Signs - Dr. Roberta Dev Anand
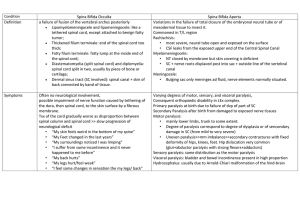
advertisement

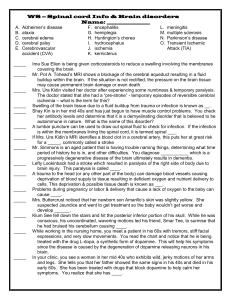
“I’ve wrestled with an alligator, I’ve tussled with a whale, I handcuffed lightning, threw thunder in jail. Last night I murdered a rock, injured a stone, hospitalized a brick. I’m so mean, I make medicine sick. I’m gonna show you how great I am.” -Muhammad Ali PART 2 CASE #5 SIGNALMENT: 4mth old, intact female Yorkshire Terrier; history of neck pain, Inability to stand/walk CASE #5: Atlantoaxial Instability Signs Toy and miniature breeds Reluctance to be patted on head Neck pain May have tetraparesis (weakness in all 4 limbs) or tetraplegia (paralysis in all 4 legs) Sudden death due to respiratory paralysis Atlantoaxial Joint Atlanto-Axial Joint Atlantoaxial instability Diagnosis Radiographs: lateral x-ray of neck in slight ventroflexion avoid further spinal cord damage with positioning Atlantoaxial Instability Normal toy breed dog Toy breed dog with atlantoaxial subluxation Narrowed spinal canal CT scan: dens is marked by * X-rays of same dogs; note separation of C1 and C2 when dog’s neck is flexed in B Atlantoaxial Instability (Subluxation) Treatment Medical splint neck in extension with cage confinement x 6 w treat like other spinal cord trauma Surgical (if unresponsive to medical Rx) stabilize/decompress attach dorsal process of axis to arch of atlas fuse atlas and axis joint with pins and bone graft hemilaminectomy to relieve spinal cord compression Atlantoaxial Instability: Surgical Correction Stabilization using trans-articular screws Stabilization using screws and bone cement Atlantoaxial Instability Client info prognosis is fair to good for animals with mild signs animals should not be used for breeding; may be hereditary CASE #6 Cervical Spondylomyelopathy: Wobbler’s Cervical spinal cord compression as a result of caudal vertebral malformation or misarticulation. Large breed dogs (Great Danes and Dobermans) Signs Progressive hind-limb ataxia (wobbly gait) Pelvic limbs cross each other when walking Abduct widely/tend to collapse May drag toes (wears dorsal surface of nails) Impaired proprioception Signs may also be present in front limb Crouching stance with downward flexed neck Rigid flexion of neck; may have neck pain Cervical Spondylomyelopathy: Wobbler Diagnosis Radiographs to show malalignment and narrowing of spinal canal Myelogram is essential to locate the region of compression CT and MRI if available Cervical Spondylomyelopathy: Wobbler Treatment: without treatment, prognosis is poor Medical Anti-inflammatory doses of corticosteroids Neck brace Cage confinement Surgical Decompression of spinal cord by laminectomy Stabilize vertebral column screws and wire dorsally spinal fusion ventrally Cervical Spondylomyelopathy: Wobbler Client info Prognosis is guarded Most likely a hereditary disease Multiple levels of compression less favorable prognosis than a single area of compression Surgery is risky and costly CASE #7 Degenerative Myelopathy Etiology: unclear May be autoimmune response to antigen in nervous sys Degeneration of white matter in ascending and descending tracts Signs Mainly in German Shep and Shep mixes (>5 yr) Progressive ataxia and paresis of hind limbs Loss of proprioception is first sign Dog “falls down” when trying to defecate Muscle wasting of back muscles along caudal thoracic and lumbosacral areas Symptoms progress until animal is unable to support weight on hind limbs Degenerative Myelopathy Degenerative Myelopathy Diagnosis Neurologic Exam ↓ proprioception N-↑ patellar reflexes Lack of pain Normal sphincter tone; normal panniculus (pin prick) reflex Radiographs usually normal Treatment: none - symptoms will progress to paralysis Degenerative Myelopathy Client info Degenerative myelopathy is a progressive, incurable disease Although symptoms are similar at early stages, it is a different disease from hip dysplasia When dog cannot support weight, quality of life should be evaluated Deafness damage to auditory pathway chronic otitis rupture of tympanic membrane damage to middle ear (ossicles) damage to auditory nerve hereditary or congenital bull terriers, Dobes, Rotts, Pointers, blue-eyed white cats, Dalmations, Aust Heelers, Aust shepherds, Eng setters, Catahoula related to drug therapy aminoglycosides (gentamicin, streptomycin, kanamycin topical polymyxin B Chloramphenicol Chlorhexidine w/ centrimide normal old age: usually due to atrophy of nerve ganglia or cochlear hair cells CASE #8 Deafness Diagnosis Inability to rouse sleeping animal with loud noise (e,g,. blast from air horn) is diagnostic Treatment: No treatment is available in most cases Hearing aids are available for animals, but most will not tolerate something in ear canal Client info Hearing loss is permanent If hereditary, do not breed Animals can be taught to hand signals rather than words Animals should not be off leash when outside Hearing aids are available for dogs but are usually not tolerated; would only be appropriate for hearing impaired Laryngeal Paralysis 3 types (always be cautious of laryngeal paralysis because of the chance of rabies) Hereditary: seen in Bouvier des Flandres and Siberian Huskies Acquired: can occur from lead poisoning, rabies, trauma, inflammation of vagus nerve Seen at 4-6 mo of age 1.5 to 13 yr of age Idiopathic: seen in middle-age to old large- and giant-breed dogs; castrated dogs and cats have a higher incidence than female and non-neutered males CASE #9 Laryngeal Paralysis Laryngeal Paralysis Signs: Inspiratory stridor Resp distress Loss of endurance Voice change Dyspnea/cyanosis/complete resp collapse Laryngeal Paralysis Diagnosis: laryngoscopy will show laryngeal abductor m. dysfunction Treatment: surgical intervention including: Arytenoidectomy Removal of vocal folds Client info: prognosis is guarded to good; do not breed if hereditary CASE #10 Coonhound Paralysis (Polyradiculoneuritis ) thought to be an immune response to an unknown etiologic factor in raccoon saliva some dogs will get it 1-2 wk after exposure, others exposed to same raccoon will not Signs: similar to tick paralysis and rabies Weakness begins in hind limbs with paralysis progressing rapidly to a flaccid tetraplegia Alert, afebrile animal Loss of spinal reflexes (patella tap, etc) Loss of voice; labored breathing; inability to lift head May die of respiratory failure May last for 2-3 mo (usually good Px) Rx: supportive nursing care Client info Dogs can be affected without exposure to raccoon May require long-term nursing care Some animals will regain total function, while more severely affected animals may not CASE #11 Tick Paralysis Cause: female tick (Dermacenter variablis, D. andersoni) → salivary neurotoxin Neurotoxin interfered with Ach at neuromuscular jct Not seen in cats; humans are affected Signs Gradual onset of voice changes and hind-limb ataxia (motor deficit) progressing to a flaccid, ascending paralysis (1-3 d) Sensation is intact Ticks on the dog Treatment Remove ticks (manually or with dip) Usually resolves in 1-3 d Supportive care until dog recovers Ventilation required for resp paralysis CASE #12 Idiopathic Facial Nerve Paralysis Etiology: unknown Occurrence Cocker Spaniels, Corgis, Boxers, Eng Setter, DLH cats Signs Older dogs (>5 y) Ear droop Lip paralysis Sialosis (drooling) Deviation of nose Collection of food in paralyzed side of mouth Absence of menace and palpebral reflex Idiopathic Facial Nerve Paralysis Treatment efficacy of corticosteroids unknown Artificial tears to prevent corneal ulcers Keep oral cavity clear of food Client info Cause is unknown Complete recovery does not usually occur May develop keratoconjunctivitis sicca (dry eye) Animals may require life-long maintenance Grey’s Anatomy Memory Center women women