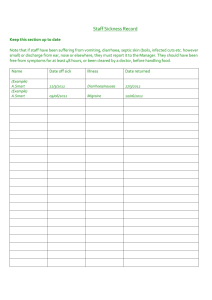
ge/02(p) chronic diarrhoea and malabsorption in children
advertisement

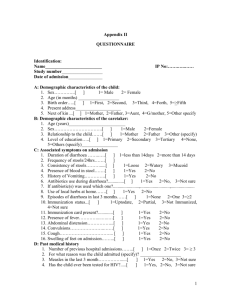
GE/01(O) CLINICO-EPIDEMIOLOGICAL STUDY OF CELIAC DISEASE IN STATE OF RAJASTHAN S.D.Sharma , Anurag Sarna , Vijay Sharma Dept. of Pediatrics, Sir Padampat MCHI, Sawai Man Singh Medical College, Jaipur "Celiac disease is an important cause of malabsorption in children & results from sensitivity to gluten . Aims and Objectives : The study was conducted to determine incidence of celiac disease in children presenting with chronic diarrhoea, abdominal distension, anemia, malnutrition and short stature. Material and Methods: The study was carried out at pediatric-gastroenterology centre, SMS Medical College, Jaipur from January-2003 to August-2005.Children <15 yr of age, attending the OPDs & indoor's with complaints of chronic diarrhoea, abdomen distension, anaemia, malnutrition, short stature & FTT were included. A detailed clinical history and examination was done with special attention to anthropometry, vitamin deficiency signs and anaemia. CBC, PBF, Serum calcium, electrolytes, MT and CXR were done wherever indicated. Celiac disease was diagnosed by modified "ESPGAN" criteria . All children were subjected to upper G.I. endoscopy with duodenal biopsy. Serological markers, Anti EMA, TtG and antiglydine antibodies were done in biopsy positive cases . Positive cases were put on Gluten Free Diet (GFD) and all showed a positive response with satisfactory compliance. Results : Out of 300 children presenting with chronic diarrhea, abdominal distension, anaemia, malnutrition, short stature, or FTT, 102 (34%) patients were diagnosed as celiac disease (CD). Majority of CD cases (74/102) were between 1-5 years of age with 54 males and 48 females. Abdominal distension (102), anaemia (102) and chronic diarrhea (98) were the commonest clinical features, followed by malnutrition (96) and short stature (91). Few cases showed features of hypokalemia and celiac crisis. Familial occurrence was seen in three. Out of 102 biopsy proved cases 96 were IgA EMA positive and 77 for TtG. Conclusion : Celiac disease is not uncommon in Rajasthan where wheat is a staple diet. The common presentations are abdominal distension, chronic diarrhoea, anaemia, malnutrition and short stature. All patients improved on GFD." GE/02(P) CHRONIC DIARRHOEA AND MALABSORPTION IN CHILDREN Puneet Jairath, Seema Rai, Ravneet Kaur, Rahul Gandhi, K.K.Locham Deptt. of Pediatrics, Govt. Medical College/Rajindra Hospital, Patiala - 147001 Objectives : To evaluate the clinical and aetiological profile of chronic diarrhoea and malabsorption. Methods : The study was conducted for a period of 7 months from January to July 2005. 14 children from 1-15 years of age, admitted in department of Pediatrics, Govt. Medical college and Rajindra Hospital, Patiala were the subjects of study. Age, sex, presenting complaints, laboratory investigation like haemoglobin estimation, PBF, ESR, stool complete examination, urine culture & sensitivity, mantoux test, X-ray chest, Barium meal studies, anti-endomysial antibodies (anti-gliadin antibodies were not estimated ) were recorded in the pretested proforma. Results : Out of 14 children, 9 (64.3%) were males and 5 (35.7%) were females. 11 (78.5%), 2(14.2%) and 1(7.4%) children were in the age group of 1-5 years , 5-10 years and 10-15 years respectively. Presenting complaints were loose stools , fever , abdominal distension and inability to gain weight in 11 (78.5%), 7(50%) , 3 (21.4%) , 2 (14.2%) cases respectively. 11(78.5%) cases had anaemia out of which mild, moderate and severe anaemia were seen in 8 (57.1%), 2 (14.2%) and 1(7.1%) cases respectively. 7(50%) cases had infective diarrhoea , 5 (35.8%) had tubercular enteritis while 2 (14.2%) children suffered from gluten enteropathy. Conclusions : Tuberculosis was the predominant cause of malabsorption while chronic diarrhoea was mainly caused by gluten enteropathy and tuberculosis. GE/03(P) CHRONIC LIVER DISEASE IN CHILDREN: CLINICAL PROFILE AND HISTOLOGY Archana Kher, Sachin Dhole, Meenakshi S. 6/A Anand Bhavan, 36 rd , Bandra , Mumbai 400050. Aims and Objectives: To study the clinical profile of disorders of the hepatobiliary system, evaluation of findings on biopsy. To assess the prognosis, outcome and effects of therapy on chronic liver disease. Material and methods: A prospective study was done where 55 children were enrolled in a period of 24 months. Symptoms like jaundice, bleeding, abdominal distension, high colored urine, clay coloured stools, edema, altered sensorium were recorded. Family history, previous therapy, history of intrauterine infection was also noted. A detailed general examination, signs of liver cell failure, evaluation of malnutrition , abdominal examination and other relevant systemic findings were noted. Investigation profile included hemogram , serum biochemistry, liver function tests, blood NH3, TORCH, protein EPP, autoimmune studies, S Cuo and urine Cu. Metabolic studies were done in a few cases. Isotope scans [Tc99sulfur colloid] USG were done . A percutaneous liver biopsy was performed in all cases, in those who were critically ill it was done post mortem, the biopsy was stained with hematoxylin and eosin and in some cases PAS, Prussian blue and reticulin stain were used. Results: 55 cases comprised of 33 males and 22 females, a maximum of 34.5% cases were in the age group of 6 to 12 years.Jaundice and abdominal distension were present in 21 and only jaundice in 19, bleeding manifestations 25, encephalopathy 16 cases of which 3 children died. Hepatomegaly was noted in 41, splenomegaly 33 cases. A USG detected HS megaly 28, hepatomegaly 17, normal USG in 10. The liver echotexture was as follows coarse 29, bright 16, normal 19 cases.2/45 had positive tests for hepatitis B infection, 5/13 had IgM HAV positive. S Cuo was abnormal in 15/31.These cases underwent further testing with urine copper, a slit examination, dry copper weight from liver [6/13 had high values.] markers for autoimmune disease like ANA, ASMA were abnormal in 7/10. 9 phytate scans and 10HIDA scans were done. Histology of the liver revealed abnormal architecture in 32, cholestasis 27, ballooning in 41, inflammation in 44, necrosis in 15 , fibrosis 40, cirrhosis 23. Special stains were done on 13 biopsies. A final diagnosis of hepatitis was made in 9, automimmune liver disease 6, Wilsons disease 12, alpha 1 antitrypsin deficiency 2, glycogen storage disease 2, IU infections 4, neonatal hepatitis 5, extrahepatic biliary atresia 4, TB 4, neutral lipid storage disease 1 case. Chelation therapy with penicillamine was given to those with Wilsons disease, steroids and immunosuppressives ,dietary modifications were advised as per the diagnosis. Conclusions: Any child with prolonged or recurrent jaundice , family history of a metabolic liver disease must be evaluated in detail. A proper investigative protocol including histology is mandatory for a conclusive diagnosis , therapy and counseling. GE/04(P) CLINICO-EPIDEMIOLOGICAL STUDY OF PERSISTENT DIARRHOEA WITH SPECIAL REFERENCE TO GIARDIASIS. S Gupta, VN Tripathi, R.P. Singh, GC Upadhyay Department of pediatrics and Microbiology, GSVM, Medical college, Kanpur Objective : (1) To Know the prevalence of persistent diarrhoea in children less than 5 years in hospital and OPD setting. (2) To study the clinical profile of persistent diarrhoea in children less than 5 years. (3) To study the prevalence and role of giardiasis in children with persistent diarrhoea. Design : Prospective Hospital based study. Setting : Patients attending OPD and admitted in children hospital, GSVM Medical College, Kanpur Methods : 429 children of different types of diarrhoeal diseases have been included with particular references to their morbidity pattern in persistent diarrhoea and giardiasis. Only the children <5 years of age were taken in this study. RESULTS : Study revealed that prevalence of persistent diarrhoea in diarrhoeal diseases is 17.5% with overall prevalence of persistent diarrhoea 5.7%, 52% of patients presenting with persistent diarrhoea were in the 0-9 month age group with 96% less than 18 month of age there were 56% of male as compared to 44% of female i.e. male preponderance. Among the children with persistent diarrhoea 50% had grade II & III malnutrition. On stool microscopic examination 32% patient had parasite in their stool microscopic examination in which 16% had giardia lamblia, 12% had Entamoeba histolytica and 4% had ova of ascaris. Out of 12 cases of patient with Giardia positive persistent diarrhoea case 7 (58.4%) were in age group of 1-3 and there was male preponderance. 100% giardia positive cases of persistent diarrhoea had loose stool (83.3%), 10 cases had fatigue & abdominal pain, 7 (58.3%) had bloatedness, 5 (41.6%) had diarrhoea alternating with consipation, 3 (25%) cases had vomiting and only 1(8.3%) case had fever. Conclusion : Persistent diarrhoea is one of the major contributors to protein energy malnutrition, growth failure and ill health in infancy and preschool age group. Young age malnutrition, impaired cell mediated immunity, recent acute diarrhoea, recent introduction of animal milk, drug used during acute phase are the risk factor for persistent diarrhea. Giardia lamblia as a common cause of persistent diarrhoea in infancy and children GE/05(P)CLINICAL PROFILE OF CASES WITH CELIAC DISEASE N. P. Chhangani, Pramod Sharma Navratan Sharma, Anurag Meena,Ravi Bhatia,Bd Gupta Umaid Hospital,Dr SN Medical College,Jodhpur Celiac disease is a genetic, immunologically mediated proximal small bowel enteropathy that causes malabsorption. The condition is characterized by sensitivity to gluten and is suspected in children having chronic diarrhoea and growth failure. The disease is associated with antibodies to gliadin and the enzyme tissue trans- glutaminase.The disease is high in areas where wheat is the staple diet. Methodology: Children less than 15 years of age attending the OPD with complaints of chronic diarrhea, anemia and growth failure were evaluated.Nutritional,hematological and anthropometrical parameters noted and features of vitamin deficiency looked for. All suspected cases were subjected to tissue transglutaminase antibody titers by ELISA method. Cutoff values were 10units /ml and only children with positive antibody test were included. Age and sex matched control group was also similarly evaluated. Results: - Forty three cases with a positive serology constituted our study group.Mean age at presentation was 6.5 +2.2 yrs.and male female ratio was 1.57:1. Majority of cases were from urban areas. Chronic diarrhea was present in 100% cases followed by abdominal distension in 70%, growth failure in 59%, vomitings in 30.5%, pain abdomen in 47.2 %, anorexia in 52.7%. Signs noted were pallor, stunted growth, hair changes, skin changes, nail changes, edema and vitamin deficiency. Features of vit A deficiency were most commonly seen. Mean duration of symptoms was 3.3 +1.2 years. Serum transglutaminase antibody titters were 54.2 +4.7 U/ml. 25% cases were severely malnourished and 25%moderately malnourished. Mean height of cases was 96+12.5 cms and that of control was 107+11.7 cms...BMI (Body mass index) of cases and control were 12.3+2.2 and 15.6+2.2 respectively.Mean Hb of cases and controls were .2+1.02Gm% and 9.97+1.01Gm% respectively with microcytic hypochromic anemia being the most common. Conclusion:Prevalence of celiac disease is high in Rajasthan and clinical picture compatible with the disease coupled with positive serology can help reach a diagnosis and tissue transglutaminase can be taken up as a scrrening test where facilities for biopsy does not exist. GE/06(O) CLINICAL, BIOCHEMICAL AND ETIOLOGICAL PROFILE OF FULMINANT HEPATIC FAILURE OF VIRAL ETIOLOGY IN CHILDREN Deepak Bhat, Gurdeep S. Dhooria, B.K. Jain, B.S. Dhillon Deptt of Pediatrics, Dayanand Medical College and Hospital, Ludhiana 141012 Viral Hepatitis is a major health problem endemic in many parts of the world. Fulminant viral hepatitis is a rare condition that occurs in only 1% of patients hospitalised with an acute viral hepatitis. There is a paucity of literature describing spectrum of fulminant hepatic falure in children in India. Objective: To study the clinical, biochemical and etiological profile of fulminant hepatic failure( FHF) of viral etiology in children.. Methods: The study was conducted in 30 children aged group between 1- 15 years admitted with FHF of proven viral etiology in Dayanand Medical College and Hospital, Ludhiana from May 2000 to October 2001. FHF was defined as occurrence of encephalopathy within eight weeks of onset of jaundice with no evidence of pre-existing liver disease. A detailed clinical evaluation including history, physical signs, staging of hepatic encephalopathy with relevant investigations and viral markers were entered in a pretested proforma. Results:.Twenty nine patients(96.7%) had enterically transmitted hepatitis. Viral markers for HAV alone was positive in 20 patients (66.67%) and in combination were positive in 28 patients ( 93.3%), HEV in 7 patients (23.3%) and HBV in 5 patients (16.7%). Eight patients had mixed viral infections. The clinical features included fever and jaundice(100%), anorexia (83.3%), vomiting (76.7%) , nausea (73.3%). Complications seen were cerebral edema (53.3%), decreased urine output (30%),GI bleeding(16.6%) and septicaemia (16.6%). The overall survival rate of FHF was seen to be 73.3%. Conclusions : HAV was found to be the commonest viral infection causing FHF either alone or in combination with others. Importance of vaccination of children with HepatitisA and HepatitisB vaccine and improvement in sanitation in prevention of FHF cannot be overemphasised. GE/07(P) CLINICAL PROFILE OF LIVER ABSCESS IN CHILDREN H.S. Agarwal, K. Rajeshwari, A.P. Dubey, P. Kumar Department of Pediatrics, Maulana Azad Medical College and associated Lok Nayak Hospital, New Delhi -110002 Introduction: Liver abscess is an uncommon but life threatening disease in children. The clinical profile and outcome of 13 children presenting with liver abscess is described. Aims and objectives: To study the clinical features, etiology and clinical course of liver abscesses in children. Materials and methods: Case records of 13 children with liver abscess presenting between March and September 2005, were analyzed retrospectively. Results: The mean age at presentation was 4.61 yrs (range 1-12 yrs) with a male: female ratio of 9:4. Average duration of symptoms prior to presentation was 10.92 days (range 4-45 days). Common presenting complaints were fever (100%), abdominal pain (84.6%) and anorexia (76.9%). Respiratory symptoms were present in only 3/13 (23%) patients, one patient had a preceding history of diarrhea. Physical findings at presentation were fever and hepatomegaly (100% patients). Importantly, only 3/13 patients had mild malnutrition, rest had normal nutritional status. Investigations revealed anemia (84.6%), leucocytosis (69.2%), neutrophilia (38.4%). On ultrasound, 9 children had solitary abscess in the right lobe, 3 in the left lobe while one had multiple abscesses in both lobes. Pus culture revealed organisms in 3/11 patients, namely Staphylococcus aureus, Coagulase negative staphylococcus and Klebsiella. Amebic serology was negative in all the cases. Antibiotic therapy alone was curative in 2 cases while some form of drainage (needle, percutaneous catheter) was required in the rest. Complications encountered were rupture into the pleural cavity, bleeding after percutaneous catheter insertion in one case each. One patient had associated transient hypertension. All the patients survived. No predisposing cause for liver abscess could be ascertained in any of the patient. Conclusion: Liver abscess is a serious illness which can occur in well nourished children without any predisposing cause. Appropriate antibiotic therapy along with effective drainage can greatly reduce the mortality of this condition. GE/08(P) HIRSCHSPRUNG DISEASE- ENTEROCUTANEOUS FISTULAE FORMATION - A CASE REPORT Karanjit Singh, Rajneesh Kapoor Kapoor Children Hospital, Department of Paediatrics / Govt. Medical College, Amritsar. A 25 day full term neonate with IUGR was admitted in tertiary care set up on 27/10/04 with complaints of abdominal distension and difficulty in respiration. The neonate was admitted previously in some hospital with H/O perinatal asphyxia and distension abdomen but recovered well. Two patches of reddish discoloration on lower anterior abdominal wall and distension abdomen was again observed for which patient which was referred to this hospital. General physical examination revealed toxic looking neonate with respiratory distress and distension abdomen. Two areas of cellulitis, 2.5-3.5 cms each were present on either side of anterior abdominal wall. On P/R examination, rectum was found to be gripping over the finger. The areas of cellulitis gave away on 5th day of admission creating enterocutaneous fecal fistulae. The neonate undergone exploratory laprotomy on 6/11/04. Investigations revealed evidence of septicemia (CRP-35, toxic granulations and band forms), thrombocytopenia, multiple air fluid levels in x-ray abdomen and long segment type of hirschsprung disease on barium enema study. Peroperative findings revealed free fecal matter in peritoneal cavity. Dense adhesions between loops of intestine were found which permitted minimal adhesionolysis. Fecal collections in peritoneum were drained out and drains were kept one in each iliac fossa and wound closed. However, child died 14 days after surgery. Hirschsprung disease results from absence of ganglion cells and occurs as short segment disease or long segment disease. The most serious complication is enterocolitis, which occurs in 17-25% of cases. In the present case, inflamed walls of gut adhered to anterior abdominal wall causing necrosis of muscles and then wall of abdomen. Then the gut perforated through anterior wall creating two enterocutaneous fistulae through which child passed stools in pelvis as well as outside abdomen. Child was also passing stools per rectum. The case is being reported for its rarity. GE/09(O) HEPATIC INVOLVEMENT IN TYPHOID FEVER-A PROSPECTIVE STUDY TO DETERMINE CLINICAL SIGNIFICANCE AND OUTCOME Deepti Chaturvedi, Devendra Mishra, R.B. Gupta, D.S. Chauhan, Manoja Das, Mukta Mantan Department of Pediatrics and Laboratory Medicine*,Chacha Nehru Bal Chikitsalaya (Maulana Azad Medical College),Geeta Colony,Delhi-31 Objective: To determine the clinical significance and outcome of hepatic dysfunction in typhoid fever. Design and Settings: Prospective study, Government Pediatric hospital attached to a medical college. Methods: All children diagnosed and treated as typhoid fever over an 8-month period (27th January to 26th September 2005) underwent a detailed clinical examination and relevant investigations. Liver function tests were done at the time of admission in all these patients. Results of the investigations and various other patient characteristics including age, sex, presenting complaints, clinical findings, bacteriological profile, serological profile and response to treatment were added to a structured proforma. The data was statistically analysed to determine the relationship between various clinical and bacteriological characteristics and hepatic dysfunction at admission. Results: There were 52 patients with enteric fever of which 23 (44%) were culture positive and 43 (82.7%) were Widal positive. Hepatic dysfunction in the form of deranged liver function tests (LFT) was observed in 12 patients (23%), of which seven (58.3%) were culture positive. Only three of these (25%) presented with history suggestive of acute hepatitis (fever, jaundice, hepatomegaly) and one had serological evidence of acute hepatitis, in addition to a positive blood culture for S.typhi. The overall complication rate was low in our sample. The mean time to defervescence, rate of complications, culture positivity, and frequency of MDRST isolation were similar between the patients with hepatic involvement and the rest of the sample. Conclusions: Hepatic involvement, as evidenced by deranged LFT is common finding in enteric fever but doesnot seem to affect the outcome. However, coexisting hepatotropic virus infection (especially those acquired oro-fecally) may rarely be present. GE/10(O) DIAGNOSTIC AND THERAPEUTIC ERCP IN CHILDREN: EXPERIENCE AT A TERTIARY REFERRAL CENTER A.S. Puri, M. Wadhawan, Y.K. Sarin, L.B. Gupta Deptt. of Gastroenterology, GB Pant Hospital & Deptt. of Pediatric Surgery, Maulana Azad Medical College, New Delhi-110002 Objectives of the study: Despite increasing use of therapeutic ERCP in children, the data available in literature is sparse. We report our experience of therapeutic ERCP in pancreatico-biliary disorders in children. Methods used: 50 ERCP procedures were performed on 47 children at a tertiary referral centre between 2002 and 2005. Thirty-seven of these procedures were done for disorders of the biliary tract whereas the remainder had pancreatic disease. Baseline demographic data and ERCP findings were recorded and patients were followed up for 3 months after procedure. Results: 47 patients (M:F 19:28;Mean age 14.5 years) underwent therapeutic ERCP procedures over 41 months. Successful opacification of the desired duct was achieved in 8 of 50 procedures (96%). The commonest indication for therapeutic procedures was choledocholithiasis. Eighteen sphincterotomies were carried out for various indications. Successful stone extraction was possible in the same sitting in 81% of children referred to us for therapeutic ERCP. Major complications occurred in only 2 procedures (4%), only one of which warranted surgical intervention. In 11 of 34 (32%) children, the referral diagnosis based on clinical and ultrasonography was revised after the ERCP, which underscores its utility as a highly specific diagnostic modality. Current trends are indicative of a greater role of therapeutic ERCP in children and a decline in its use as a mere diagnostic modality in the wake of excellent imaging modalities as seen in adults. Conclusions: ERCP is very safe and useful in the management of various liver, biliary and pancreatic disorders in children. Complication rate of ERCP in children is low in expert hands. GE/11(P) DIARRHOEAL DISEASES: CLINICAL SPECTRUM IN MALNOURISHED CHILDREN. Ravinder K. Gupta Department of Pediatrics, Acharya Shri Chander College of Medical Sciences & Hospital, Sidhra, Jammu-180004 Objective: To delineate clinical spectrum of diarrhoeal diseases in malnourished children. Design: Prospective study Setting: Indoor and Outdoor wing, Department of Pediatrics, ASCOMS Hospital, Sidhra, Jammu. Methods: The study was conducted over a period of one year in which 260 malnourished children of age group 0-5 years were taken at random. These children were assessed regarding various feeding habits, type of diarrhoea and dehydration. A detailed clinical examination was also conducted.Results: Out of 260 malnourished children taken for study in 125 (76 males and 49 females) had diarrhoeal disease at the time of admission. Majority 60% of subjects were between 1-2 years, 24% were less than 1 year while rests were above 2 years. The male female ratio was 1.5:1. Out of 125 cases of malnutrition with diarrhoea 32% had acute gastro-enteritis, 30.4% had acute diarrhoea, 24% had acute dysentery and rest 13.6% had chronic diarrhoea. Exclusive breast feeding was a rarity. However 30.4% were breast fed while rests were not at all given breast feeds. Weaning was not started in 20% children, while 44% were weaned before one year of age. On examination 20% had puffy appearance, 13.6% had apathetic look, and 12% were cachexic. Mild, moderate and severe anemia was clinically present in 60%, 32% and 8% children respectively. Vitamin D deficiency features were present in 64% children while vitamin A deficiency features were seen in 28% children. Vitamin B-complex deficiency features in form of glossitis, angular cheilosis, stomatitis, etc. were seen in 19.2%. Respiratory tract signs in form of crepts and wheeze were seen in 10.6% cases. Cardiovascular system examination was almost within normal limits. Hepatomegaly was seen in 16% while splenomegaly was seen in 8% cases. Skin changes were seen in 4%. About 60% had no dehydration, while 28% had some dehydration and rest 12% had severe dehydration at the time of presentation. As per IAP classification, 64% belonged to grade II-III, 28% belonged to grade IV, while rest belonged to grade I. Kwashiorkor was seen in 32% of the subjects. Conclusion:Malnutrition invites diarrhoeal manifestations through different modus operandi and diarrhoea in turn further deteriorates the nutritional status. The observation that in 12.5% of the cases diarrhoea becomes chronic has significant implication. GE/12(P) GASTRIC DUPLICATION CYST PRESENTING AS CONGENITAL DIAPHRAGMATIC HERNIA Anup Mohta, Lalendra Upreti Guru Teg Bahadur Hospital and associated University College of Medical Sciences, Dilshad Garden, Delhi Aim: To present an unusual case of duplication cyst of stomach that presented as congenital diaphragmatic hernia. Methods: An infant presented to the hospital with respiratory distress in the casualty. Clinical signs and diagnostic investigations were suggestive of congenital hernia. At surgery, multiple duplication cysts of the stomach were seen that were successfully excised. Conclusion: A case of uncommon mode of presentation of gastric duplication is presented. GE/13(P) GASTROESOPHAGEAL REFLUX DISEASE: CLINICAL PROFILE AND OUTCOME Maninder S. Dhaliwal, Abhinav Rastogi, Rathika Shenoy, Nutan Kamath Kasturba Medical College, Mangalore, Karnataka- 575001 To assess the clinical presentations and outcome of 58 children diagnosed to have gastro esophageal reflux disease (GERD) at Kasturba Medical College Hospital, Attavar, Mangalore, Karnataka. Design: A prospective hospital based study. Methods: 58 children diagnosed to have GERD by videofluroscopic studies; between August 2002 and December 2004 were analyzed for clinical presentation and followed up for 6 months. Results: 70 % of children were under the age of 1 year; with majority being less than 6 months with equal sex distribution in all ages. Presenting symptoms were regurgitation (62 %), pneumonia in (48 %), asthma (20%), failure to thrive (20%) and apnea (6%).Regurgitation being a major complaint in 1st 6 months & pneumonia being in next 6 months. The children were treated with first dietary modification and if no subsidence of symptoms occurred, a standard medical & surgical therapy was followed as per individual case requirements. 70 % required drug therapy, which on follow up showed significant improvement in nutritional status and resolution of symptoms. Conclusion: GERD in children may have varied clinical presentations. Early recognition and therapy may suffice in most children. GE/14(P) ORAL MUCOSAL PIGMENTATION A KEY TO DIAGNOSIS IN A CHILD WITH CHRONIC ABDOMINAL PAIN. A CASE REPORT Ann Mathew,Sudhir Joseph,Suman Lata Deptt. of pediatrics and pediatric surgery,St Stephen's Hospital,Delhi-110054 A ten-year-old boy presented to the outpatient department with history of recurrent abdominal pain, nausea and intermittent vomiting for the past 2 years standing. He was admitted to investigate the cause of Failure to thrive and chronic abdominal pain. His weight and height were below the third centile for age. An abdominal ultrasound showed an intestinal intussusception with a pathological lead point. This diagnosis had not been made despite several prior evaluations for episodes of similar symptoms. General examination revealed irregularly distributed light to dark brownish macules of 5mm diameter in the oral mucosa..These had appeared in the past two years. This lead to the diagnosis of Peutz –Jegher syndromeThe child underwent an elective open laprotomy, which revealed ileoileal intussusception On operation, the cause of the invaginations appeared to be 9 polypous formations in the small intestine. Approximately sixcentimeter length of ileum, which was studded with several polyps, was resected and end-to-end anastomosis done. In addition intraoperative endoscopy was done and 5 polyps were removed. PeutzJeghers syndrome is an autosomal dominant disorder characterized by gastrointestinal polyposis and mucocutaneous pigmentation. The natural history is characterized by gastrointestinal complications of occlusion, invagination and hemorrhage in young patients as is manifested by this case. . Treatment requires a combination of endoscopy and laprotomy/laproscopy. A pre- operative diagnosis of the syndrome in a case of chronic intussception helps as whenever operation becomes necessary, a very cautious approach must be advised to preserve as much of intestinal length as possible in these patients who have a lifelong disease which may require repeated operations. GE/15(P) FORME FRUSTE CHOLEDOCHAL CYST Y.K. Sarin Deptt. of Pediatric Surgery, Maulana Azad Medical College, New Delhi-110002 The classical choledochal cyst (CCC) consists of a rounded cystic dilatation of the common bile duct with distal narrowing. Forme fruste choledochal cyst (FFCC) is a variant that has minimal or no dilatation of the extrahepatic bile duct (EHBD) and is associated with pancreaticobiliary malunion (PBMU). The presenting symptoms include recurrent abdominal pain, recurrent jaundice, fever and pancreatitis and these closely resemble those seen in patients with CCC. The differentiation of FFCC from CCC is essentially done on findings of ERCP, MRCP, or intraoperative cholangiopancreaticogram. The cut off diameter of EHBD above which the diagnosis of FFCC is unacceptable has been arbitrarily decided as 10 mm. Other subtle differences that have been noted between FFCC and CCC include higher incidences of dilatation of common pancreaticobiliary channel and presence of protein plugs or debris at the level of common channel in FFCC as compared to the classical choledochal cysts. We report three children with FFCC who were successfully treated by excision of the diseased extra-hepatic biliary duct and hepaticodochojejunostomy. The aim of the presentation is to aware the pediatricians of this rare variant of choledochal cyst that is not a cyst. GE/16(O) ROLE OF PREBIOTICS AND PROBIOTICS IN ACUTE WATERY DIARRHOEA IN CHILDREN AGE 3 MONTH TO 5 YEARS. Singh Karnail, Pannu M.S., Singla Amit. Deptt of Pediatrics, Govt. Medical College, Amritsar, Punjab. Introduction : Diarrhoeal diseases are frequent cause of morbidity and mortality in developing countries like India. ORS is a mainstay of treatment in most of the cases. Recently a lot of interest has been generated in evaluating probiotics in diarrhoea. Continuing in the same direction the present study was conducted using prebiotics and probiotics in deptt of paediatrics , GMC, Amritsar. (ii) Aims and objectives: (a) to see whether prebiotics and probiotics are effective in reducing frequency of stool and duration of diarrhoea ( no of days) in children age 3 months to 5 years suffering from diarrhoea. (b) Whether it is cost effective in acute diarrhoea in developing countries like India. (iii) Material and methods:- One hundred children between 3 months and 5 years with acute diarrhoea were enrolled in a prospective study. Patients were randomly distributed into study group( n=50) and control group( n=50). The control group was given only WHO ORS and study group was given ORS along with a combination of prebiotics and probiotics( streptococcus faecalisT-110( 30 million/0.5g), clostridium butyricumTO-A( 2 million/0.5g), Bacillus mesentrericus TO-A( 1 million/0.5g) and Lactic acid bacillus (50 million/0.5g). The above combination was given in a dose of 0.5 gms thrice daily. Children in two groups were evaluated for decrease in frequency and duration of stools over 5-7 days. (iv) Results: The two groups were statistically similar at the time of admission with respect to age, sex, weight, feeding, vomiting & duration of diarrhoea. Duration of diarrhoea after enrollment was 47.1 hrs (1.96 days) in the study group versus 69.78 hrs ( 2.90 days) in control group. (v) Conclusions: Administration of ORS with pre and probiotics in acute watery diarrhea is safe and results in shorter duration of diarrhea and faster discharge from the hospital showing it to be cost effective as it shortens the duration of stay in the hospital. GE/17(O) RACECADOTRIL - A NEWER ANTIDIARRHOEAL DRUG Nivedita Shenoy , M.L.Kulkarni , Shilpa Deshmukh , Gayathri .K JJM Medical College , Davangere, Karnataka “Racecadotril-a new approach to diarrhoea in children Diarrhoeal disease is a leading cause of illness and death in children in developing countries.Oral rehydration is the mainstay of treatment.However oral rehydration solution doesn’t reduce symptoms of diarrhoea.Racecadotril is a novel drug, an encephalinase inhibitor which reduces intestinal secretion and is a useful adjunct.Objective: To assess the effect of Racecadotril as an adjunct to ORT in young infants and children. Methods: This was a “Randomised Double Blind Placebo Control Trial” conducted in “Diarrhea Treatment and Training Unit” (DTTU) in a district hospital in CGH, attached to JJMMC, Davangere, Karnataka in India between August 2004 and January 2005. Patients eligible for the study were males (to facilitate separate collection of stool and urine), aged six months to two years with a history of acute watery diarrhoea. A total of 32 patients were studied over a period of 6 months. Weight of the stools in grams per stool, number of stools per day at 48 and 72 hours was assessed along with number of days of hospital stay. Results: The mean+SD for the number of days of hospital stay in racecadotril study group was 2.9+0.7 whereas in placebo group was 4.6+ 0 .7. I.V fluid requirement was higher in placebo group, than in racecadotril study group. The number of stools per day in racecadotril study group after 48 hours was 4.3 +/- 3.8 compared to 8.2 +/- 2 .4 in placebo group. After 72 hours, the number of stools per day was 4.1+/3.4 in Racecadotril study group and 6.6 +/- 2 .3 in placebo group. The weight of the stools in grams per stool was 12.7+/-5.6 in racecadotril study group whereas it was 20.7+/-14.1 in placebo group after 48 hours and after 72 hours was 13.1+/-14.7 in racecadotril study group whereas it was 18.1+/-11.3 in placebo group. Conclusion: There was significant reduction in the duration of hospital, I.V fluid requirements, the number of stools per day after 48 hours and 72 hours and weight of stools after 48 hours and 72 hours in racecadotril group. GE/18(P) INCIDENCE OF SECONDARY LACTOSE INTOLERANCE DIARRHOEA AND RELATION TO ITS DURATION IN CHILDREN A. N. Prasad Deptt. of Pediatrics, Military Hospital, MHOW, Indore-453441 FOLLOWING Objective : Lactose intolerance (secondary) following gastroenteritis is a common problem, hampering the refeeding of milk following diarrhea. This study was done to evaluate the incidence of secondary lactose intolerance, following infective diarrhea in children, and to correlate it with the duration of diarrhea. Design : A hospital-based prospective study. Methods : 100 children less than 5 years age, admitted in the hospital with infective diarrhea (clinical and laboratory evidence in form of fever/ dysentery/ pus/mucus in microscopic stool examination/ bacteriological growth in stool culture ) were randomized to receive whole milk (>2gm/kg/day of lactose) immediately after the recovery from diarrhea. Outcome measures in form of abdominal bloating and cramping pain, nausea and vomiting, rumbling, gaseousness, flatulence and diarrhea ; were observed for following (15 minutes to several hours) the milk ingestion. Lactose intolerance was confirmed by lactose tolerance test and stool acidity test. Results : In children with diarrhea of more than 7 days duration, the incidence of lactose intolerance was 35%, whereas it was 15% in children with diarrhea of less than 7 days duration. There was no significant difference between the 2 sexes. Children with diarrhea more than 7 days had significantly higher incidence (20%) of malnutrition, compared to the other group (5%). Conclusion : Acute infective diarrhea of more than 7 days have significantly higher incidence of lactose intolerance. GE/19(O) IS IT POSSIBLE TO PREDICT DURATIONAND COMPLICATION OF ACUTE CHILDHOOD DIARRHEA Munlod S. S., Patel Ab, Dibley Mj,Kulkarni Lr Indira Gandhi Government Medical College, C. A. Road, Nagpur (MS) OBJECTIVE: To identify risk factors for duration and complications of acute watery diarrhoea in underfive year children. DESIGN: Baseline data analysis of a randomized controlled micronutrient clinical trial at a tertiary care hospital, Indira Gandhi Government Medical College Hospital, Nagpur, India. PARTICIPANTS: 300 children aged 6 months to 59 months with diarrhoea < 72 hours. OUTCOME MEASURES : Duration of diarrhea in hours and proportion of complications such as electrolyte imbalance, convulsion, azotaemia, hemolytic uremic syndrome, abdominal distention and sepsis. RESULTS: Thirtyfour base line and …. characters at 6 hour observation were studied for their probable association with duration and complication of acute watery diarrhea. In multivariate analysis factors associated with duration of diarrhea were: increased duration of diarrhea and vomiting before admission, higher rectal temperature, lower zinc level, presence of red cells in stools at admission. At 4 hours the factors were increased stool volume, urine output and oral intake. Weight fall and dehydration status at 6 hour were also associated with increased duration of diarrhea. Complications were predicted using multivariate logistic regression by only baseline factors – number of loose motions before 24 hours of admission [OR1.16 (1.02. 1.33)] and dehydration status at admission [OR 7.1(1.54, 33.1)]. 4 or 6 hour assessments did not contribute to detection of complications some of which were experienced before 4 hours. CONCLUSIONS: Accurate assessment at the time of admission of the above risk factors will help in predicting complications and duration of diarrhoea and decision on timing of observation or discharge of the patient. GE/20(P) A STUDY ON RECURRENT ABDOMINAL PAIN IN CHILDREN. Rabindra Sahoo, S.K.Agrawala, S.K.Satpathy, G.C. Samal Aim:-To know the epidemiological factors ,aetiology and clinical manifestation Of Recurrent Abdominal Pain (RAP) Design:- Prospective study Method:-300 children (5-15 years) admitted to pediatrics department of MKCG Medical college from august 2004 to July 2005 with chief complain of abdominal pain were examined & detailed laboratory investigation done. Result: In this study 180 Children presented with RAP out of a total of 300 cases of pain abdomen. The peak incidence of RAP was between 7-10 yrs with male predominance in younger age group & female predominance in older age. Loose motion, vomiting & abdominal distention were common associated findings. Most common site of RAP is periumbelical. Pallor & under nutrition were marked in 60.18% & 40.28% respectively. Eosinophilla was an important hematological finding in 32.14% cases followed by raised ESR (26.40%). Non-organic RAP (NORAP) is the commonest aetiological agent (40.62%) followed by Giadiasis & sickle cell disease. Organic RAP is more frequently associated with bowel complaint, tenderness, rigidity & pain interfering with sleep, as compared to NORAP where body ache was a typical feature. Both home & school related psychosocial problems were more marked in NORAP than ORAP. Conclusion: NORAP is the most important cause of RAP followed by worm infestation & sickle cell disease. Functional aetiology of RAP should be suspected in children with psychological problems belonging to upper class. GE/21(O) ACUTE DIARRHOEA IN CHILDREN: FIRST ACTION MANAGEMENT BY PERIURBAN MOTHERS. Ravinder K. Gupta, Ritu Gupta Child Care Centre, Nai Basti, Jammu Cant., J&K -180004 Objective: To study the first action management by periurban mothers in case of acute diarrhea in children. Design: Prospective descriptive study. Settings, Subjects and methods: This prospective study was conducted at a pediatric clinic from June 2004 to May 2005. About 2120 children having acute diarrhoea were enrolled for the study. The periurban mothers were interviewed with the help of pre-structured questionnaire. Detailed information was obtained regarding diarrhoeal episode, first action management by the mothers and nature of treatment given by private / government health agencies. Mothers were also asked about the knowledge of ORS, its preparation and administration. Health education was imparted. Results: Amongst 2120 children surveyed with acute diarrhoeal episode, majority (80%) were under five, with males having definite predominance (60%). About 65% children belonged to joint families. Fifty one percent of mothers had education above matric, while 38% were either graduates or post-graduates. Blood in the stools was associated in 7.3% cases. About 15.9% mothers adopted home available fluids and ORS as first action in acute diarrhoeal episode. Readymade ORS, sugar salt solution, ‘lassi’, or ‘shikanji’ were used by these mothers. Feeds including breastfeeds and fluids were stopped by 7.8% mothers. Household remedies such as rice gruel, dal water, curd, ajwain, jeera, sonf, onion juice, mashed banana / potatoes etc. were adopted as first action by about 8.6% mothers. Application of sacred thread (amulet) on upper arm, crushed leaves on anterior fontanel and certain superstitious beliefs like applying kajal and burning of chilies were adopted by some of these mothers. The private practitioners and quacks were consulted by 39.4% mothers while 20.4% children were taken to government health agencies or qualified pediatricians. About 7.6% mothers believed in self medication. In 1.2% cases no action was taken at all. Six hundred and seventy seven mothers who had adopted initial three above mentioned actions subsequently took their children to private practitioners / health agencies on 2nd day (22.4%) or 3rd day (47.6%).The correct preparation of sugar salt solution by using finger pinch, scoop or spoon were known to 15.4% mothers. About 20.7% mothers were properly using the readymade ORS. Conclusions: To conclude most of the periurban mothers still take unorthodox actions for the management of acute diarrhoea in children. ORS / home available fluids are inadequately used by these mothers and they do prefer private practitioners / quacks to qualified persons for the diarrhoeal management. The results emphasize the need for frequent demonstration and correct preparation and use of ORT for prevention and treatment of diarrhoea and restriction of the use of drugs. Community lectures, street plays, television spots and print media can play an effective role in eradicating deleterious misbeliefs and popularizing ORS in management of acute diarrhoea at home. GE/22(P) A STUDY ON CLINICAL AND BIOCHEMICAL PROFILE IN HEPATITIS A Amit Gupta, Monika Garg, Anjoo Bhatnagar, Vikas Goyal Escorts Hospital and Research Centre, Faridabad - 121002 Retrospective study in a tertiary care urban hospital. Period : 1-10-04 to 31- 08-05 Inclusion criteria : patients admitted to the department of Pediatrics with a confirmed serological diagnosis of hepatitis A. Exclusion : patients with associated infections, congenital syndromes or enzyme deficiency. 53 such subjects were enrolled in the study and their clinical and biochemical profile noted. The data thus collected was analysed . Results : 1.the cases were evenly distributed among all age groups.2.fever, vomiting, decreased appetite and pain abdomen were the most common symptoms in descending order. Fever in 46/51, vomiting in 42/51, jaundice in 40/51, decreased appetite in 37/51 & pain abdomen in 26/51.3.average duration of fever through the illness was upto with average of 4.s. bilirubin most commonly was between 3-10 mg% (35/51) & only 3/51 having direct fraction <50%.5.SGPT in these children ranged from 312 to 6041 with an average of 1945 against the usual of around 1000-1500 IU.6.SGOT was also significantly reaised to an average value of 1482 (range 124 to 4559) unlike studies showing an average about 700.7.in 11/38 (29%) cases SGOT was more than SGPT with 10 of them having a difference of more than 10%.8.there was an average drop of 1200 IU in SGPT after an average duration of 4.3 days.9.Albumin was maintained at >3 mg% except in 1 case who had ascites also. 10.on USGthe common findings were, gall bladder wall oedema (7/15) (47%); pericholecystic edema (6/15) (40%) ; minimal free fluid (6/15) (40%) & right sided pleural effusion (minimal) (4/15) (27%) were significant.11.none of the patients developed life threatening complications. Conclusions: •High elevation of SGOT & SGPT are expected in Hepatitis A.•Although in hepatitis A, rise in SGPT is often more than SGOT SGOT more than SGPT is seen often in conditions like alcoholic liver disease echoviral infections, but an elevation of SGOT> SGPT especially when in thousands should not be seen as away from hepatitis A.•clinical symptoms cannot be relied uponto assesss the severity of illness.•no role of vitamin K.•urine bile salts & pigments even in the presence of jaundice and is not reliable to screen for jaundice. GE/23(O) ACUTE HEPAITIS IN TYPHOID FEVER IN CHILDREN N K Biswas, Uma Raju, Kiran Sodhi,M Sharma, H Ravi Ramamurhty Command Hospital, Wanowrie Road , Pune Introduction: Typhoid fever is very common and is often associated with abnormal hepatic biochemical tests.However, severe hepatic involvement with clinical picture of acute hepatitis with fever, jaundice, right upper quadrant pain is uncommon and infrequently reported. Aim: To characterize the clinical picture, biochemical features, response to drugs and prognosis of typhoid fever associated with acute hepatitis in children. Material and Methods: 50 cases of typhoid fever( Age 0-12 years), proven by blood culture were studied with special referance to hepatic dysfunction. Liver function tests(LFT), Alkaline phosphatase(ALP), Aspargine transaminase(AST), Alanine transaminase(ALT),Prothrombin time(PT) & Prothrombin time with activated thromboplastin with kaolin(PTTK) were carried out in all cases. Results: Out of 50 cases, 3(6%) had hepatitis on admission. All had high fever( Range 101o F – 104o F), right hypochondriac pain, tender heptomegaly, direct hyperbilrubinemia(Range 2mg/dL – 7 mg/dL), elevated serum ALT(Range 98IU/L – 590 IU/L) and ALP(Range 230IU/L – 750 IU/L). Jaundice was noticed within 2 weeks of onset of fever (5 – 10 days). One patient showed mild derangement of PT. All the three cases were treated with Injection Ceftriaxone and showed complete clinical and biochemical recovery. Conclusions: Typhoid hepatitis is an uncommon but challenging problem and recognition of the entity is important to differentiate it from common ailments in the tropics such as viral, malarial or amoebic hepatitis. Early institution of specific therapy in cases of typhoid hepatitis carries a good prognosis GE/24(P) A CLINICO PATHALOGICAL PROFILE OF VIRAL HEPATITIS – A (VIRUS) IN CHILDREN AT BORDER DIST. OF HARYANA B. M. Jyani, Aruna Jyani Jyani Maternity & Children Hospital , Sirsa 125055 Hepatitis A virus still remains the commonest etiology of viral hepatitis. Various hematological and biochemical tests have been to prognosticate the disease, but all have their limitation. Different studies shown altered lipid profile hepatitis patients. As liver is the organ for lipid synthesis, in addition to the usual liver function tests, complete lipid profile of the patients was done. Aim and objectives: A clinicopathological study was undertaken to study the profile of all the serologically confirmed Hepatitis A Disease. A Period of study: Nine months-October, 2004 to June, 2005. Place of study: Jyani M.C. Hospital and Deptt. Of Pathology, Govt Medical College, Rohtak (Hry.) Materials and Methods: Twenty five patients were diagnosed over nine months. Detailed history was taken and clinical examination was done on admission. All the investigations were sent within 24 hours of admission. Results and analysis: The chief complaint was fever, the duration ranging from 2 to 7 days. All the patients except three notice jaundice before admission. Other complaints were anorexia, vomiting, pain abdomen and 9 had deep yellow (mustared oil like) urine and whitish stool. Liver was enlarged in all the cases and spleen was mildly enlarged. Three child developed hepatic encephalopathy 3 days after admission. Few of them had serum bilirubin 14.8 mg/dl on admission and Prothrombin time 49 sec. (Control 15 sec). On admission total bilirubin range was 1.7 to 19.6 mg/dl. Minimum SGPT was 130 IU/L Maximum was 1870 IU/L. The children who developed encephalopathy had SGPT 390 IU/L on admission. Prothrombin time could be done in 25 cases 5 were normal and rest 20 had double the control. In the lipid profile of the cases;-HDL, LDL and cholesterol was in the normal range in all the cases. VLDL was 2 to 10 times increased in 7 cased. Triglyceride was 2 times increased in 10 cases. The cases which went into Encephalopathy had low liver enzymes and lipid profile. Although all cases (except two) recovered clinically within 10-15 days biochemical parameters were normal by 20-22 days. Three cases expired at Govt. Medical College. The child with hepatic encephalophaty regained normal sensorium after four days and recovered after five days and discharged after 12 days. The biochemical parameters were altered throughout the course. The children left the hospital after 14 to 21 days and did reported for follow up and recovered well. Conclusion: Children with Hepatitis A infection usually have a short course of illness with good outcome. Along with the usual biochemical parameters, VLDL and triglyceride are markedly increased. The children with hepatic encephalopathy had low VLDL and triglyceride level. Good clinical judgement, meticulous history taking and well planned laboratory investigation and nice nursing care pays a lot in survival of high risk sever viral hepatitis cases in children.