include poor enforcement of bans on locations of selling (near schools), advertising and sponsorship, low taxes and price of alcohol (relatively affordable for youth), and lack of resources [10]. (4) Programme Management Managers recognize the importance for adolescents, and express concern at lack of funding support and progress. Funding for programme primarily is generated by the 2% tax on tobacco, which is a modest sum. (5) Conclusions Adequate strategic information and supportive policies Implementation, enforcement weak Inadequate focus on cessation and prevention for adolescents Inadequate resources under current funding model 2.2.3 Tobacco use (1) Scope of the problem in adolescents: Harmful to adolescents through exposure and direct use. Like alcohol abuse, smoking affects Mongolian adolescents both indirectly, through exposure at home and in public places due to high prevalence (among m en), and directly, through their own consumption. The gendered nature of tobacco consumption is particularly notable. (a) Adult male smoking rates are 43%, over 10 times those of females (4%) [12]. -9- - 10 - The impact of second-hand smoking is harmful for respiratory health of all people, including children and adolescents. It also normalises (especially) male smoking through role modelling by fathers, male relatives and other men in the community. Tobacco is very affordable; the cheapest popular brand is priced at about USD 0.39, and attracts very low excise [14]. (b) Smoking prevalent among Mongolian youth, especially males The STEPS 2006 survey [12] found that 23.3% of males aged 15-24 were current smokers, versus 2.1% of females. Average age of smoking initiation among males was 19 and females 28 years. The most recent Global Youth Tobacco Survey (GYTS) [15] among Mongolian students aged 13-15 found higher, and more equal, rates between the sexes (males 35%; females 13%). Students in the survey who smoked were more likely to be from smoking households. Most (88%) recognised that smoking is harmful. An article reporting on the 2003 GYTS noted higher rates of smoking among students with spending money, and lower odds among those who saw smoking as harmful [16]. The Health Professional Student Survey found current smoking rates of 59% for males and 25% for females in Mongolia, which is particularly concerning given their field of study and potential as role models [15]. (2) Policies as relevant to adolescents: Law on Tobacco Control 2005 [17] This policy, like the programme aimed at preventing alcoholism, addresses both demand and supply side considerations, and generally adopts the features of the WHO Framework Convention on Tobacco Control (to which Mongolia is a signatory). The Law restricts sales, sponsorship of youth events, raises the legal age of purchasing tobacco to 18, introduces gradual increases in taxation, and nominates education and life skills to discourage smoking. In 2007, Mongolia began to divert 2% of tobacco taxes to set up the Health Promotion Foundation, and to use these proceeds for anti-tobacco and anti-alcohol activities. (3) Implementation (a) Health sector and other sectors Much like the situation for alcoholism prevention, action on tobacco is inadequate for all populations, and very little directly targets young people. Bans and restrictions are poorly enforced, with the tobacco industry able to find ways to circumvent laws on promotion, and prices remain relatively affordable for youth. Retailers cannot demand age identification, and children can buy cigarettes individually through unlicensed vendors [18]. Tobacco is part of the general health education in the school curriculum and many teachers have been trained, but a MoH survey found 39% of students were taught just one hour in previous year for all health topics [15]. The importance of gender norms for smoking uptake does not appear to have been incorporated into awareness activities. (4) Programme Management Managers recognise importance for adolescents, and express strong concern at continued uptake of tobacco. (5) Conclusions Disparities in rates between major surveys indicate need for continued monitoring by age, sex and location. Supportive policies, although higher prices would discourage adolescent uptake, and the harmfulness of male gender norms is not noted. Implementation, enforcement weak. - 10 - - 11 - Inadequate focus on cessation and prevention for adolescents. Inadequate resources, with small funding base of 2% tobacco tax. 2.2.4 Nutrition (1) Scope of the problem in adolescents In Mongolia, nutritional problems are linked to its terrain and climate, food availability, cultural norms and costs of food, as well as the increase in sedentary lifestyles for a formerly very physically active population. (1) Some evidence of over- and under-nutrition in adolescents, with regional disparities. The 2010 GSHS found 3.1% of urban 13-15 year olds were underweight (vs 2.3% in rural areas). It also found higher rates of overweight/obesity in urban areas (7.9%) as compared to rural (6.4%). This survey also found around 35% of students drank soft drinks at least once a day in urban areas, vs 25.5% in rural areas [2]. The earlier 2002 WHO report on SRH of Adolescents and Youth [19] in Mongolia noted that 16% of adolescents were delayed physically, 47% were below average weight and 49% below average height. (a) Low intake of fruit, evidence of micronutrient deficiency The 2006 STEPS survey [12] found 32% of youth ate no fruit daily. Studies in 1999 in children and adolescents found 20% had signs of goitre (iodine deficiency) and 24% were anaemic [5]. (b) Traditional beliefs The 2007 UN Country Assessment [20] noted the existence of some harmful traditional beliefs about the need for meat and fats to counter the effects of prolonged severe cold weather in Mongolia. Normative eating patterns affect all age groups, including adolescents. (2) Policy as relevant to adolescents: National Food Security Programme 2009-2016 [21] This policy specifies the need for safe, nutritious food for school children. It calls for the development of a nutrition training curriculum, nutrition standards to meet specific needs for age and sex, and training of (teacher) trainers and training of volunteers. (3) Implementation (a) Health sector A Dietary Intake Survey was conducted in 2009 (results are pending). Key informants said that health service providers are generally unable to offer nutritional advice, although some of the doctors working in adolescent friendly health services make occasional school visits for this purpose, and have developed nutritional guidelines. (b) Other sectors Weak coverage of nutrition in school curriculum, with anecdotal evidence that policies on healthy eating in canteens are not enforced. - 11 - - 12 - (4) Programme management The director expressed strong interest and concern in relation to adolescent nutrition, but noted minimal action or coordination. It was suggested that the national focus on Millennium Development Goals may have resulted in relatively greater emphasis on maternal and child health, and less on adolescent well-being. (5) Conclusions Policy does address adolescents as a specific group. Need data on nutritional status, including micronutrients. Widespread consumption of ‘empty calories’ (soft drinks); Implementation of policy is weak or non-existent (in many areas); Resources are inadequate for the programme activities. 2.2.5 Sexual/Reproductive health (SRH) and HIV/STIs Although we are reporting on SRH and HIV/STIs in tandem, we have extracted the specific concerns of relevance for each issue to young people in Mongolia below. In the case of SRH, our particular focus is on pregnancy, abortion and RH knowledge in the teenage years, whereas for HIV/STIs our emphasis includes both adolescents and youth in their early 20s, because the latter age band often sees a sudden spike in STI and HIV infections and/or risk behaviours. Obviously, the risk practices for pregnancy are also risks for STI and HIV. (1) Scope of the problem in adolescents and youth (a) Adolescent pregnancy: Marginal increase from 2003–2008 According to the 2008 Reproductive Health Survey [22], the percentage of women aged 15-19 who had children or were pregnant has increased marginally from the 2003 RH Survey (from 7.4% to 8.2%). These figures both represent small declines from the rate of 9.0% in 1998. No childbearing or pregnancy was found among girls aged 15 in the 2008 survey. Importantly, however, there was a large increase in Ulaanbaatar from 4.5% in 2003 to 16.7% in 2008. The 2003 RH Survey [23] found girls aged 15-19 were the cohort most likely to deliver at home, with 57% having complications. Adolescent childbearing is also of concern because it usually interferes with educational attainment in young mothers, thus reducing career choices. (b) Contraceptive knowledge is high Over 90% of adolescents could name at least one modern method of contraception [22], with pills most often mentioned (83%), followed by IUD and Injections (each ~ 71%), female condom (70%) and male condom (64%). (c) Sexual debut A UNFPA situation analysis in 2005 [24] found mean age at first sexual intercourse was 16.8 for males and 18.9 for females, with 32.5% of respondents aged 15-19 having had sex. Forty-one percent overall reported sexual experience with a casual partner, with rates much higher in males (55%). Rural youth aged 11-16 were twice as likely to have had intercourse than urban counterparts. (d) Condom use - 12 - - 13 - The UNFPA report [24] found that among those having sex in the previous week, just 59.9% used condoms. Rates were as low as 6.7% at first intercourse among girls, and 20% at most recent intercourse. Condoms were used in these circumstances much less in rural than in urban areas. Embarrassment at buying condoms (and discussion of sexuality) were found in a qualitative study and a survey [25-26]. (e) Abortion in adolescence The 2009 Health Indicators [27] report that 6.2% of total abortions occurred in women below 20 years of age. (f) STIs: evidence of high prevalence among youth Documenting STI prevalence is complicated because infections may not be diagnosed and treatment is sought from both public and private providers. However, the Antenatal Clinics Epidemiology Survey 2001-2002, conducted by MOH (and partners), found high STI prevalence in general among pregnant women, with relatively higher rates in the 15-24 age group for: chlamydiasis (21-27%), trichomoniasis (8-13%) and gonorrhoea (7-8%) [24]. The UNICEF Midterm Report (2005) [28] also noted STIs comprise 36-42% of all communicable diseases. AIDS National Centre statistics suggest 39% of sex workers began aged 14-16, and this sub-group had low knowledge about STIs. Uneven knowledge exists on STIs, with especially poor understanding among youth with disabilities aged 15-24 [24, 29]. (g) HIV: low prevalence but risk factors exist The National Strategic Plan on HIV/AIDS and STIs (2009-2015) [30] reports low prevalence of HIV in Mongolia, with fewer than 80 cases identified nationally. It is likely that more infections exist. Of concern for youth is the potential for HIV to spread rapidly in Mongolia, given levels of unprotected sex and multiple partners [31], use of alcohol and STIs, as noted above. While HIV knowledge is good, it is not fully comprehensive in many young people [22]. (2) Policies as relevant to adolescents There are two main policies that address SRH and HIV/STIs: (3) Third National Reproductive Health Programme of Mongolia (2007-2011) [32] identifies adolescent fertility National Strategic Plan on HIV/AIDS and STIs 2009-2015 [30] cites adolescents as priority group. Implementation (a) Health sector Adolescent friendly clinics, with support from UNFPA and WHO (and others) (in most densely populated centres, ie aimags and Ulaanbaatar), and STI consultation centres have been initiated and guidelines developed in accordance with Objective 2 of the Third National RH Programme [32]. Programmes addressing the population as a whole also reach adolescents (e.g. IEC, 100% condom use programme). (b) Other sectors - 13 - - 14 - Educational materials on HIV/STI have been developed and some teachers trained. Materials for non-formal education on HIV/STI have also been developed, but it is not clear if these have been used. A small number of peer education programmes have been implemented, along with some awareness-raising for school doctors in large schools (>600 students). Some RH education has been conducted for police and armed forces, and an unknown number of journalists were oriented to communicate appropriate messages. (4) Programme management Compared to some programmes that involve adolescents and young people, resources are relatively more available. However RH programmes are less well funded compared to the HIV programme. (5) Conclusions Policy environment for both SRH and HIV/STIs is very supportive, and reasonably good data are available. Comprehensive data on STIs and abortion in youth are lacking. Effective but small scale implementation of activities (concentrated in more urbanized settings), with little evaluation to date. Limited activities by the education sector, including in life stills training. Various NGOs and agencies give services, but limited coordination reduces efficient use of resources. 2.2.6 Adolescent Friendly Health Services (AFHS) Mongolia has substantial experience and success in establishing AFHS. These mainly focus on SRH, although some incorporate interest in nutrition and there is potential to focus on other health areas. Numbers. UNFPA has supported the establishment of ‘Future Threshold Adolescent Health Centres’ (six located in three of the nine districts in the capital city, 12 located in 11 aimags). There are some others set up with support from WHO, GTZ and IPPF. Location. Capital city: District health centre/'Khoroo' health centre. Elsewhere in the country: Outpatient unit of the Department of Health. Activities carried out. SRH service provision; some outreach education; some peer education; and some training of health workers. Resources. Staff are paid for by the national/local government, as are infrastructure, amenities and basic equipment. Some medicines and supplies and educational materials are paid for by donors. Overall impression Quality: Many strengths and some weaknesses, but structured assessment needed. Coverage: Likely to be limited to the catchment area; assessment needed. Sustainability: Some elements could be sustained even if external funding ends. - 14 - - 15 - 3. 3.1 CONCLUSIONS AND RECOMMENDATIONS General conclusions of the Rapid Programme Review Drawing on all sources of information, including feedback from stakeholders, we offer the following overarching conclusions: (1) Our knowledge of the epidemiologic situation in adolescents is fairly good overall. However there are some gaps which need to be filled. (2) Adolescents have been identified in all the policy and strategy documents as a population segment to be addressed, and evidence-based actions have been proposed. Programme staff appear committed to addressing adolescents. (3) On HIV/AIDS and Reproductive Health, many – but not all – proposed actions have been implemented. The interest and support of external agencies has contributed to this. Useful lessons have been learned on youth friendly health services, though the reach of these initiatives has been limited. On other health issues, relatively little implementation has occurred. (4) Lack of adequate resources and inadequate collaboration within the health sector as well as with other sectors were identified by many key informants as a major hindering factor. Limitations of the review It is important to emphasize the limitations of our identified findings and conclusions. No piece of data collection can ever claim to be definitive. The first limitation relates to the limited timeframe for the review, although this was supplemented to a large extent by background documentary review and synthesis, together with intensive meetings in the field with key informants. The second relates to the scope of the review; while we spoke to several adolescents, we may have gained different or additional insight from discussions with adolescents from a diverse range of backgrounds. The third relates to the fact that those ultimately responsible for this report have only limited knowledge of Mongolia, and do not speak Mongolian. Again, this was addressed by using local informants for data gathering, discussion and analysis. Nonetheless, we offer our findings and conclusions with a degree of caution. 3.2 Recommendations of the Rapid Programme Review General Considerations The review team make the following observations which underpin their identification of recommendations: There is a need to balance efforts to prevent current mortality and morbidity, and to prevent the risk behaviours which will lead to mortality and morbidity in the future, particularly in relation to non-communicable diseases, which have a long lead time. - 15 - - 16 - There is a need for effective actions both within the health sector and outside the health sector. In health service provision, there is the need to find the right balance between: - Promotive and preventive health and curative and rehabilitative health; - Primary health care and tertiary health care; - Increasing and improving supply and creating demand. Adolescent health is influenced by both risk and protective factors. It is also a field of health in which it is singularly important for adults to learn ways of effective communication with young people. Therefore, well-being in adolescence can be achieved by reducing risk through legislation and protective policies and approaches, and providing what is needed to help young people make good choices (i.e. information, skills, supportive peers/family/teachers etc). It is thus apparent that effective responses to adolescent health needs in Mongolia, as elsewhere, are often similar in nature and approach. For this reason, we have clustered these as general recommendations in terms of actions and approaches that will cut across most or all of the areas reviewed. Specific recommendations for programme areas follow below, followed by overarching action steps. 3.2.1 General recommendations (1) Fill the gaps in adolescent epidemiology, identified in this review. (2) Step up the implementation of the actions proposed in the strategies in all areas reviewed. In doing this make every effort to strengthen synergy and use available assets effectively and efficiently (e.g. use a training opportunity for one health area to build capacity in others as well). (3) Document, evaluate and disseminate the experiences gained in youth friendly health service provision in the country. (4) Integrate and scale up youth friendly initiatives within the existing primary health care system (including soum health facilities, family group practices and bag feldshers). (5) Strengthen coordination and collaboration within the Ministry of Health, and with other sectors to ensure that a truly multisectoral response is in place. This may be achieved by establishing mechanisms such as a task force and a designated official/unit responsible for adolescent health. Note; Ways and means of strengthening collaboration Lack of collaboration was identified as a problem by all the programmes we reviewed. When we recommended stronger collaboration we were asked to provide concrete suggestions for making this happen. Here is a list of actions that the Ministry of Health could consider taking: 1. The Ministry of Health should clearly state that all the relevant programmes should collaborate (i.e. making a clear policy statement that it wants to see this happen.) 2. The Ministry of Health should provide incentives for collaboration. These could include both non-financial incentives (such as public recognition of collaborative work) and financial incentives (such as setting aside some funds for collaborative activities). 3. The Ministry of Health should bring representatives of different programmes (both at headquarters and from the field) together for an exercise that would include: an assessment of strengths, weaknesses, opportunities and threats (SWOT); visioning; road-mapping. This will help them to identify what they need to do, and where they could work together (i.e. in training teachers to communicate to adolescents about a variety of health issues) on the one hand, and where they need to work together separately (i.e. enforcement of a - 16 - - 17 - ban on tobacco advertising is relevant to the tobacco programme but not to the HIV programme). 4. As work plans and budgets are developed, the Ministry of Health should set up mechanisms that facilitate collaboration: peer review of the work plans of the different programmes; the development of Gantt charts with the roles and responsibilities of different programmes clearly noted. 5. Finally, the Ministry of Health should set up mechanisms for periodical information-sharing (e.g. quarterly information-sharing meetings). 3.2.2 Specific recommendations The specific recommendations presented below for each programme area have been derived from the conclusions of our review and conceptualized with reference to the policy and strategy documents of each programme, and to the following key overarching strategies : Mongolian Health Sector Strategic Master plan (HSSMP) (2006–2015) [33] WHO Country Cooperation Strategy (WHO CCS) (2010–2015) UNFPA 4th Country Programme (2007–2011) The specific section of these strategies is indicated at the outset of each set of recommendations. Specific recommendations have been grouped under the information and actions that are known to be crucial to ensure adolescent well-being: Strategic information (data or evidence that should be collected, analyzed and used for advocacy and to inform policies and programmes) Supportive policies (based on evidence, that can facilitate and guide action in relation to adolescent needs) Services and commodities (health services and commodities adolescents need to achieve clearly defined health outcomes) Strengthen other sectors (to support other sectors/civil society organizations to maximize their contribution to adolescent health and development). Note: Because of the overlap in recommendations for alcohol and tobacco use, these are presented together. The same approach has been used for SRH and HIV/STIs. 3.2.2.1 Mental health HSSMP (2006–2015) Essential package of services: mental health 5.3, adolescent health 2.4 WHO CCS (2010-2015) Strategic Priority 2, main focus 2.4, strategic approach 2.4.3. (1) Strategic information: Identify appropriate indicators on adolescent mental health, and ensure that age and sex disaggregated data is gathered, analysed and used. (2) Supportive policies: No actions are needed on this. - 17 - - 18 - (3) Services and commodities: Build the capacity of primary level health workers to diagnose and manage mental health problems at the primary level, and to refer patients who need specialized care to the next level. (4) Strengthen other sectors Build the capacities of teachers to build the psychosocial skills in their students, and to identify and refer those students who have mental health problems that might need medical attention. Build the capacities of parents to build the psychosocial skills of their sons and daughters and to refer them for medical attention if they might need it. Create awareness in communities about the need to promote mental health and respond to mental health problems when they occur with empathy and understanding. 3.2.2.2 o o Alcohol abuse and tobacco use HSSMP (2006-15) Essential Package of services: adolescent health - 2.4, non communicable diseases - 4.2; WHO CCS (2010-2015): Strategic priority - 2, main focus - 2.3, strategic approach - 2.3.1. (1) Strategic information: No actions needed. (2) Supportive policies: No actions needed. (3) Services and commodities: Build the capacities of health workers to provide tobacco and alcohol cessation services. (4) Strengthen other sectors 3.2.2.3 o o Build the capacities of teachers to create awareness among their students about the dangers of tobacco and alcohol use, and the negative consequences of male gender norms. Enforce laws to prohibit the advertising of tobacco and alcohol products and the sponsorship of sports and entertainment events; the sale of tobacco and alcohol to minors; and their sale near educational institutions. Increase taxes on tobacco and alcohol. Nutrition HSSMP (2006-15) Essential package of services: adolescent health - 2.4, integrated prevention and control of risk factors through enabling environment - 2.3; WHO CCS (2010-2015) Strategic priority - 2, main focus - 2.3, strategic approach - 2.3.1. (1) Strategic information: Strengthen epidemiology of nutritional status among adolescents. (2) Supportive policies: No actions needed. (3) Services and commodities: Build the capacities of primary level health workers to provide nutritional advice and counselling, and to diagnose and manage nutritional problems in adolescents. - 18 - - 19 - (4) Strengthen other sectors Build the capacities of teachers to carry out effective education programmes on healthy eating and regular exercise in schools. Educate parents and engage them to promote healthy eating and regular exercise at home. Create awareness in the community about the importance of healthy eating and regular exercise. Enforce laws and policies on the marketing and sale of food products, including in canteens. 3.2.2.4 Sexual and reproductive health and HIV/STIs Sexual and Reproductive Health o o o HSSMP (2006-15) Essential Package of services: reproductive health 1.1, 1.4, 1.5, 3.2 adolescent health - 2.4; WHO CCS (2010-2015): Strategic priority - 3, main focus - 3.2, strategic approach - 3.2.2. UNFPA 4th Country Programme (2007-2011): Output 2.1. HIV/STIs o o HSSMP (2006-15) Essential Package of services: STI/HIV/AIDS 3.2 adolescent health - 2.4; WHO CCS (2010-2015): Strategic priority - 3, main focus - 3.4, strategic approach - 3.4.2. (1) Strategic information: Strengthen epidemiology of STIs in young people. (2) Supportive policies: No actions needed. (3) Services and commodities Draw out the lessons learned from the adolescent friendly health services in the country. Scale up "friendly" health service provision to adolescents using the existing health care delivery system. (4) Strengthening other sectors Build the capacities of teachers to carry out effective reproductive health and life skills education programmes. 3.3 Articulating a vision for adolescents in Mongolia Our vision is that all adolescents should grow up in safe and supportive environments at home, in their schools and in their neighbourhoods. Firstly, we want them to grow up in homes which are safe and supportive. By safe we mean an environment with the food they need to grow and develop in good health, where they are not at risk of injuries, and where they are not exposed to tobacco, alcohol and violence. By supportive, we mean an environment in which they feel valued and where they learn how to stay healthy and to cope with the stresses and strains of everyday life. By supportive we also mean an environment where they can ask for and obtain help when in need. Secondly, we want them to learn in schools which are safe and supportive. By safe we mean an environment free of tobacco, unhealthy foods and violence. By supportive we mean - 19 - - 20 - an environment in which they feel supported, and learn how to stay healthy and to cope with the stresses and strains of everyday living. By supportive we also mean an environment where they can ask for and obtain help when in need. Thirdly, we want them to grow up in safe and supportive neighbourhoods. By safe we mean an environment where publicity of tobacco is banned, and publicity on alcohol and unhealthy foods is regulated, where access to tobacco, alcohol and unhealthy foods is restricted, and where there is no violence. By supportive, we mean an environment where caring and healthy norms prevail, and where they can get the health care or social services they need. For this vision to be achieved, in each community there needs to be caring, competent and diligent working together to meet the needs and fulfil the rights of adolescents: • parents • teachers • social workers • inspectors and law enforcement workers • health workers All the programmes that we reviewed - HIV, SRH, mental health, nutrition, tobacco and alcohol should work together to contribute to this. What this means is that strong collaboration in needed within the health sector. In addition, strong collaboration is needed between the health and other sectors such as education, social welfare and criminal justice. 3.3.1 Action steps After presentation of findings to stakeholders, the review team and partners discussed a range of potential actions that could be undertaken by various agencies or sectors to advance the recommendations listed above. We offer these here for consideration and discussion. The achievement of adolescent well-being depends on support from various actors: Parents Teachers Social workers NGO personnel Inspectors/Law enforcement officers Health workers Peers We have therefore conceptualized next steps in terms of mechanisms to enable these actors to play positive roles. We have also borne in mind the practical constraints of Mongolia, particularly in relation to low population density outside of Ulaanbaatar, long period of very cold weather, distances between areas of settlement, the availability of doctors and social workers in larger schools, and other current health activities and approaches that may permit efficiencies of scale. Potential next steps for each type of actor are described in relation to the following categories: Potential role of group Current activities related to this group Potential actions for consideration - 20 - - 21 - 3.3.1.1 Group 1: PARENTS Potential role of this group Parents may be the first port of call for adolescents in terms of getting information, understanding and support. Parents are able to play a crucial positive role in adolescent wellbeing, and are typically interested in doing so, but may lack the skills to support young people within an environment of social change. o o o Current activities related to this group Very little is being done There are no materials targeting parents Parents tend to be called in by school teachers in case the adolescent has a problem Potential actions for consideration o Schools could convene regular meetings with parents at the aimag, district and soum level. These meetings could be utilized for discussions and skills building of parents on issues of importance (to be selected in consultation with the school authorities and the parents). o NGOs, including INGOs (e.g. World Vision) could train their personnel to address parents in their work (e.g. in Mothers’ Groups). o Religious organizations (e.g. churches) could use their networks to address various aspects of adolescent health and development o To reach scattered populations, festivals and other events in rural areas, at which families remain for up to several days, could be utilized to inform parents and build their capacities. o Health facilities could inform parents about the importance, scope and availability of AFHS. This would also help increase demand for these services. 3.3.1.2 Group 2: TEACHERS Potential role of group Because of high school retention rates and the number of hours spent with young people, teachers have enormous potential to build the knowledge and understanding and skills of adolescents and to influence their behaviours. They also play a crucial role in ensuring that schools provide a safe and supportive environment. Current activities related to this group: Some capacity building efforts on adolescent health are being carried out. However the initiatives have not been scaled up (? lack of resources, other reasons) o Appropriate materials have been developed. Again the relevance and range of material need to be reviewed. Overall our review found that teachers lack the requisite knowledge and skills to address the needs of the adolescents adequately. Potential actions for consideration o School authorities and teachers could be sensitized and oriented to the opportunities and risks of adolescence, and the crucial role that they could play in ensuring their health and development. o School health promotion could be institutionalized - i.e. it should be part of the curriculum and the responsibilities of teachers and school principals, it should also be included in the students' examinations. o Criteria could be developed for involving teaching in school health promotion. - 21 - - 22 - o The capacities of teachers to address the critical risks faced by adolescents could be built through pre-service and in-service training (using both traditional and distance learning approaches), supportive supervision and follow up. Certified teachers could receive further training and join refresher courses periodically. o For this to be done, materials for sensitizing and orienting school authorities and teachers, and for the latter to use to inform and build skills of their students could be developed. o Teachers could be encouraged to hold regular meetings with parents. o Teachers could also be encouraged to collaborate with health facilities, NGOs and other bodies. o Mechanisms could be put in place to broaden the interface and improve collaboration between the doctors, health workers and teachers at the aimag / soum/ bag level to improve synergy and effectiveness of the programmes. 3.3.1.3 Group 3. SOCIAL WORKERS: Potential role of group Social Workers are attached to the Ministry of Social Welfare and Labour (MoSWL). Most schools have one. Some Family Group Practices also have them. Current activities related to this group o Primarily involved with problem solving when social problems arise. o Interact with teachers and parents (e.g. meetings in schools and house hold visits) but generally in the context of problem solving. Potential actions for consideration o The role of social workers could be expanded to go beyond problem solving to acting as an interface between the school and the doctor/health sector and parents. o They could be involved in reaching out to Most at Risk Adolescents (MARA) in the community. o Their capacities would need to be built (through pre-service and inservice education using traditional and distance education approaches), on identifying, managing and when appropriate referring adolescents with psycho-social and other problems to appropriate service providers. 3.3.1.4 Group 4. NGOs/CIVIL SOCIETY BODIES Potential role of group NGOs and civil society bodies are relatively new in Mongolia. There are a number of NGOs - including INGOs - and civil society bodies like churches and women's groups. Some of them are working in the field of adolescent health, at the aimag and soum level. They could be encouraged and supported to make a stronger contribution, well coordinated with the government. Current activities related to this group o There is little information at hand on what is being done. o International NGOs such as World Vision and Save the Children are providing information and services, but this needs to be verified. Potential actions for consideration o NGOs and civil society organizations could be brought together in a network or consortia so that they would work effectively together. o Collaborative mechanisms could be put in place to between MoH and NGOS and civil society bodies in order to utilize their presence and influence in the communities they serve. o They could reach out to families and adolescents – especially those who are marginalized to prevent problems and to respond to problems when they occur. . . - 22 - - 23 - 3.3.1.5 Group 5. INSPECTORATE AGENCIES: Potential role of group o These agencies are charged with enforcing food safety and security, alcohol and tobacco control. Therefore, their staff could play a vital role in implementing the good policies that exist in these domains. What is currently being done? o Very little is being done to enforce protective policies that contribute to the health of adolescents. Potential actions for consideration o Mechanisms could be put in place for the inspectors to meet with adolescents (in schools, colleges, and other settings ) to discuss on prevailing laws and norms whether they could encourage compliance to laws and policies. o They could do more to monitor whether laws and policies are being followed, and hold violators to account. . 3.3.1.6 Group 6. HEALTH WORKERS: Potential role of group To reach the large number of adolescents, various categories of health workers –doctors, nurses, midwives, assistants to nurses, bag feldshers – would need to provide the bulk of the services to adolescents and young people. MoH should see these different health workers as a ‘first port of call’ for adolescents, particularly for curative services. What is currently being done ? o There are 18 AFHS clinics (including 12 supported by UNFPA) that provide services – mostly related to SRH – to adolescents. The doctors of these clinics and, in some cases, other staff have undergone orientation on adolescent health and AFHS. However, services have not been scaled up. o The health providers from these AFHS clinics carry out some activities in schools and communities in their catchment area, particularly on sexual and reproductive health. Potential actions for consideration o The provision of AFHS could be scaled up. Appropriate national and aimag level plans that are in line with a primary health care approach could be drawn up and implemented for systematic and consistent scaling up. At the soum level, bag feldshers should be utilized to provide community based preventive and curative health services to adolescents..At least 2-3 health workers at the soum level and 4-6 in each aimag hospital could be oriented to the needs of adolescents and have the skills to provide adolescent friendly health services.. o 'Resource centres' at the secondary level, and tertiary level referral centres could be developed to respond to those adolescents whose needs and problems cannot be met at the primary level. o Collaboration between the relevant programmes could be improved at the central, aimag and soum levels. At present, most programmes are overly ‘vertical’ and rarely collaborate with others; o Collaboration between health, education and other sectors could be enhanced and streamlined to improve synergy between health providers and teachers, social workers, NGOs, others. Health workers could support these partners by: providing evidence to inform policy and programming; assisting with advocacy and mobilization; supporting development of materials for teachers, students, parents; supporting capacity building efforts; collaborating for demand generation for AFHS; and developing and supporting referral mechanisms from educational institutions and other agencies to health facilities/AFHS centres. - 23 - - 24 - 3.3.1.7 Group 7. PEERS Potential role of group Peers, that is, adolescents themselves, play a critical role - potentially positive or potentially negative in adolescent health. With their genuine, continual engagement, coupled with building their understanding and skills, adolescents could help support their peers in making healthy choices, and offering the friendship and support to those in need. Current activities related to this group o Adolescents are not routinely involved in health activities, although many stakeholders identify them as a key group. Having said that some organizations such as UNFPA do involve adolescents actively in their activities. Potential actions for consideration o Adolescents could be invited to provide their perspectives on health and health needs/preferences, help draft information, education and communication materials, and use their creative potential to develop interventions that are readily understood and appreciated by peers. o Adolescents, if properly trained and supported, could play a useful role as peer educators, as recuiters for counseling and health services and as providers of some of this themselves. - 24 - - 25 - References 1. The Government of Mongolia (2009). The Second National Mental Health Program 20102019, Ulaanbaatar, Mongolia. 2. Global School-based Student Health Survey Mongolia (2010). WHO. 3. Lois Lambert, Sovd Tugsdelger, and Don Hinrichsen (2004). Creating a Culture of participation Voices of Mongolian Adolescents Telling the UN story, Ulaanbaatar 4. WHO, MoH Mongolia (1997). Report: KAP survey on adolescent reproductive health, p.39. 5. Sumberel, N and Oyunbileg, S (2002). A case study on Adolescent Health and Development, Ulaanbaatar , Mongolia 6. WHO and MOH (2006) WHO-AIMS Report on Mental Health System in Mongolia. Ulaanbaatar. 7. Dr. Tsetsegdary, G (2009) Mental Health Progress Report, Ulaanbaatar, Mongolia 8. Key informant presentation, 22 June 2010 workshop, RPR Adolescent Health. Reference not provided. 9. Mongolia Current Status of Alcohol Policy (2010), presentation to: Regional Meeting on Sustainable Alcohol policy, April 2010, Bangkok Thailand 10. National Program on Prevention and Control of Alcoholism 2003-2012 11. From Alcohol Background Paper, p. 2, (iii) Determinants, and p. 14 Evidence basis, item 1.2.6. This may be the same source from an organisation that changed its name from “Center of Health Management, Information and Education” to “NCCD”. Year appears to be 1997. 12. MoH, PHI and WHO (2006) Mongolian STEPS Survey on the Prevalence of Noncommunicable Disease Risk Factors 2006. Ulaanbaatar Mongolia 13. From Alcohol Background Paper, p. 17, Task (i): Assessment in 2007 … source: Midterm report of program evaluation. 14. World Health Organization (2009). WHO report on the global tobacco epidemic, 2009: Implementing smoke-free environments. WHO: Geneva. 15. MoH, WHO, and PHI (2009). Global Tobacco Surveillance System- Mongolia, 2007. Ulaanbaatar, Mongolia 16. Rudatsikira E, Dondog J, Siziya S, Muula A S (2008). Prevalence and determinants of adolescent cigarette smoking in Mongolia. Singapore Med J. 2008; 49 (1) : 57 17. The Government of Mongolia (2005). Laws of Mongolia: Law on Tobacco Control. Chuluunbar. Ulaanbaatar, Mongolia 18. Oumar Ba ( 2008)Challenges of Tobacco control in low/middle-income countries. Simon Fraser University. 19. WHO (2002), Sexual and Reproductive Health of Adolescents and Youths in Mongolia, Ulaanbaatar, Mongolia 20. UN Common Country Assessment (2007) 21. National Food Security Programme 2009-2016 22. National Statistics Office and UNFPA. (2008) Reproductive Health Survey 2008. Ulaanbaatar. 23. National Statistics Office and UNFPA. (2003) Reproductive Health Survey 2003. Ulaanbaatar. 24. Mongolian Federation of Obstetricians and Gynecologists, UNFPA. (2005) Report on Situation Analysis to introduce RTI/STI prevention service through social franchising among the young people. [http://mongolia.unfpa.org/drive/RTISTISituationAnalysisreport_ENG_2006.pdf] 25. Amanda B. Roberts, C. Oyun, E. Batnasan, Lory Laing. (2005) Exploring the social and cultural context of sexual health for young people in Mongolia: implications for health promotion. Social Science & Medicine. 60, 1487–1498 - 25 - - 26 - 26. HMIEC, MFOS, MSF (1999). Report: National survey among youth of 15-25 age group on STIs/HIV/AIDS prevention. 27. MOH.(2009) Health indicators 2009 28. UNICEF, 2005 Mid- term report. (incomplete reference, given on p. 8, Background Paper, SRH and HIV/STIs) 29. UNFPA (2008 ) Survey report of needs assessment of knowledge, attitude, and behavior amongst illiterate youth, youth who dropped out of school and youth with disability aged 15-24 ,Ulaanbaatar, Mongolia 30. National Committee to coordinate the activities related to HIV/AIDS.(2010) The National Strategic Plan on HIV/ AIDS and STIs 2009-2015, Ulaanbaatar, Mongolia 31. Second Generation HIV/STI Surveillance Report (2007). Ulaanbaatar, Mongolia 32. MOH. (2007) The Third National Reproductive Health Programme of Mongolia 20072011. Ulaanbaatar, Mongolia 33. Government of Mongolia (2005). Ministry of Health. Health Sector Strategic Master Plan 2006-2015, Ulaanbaatar. - 26 - 27 ANNEXE List of participants involved in the Rapid Programme Review, and organisations represented (Monday 21 June and Tues-Wed 22-23 June) Participants to introduction of the "Rapid Programme Review on ADH" (Monday, 21 June 2010) N Names Organizations o 1 R. Molor 2 S. Otgonsukh Global Fund National Center for Communicable Diseases (NCCD) /HIV 0 3 O. Baatarjav National Center for Mental Health (NCMH) 4 Z. Tuya National Center for Mental Health (NCMH) 5 D. Enkhtuya National Center for Mental Health (NCMH) 6 N. Tuya National Center for Mental Health (NCMH) 7 N. Altantsatsral Doctor, Secondary School no. 5 8 Doctor, Secondary School no. 5 A. Tsiiregzen 9 G. Erdenetsatsral Doctor, Secondary School no. 5 1 J. MunkhAldar Student, Secondary School no. 39 1 R. Galbadrakh State Research Center for Maternity and Child Health 1 D. Mandakh State Research Center for Maternity and Child Health 1 O. Tuul Bayanzurkh district, Health Department 1 N. Tuya Sukhbaatar district, Health Department 1 M. Tseveen Chingeltei district Health Department 1 2 3 4 5 27 28 1 D. Enkhmyagmar Public Health Institute 6 1 Sh. Tegshbayar City Health Department 7 1 Munkhjargal 1 B. Baatarkhuu 8 Songino khairkhan district 9 0 2 N. Radnaakhand Health Sciences University 2 L, Oyunaa Health Sciences University 2 B. Manlai Health Sciences University 2 Davaadorj Health Sciences University 2 G. Soyolgerel Ministry of Health, Mongolia 2 Enkhmyagmar 1 2 3 4 5 6 2 B. Tsogzolmaa WHO 2 Tuul 2 Munkhzul WHO 2 B. Chimgee Health Sciences University 3 S, Gonchig Health Sciences University 3 Sh. Oyunkhuu Health Sciences University 7 8 9 0 1 2 3 G, Tsetsegdary Ministry of Health, Mongolia 3 Sh. Enkhbat Ministry of Health, Mongolia 3 D. Baigalmaa Ministry of Health, Mongolia 3 4 28 29 3 Otgonjargal Ministry of Health, Mongolia 3 Jargal Health Sciences University 3 Mibu Toyoda Save the Children 5 6 7 8 3 Victoria Murlagh Save the Children 3 D. Odgerel Save the Children 4 Shibaru 9 0 1 4 G. Uranchimeg UNFPA 4 J. Batjargal 4 T. Navchaa 3rd Project for Health 4 Otgon Health Sciences University 4 Salik Govind WHO 2 3 4 5 List of participants to workshop (22-23 June 2010) held in Terelj Bumban N Names Organizations o 1 R. Molor 2 S. Otgonsukh Global Fund National Center for Communicable Diseases (NCCD) /HIV 3 O. Baatarjav National Center for Mental Health (NCMH) 4 N. Altantsatsral Doctor, Secondary School no. 5 5 Doctor, Secondary School no. 5 A. Tsiiregzen 6 D. Altantsetseg Dundgobi aimag, Health Department 7 Chingeltei district Health Department M. Tseveen 29 30 8 R. Galbadrakh State Research Center for Maternity and Child Health 9 D. Mandakh State Research Center for Maternity and Child Health 1 Z. Tuya National Center for Mental Health (NCMH) 1 D. Enkhtuya National Center for Mental Health (NCMH) 0 1 2 1 S. Yagaanchimeg Dundgobi aimag, Health Department 1 O. Tuul Bayanzurkh district, Health Department 1 N. Tuya National Center for Mental Health (NCMH) 3 4 5 1 B, Tsegtsbayar Huvsgul aimag, Health Department 1 Sukhbaatar district, Health Department P. Tuya 6 1 D. Enkhmyagmar Public Health Institute 7 1 J. MunkhAldar Student, Secondary School no. 39 8 1 Huvsgul Health Department S. Narantuya 9 2 Ts. Chuluuntsetseg Sukhbaatar aimag Health Department 0 2 Sh. Tegshbayar City Health Department 1 2 Songino khairkhan district B. Baatarkhuu 2 2 N. Radnaakhand Health Sciences University 3 2 B. Tsogzolmaa WHO 4 2 Tuul 2 Munkhzul WHO 2 L, Oyunaa Health Sciences University 5 6 30 31 7 8 2 G. Erdenetsatsral Student, Secondary School no. 5 2 Ministry of Health, Mongolia G. Soyolgerel 9 31