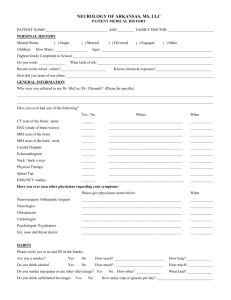
NEUROLOGY OF ARKANSAS
advertisement

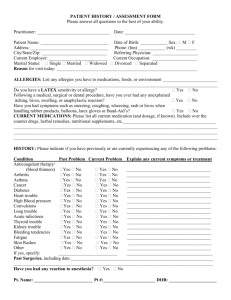
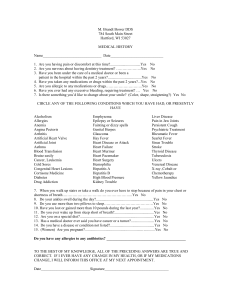
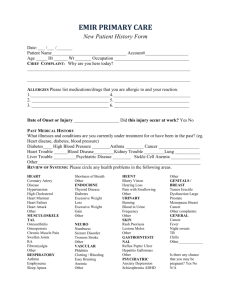
NEUROLOGY OF ARKANSAS PATIENT MEDICAL HISTORY PATIENT NAME:_________________________________ AGE:_________ FAMILY DOCTOR: ________________________ PERSONAL HISTORY Marital Status: Children: ( ) Single ( ) Married How Many: _________________ ( ) Divorced ( ) Engaged ( ) Other Ages: ___________________________________________________________ Highest Grade Completed in School: __________________________________________________________________________ Do you work: ______________ What kind of job: _____________________________________________________________ How did you learn of our clinic: ______________________________________________________________________________ GENERAL INFORMATION Why were you referred to see Dr. McCoy? (Please be specific) ________________________________________________________________________________________________________ Have you ever had any of the following? (check if yes) Where When CT scan of the brain / spine _______ _______________________________________ ____________ MRI scan of the brain / back/ neck _______ _______________________________________ ____________ Carotid Doppler / Echocardiogram _______ _______________________________________ ____________ Neck / back x-rays _______ _______________________________________ ____________ Physical Therapy _______ _______________________________________ ____________ Have you ever seen other physicians regarding your current symptoms: Please give physicians name below: When Neurologist _____________________________________________________ ____________ Chiropractor _____________________________________________________ ____________ Cardiologist _____________________________________________________ ____________ Psychologist, Psychiatrist _____________________________________________________ ____________ Ear, nose and throat doctor _____________________________________________________ ____________ HABITS Please circle yes or no and fill in the blanks: Are you a smoker? Yes No How much? __________________________ How long? _____________ Do you drink alcohol Yes No How much? __________________________ How much? _____________ Do you smoke marijuana? Yes No How often? _____________________________________________________ Do you use other illicit drugs? Yes No What kind? ___________________________ Do you drink caffeinated beverages Yes No How many cups or glasses per day? __________________________________ How often? _____________ ARE YOU ALLERGIC TO ANY MEDICATIONS? (if so please list) ________________________________________________ MEDICAL HISTORY Do you have or have you had any of the following? ____ Asthma ____ Diabetes ____ Hepatitis ____ Sleep Difficulty ____ Emphysema ____ Hypoglycemia (low blood sugar) ____ Seizures ____ Jaw/Joint Pain ____ Glaucoma ____ Back Trouble ____ Fainting/ Blacking out ____ Other (list)_ ____ Heart Disease ____ Neck Trouble ____ Arthritis ____________________ ____ Irregular Heart Beat ____ Thyroid Disease ____ Nervous Condition/ Anxiety ____________________ ____ High Blood Pressure ____ Liver Disease ____ Depression ____________________ ____ Stomach Ulcers ____ Renal (Kidney) Disease ____ Cancer ____________________ ____ Hiatal Hernia ____ Exposure to AIDS ____ Sinus Problems ____________________ ____ Cancer, if so what kind: __________________________________________________________________________________ ____ Autoimmune Disorders, such as Lupus, Rheumatoid Arthritis, etc. ________________________________________________ ____ Family History of: Stroke, Parkinson’s, Alzheimers, ALS (Lou Gherig’s disease), other nerve or muscle disorders resulting in full or partial paralysis. (circle all that apply) SURGICAL HISTORY Please list all surgeries with the most recent first: Type of operation Approximate date Hospital Surgeon ___________________________ _____________ ____________________ __________________________ ___________________________ _____________ ____________________ __________________________ ___________________________ _____________ ____________________ __________________________ ___________________________ _____________ ____________________ __________________________ Please list all medications (List prescription medications first, then any over-the-counter medications. Bring Meds or complete list) Medication Dosage How Often What for Prescribed by ________________________ ____________ ___________________ ___________________ _____________________ ________________________ ____________ ___________________ ___________________ _____________________ ________________________ ____________ ___________________ ___________________ _____________________ ________________________ ____________ ___________________ ___________________ _____________________ ________________________ ____________ ___________________ ___________________ _____________________ REVIEW OF SYSTEMS Constitutional: How many hours do you sleep at night? ____________________ Yes No Do you experience excessive daytime sleepiness? Yes No Change in appetite? Yes No Do you snore? Yes No Recent weight gain / loss in the last 6 months? Yes No Are you physically fatigued? Yes No Do you experience fever or chills? Yes No Chest palpitations? CV: Yes No Chest pain? Yes No Passing out spells? HEENT: Yes No Do you have frequent headaches? Yes No Trouble swallowing? Yes No Flashing lights. Dark spot in vision? Yes No Trouble with speech? Yes No Hallucinations? Yes No Double or loss of vision? Yes No Hearing loss? Yes No Dry eyes or dry mouth? Yes No Ringing / roaring in ears? Yes No Frequent mouth ulcerations? Yes No Dizziness? Yes No Neck pain or stiffness? RESP: Yes No Shortness of breath at rest or exertion? Yes No Chronic cough? Yes No Pain on inhalation? Yes No Cough up blood? Yea No Shortness of breath after lying flat? Yes No Awaken gasping for air? GI: Yes No Abdominal pain? Yes No Diarrhea or constipation? Yes No Nausea or vomiting? Yes No Blood with stool? Yes No Black blood bowel movements? GU: Yes No Urinary incontinence? Yes No Bowel incontinence? Yes No Burning or painful urination? Yes No Frequent urination? Yes No Blood in urine? Yes No Kidney stone? Yes No Abnormal sweating? ENDOCRINE: Yes No Sexual dysfunction? Yes No Light-headedness with standing? PSYCH: Yes No Depression? Yes No recent stress in life? Yes No Anxiety? Yes No Suicidal / Homicidal thoughts? NEUROLOGIC: Yes No Numbness or tingling in extremities? Yes No Confusion-spells? Yes No Extremity weakness? Yes No Seizures? Yes No Paralysis? Yes No Memory loss? Yes No Imbalance when walking? Yes No In-coordination of arms? Yes No Burning or stinging pain in extremities? Yes No Slurred speech? Yes No Involuntary movements? Yes No Tremors? Yes No Low back pain?