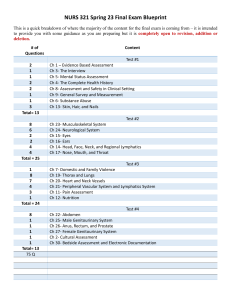
General endocrine patient form - St. John Providence Physician
advertisement
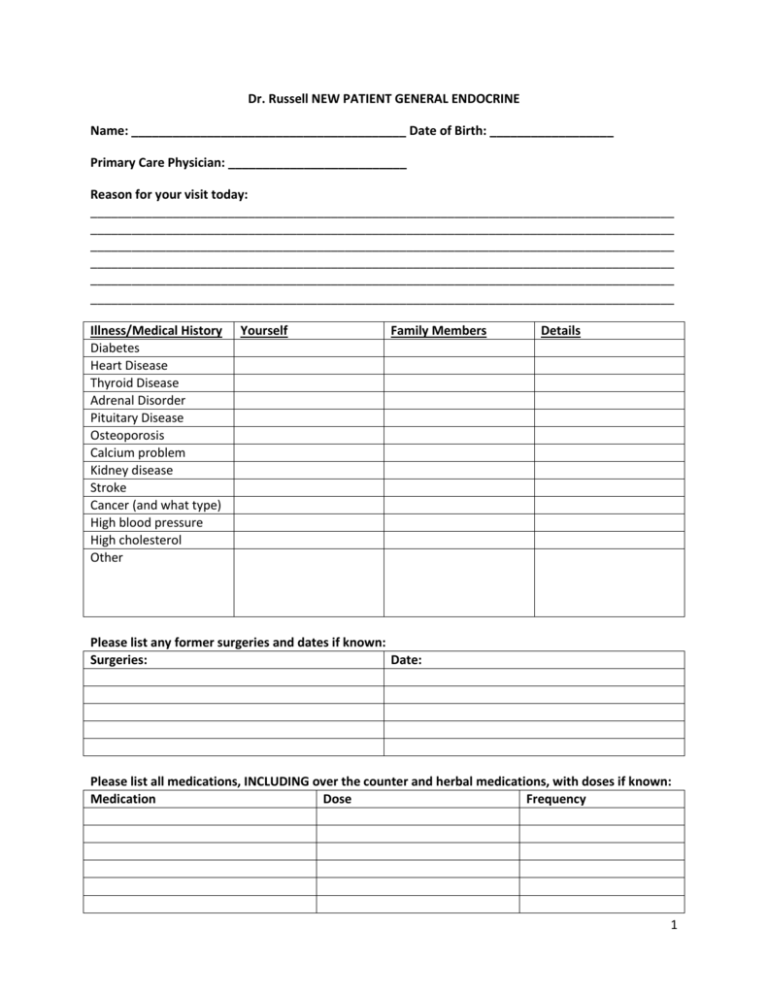
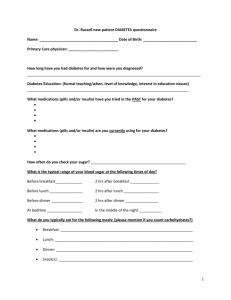
Dr. Russell NEW PATIENT GENERAL ENDOCRINE Name: ________________________________________ Date of Birth: __________________ Primary Care Physician: __________________________ Reason for your visit today: _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ Illness/Medical History Diabetes Heart Disease Thyroid Disease Adrenal Disorder Pituitary Disease Osteoporosis Calcium problem Kidney disease Stroke Cancer (and what type) High blood pressure High cholesterol Other Yourself Family Members Details Please list any former surgeries and dates if known: Surgeries: Date: Please list all medications, INCLUDING over the counter and herbal medications, with doses if known: Medication Dose Frequency 1 Are you allergic to any medications? If so, what reaction did you have? _________________________ Social History: Current smoker, if checked, how much and for how many years? _________________________ Smoked in the past, If checked, how much and for how many years? ______________________ Drink alcohol, If checked, how much and how often? ___________________________________ Marital Status: _________________________ Are you sexually active? Yes No For women only: Are you currently or in the near future interested in becoming pregnant? Yes No Review of systems: Please circle any CURRENT symptoms you are having on a FREQUENT basis General Head Neck Heart Lungs Gastrointestinal Urinary Reproductive Skin Blood Endocrine Musculoskeletal Neurological Psychological Fatigue, generalized weakness, weight loss, weight gain, abnormally thirsty Visual difficulty, double vision, blurred vision, change of voice, difficulty swallowing, painful swallowing Neck pain, neck swelling Fast heart rate, palpitations, chest pain, shortness of breath with exertion Shortness of breath, cough, difficulty breathing when lying down, difficulty with breathing when raising both arms above your head Abdominal pain, nausea, vomiting, diarrhea, constipation Frequent daytime urination, frequent nighttime urination, frequent urinary or vaginal infections For women: Last menstrual period _________, irregular periods, pregnant, post menopausal (including surgical menopause) For men: low libido, difficulty with erections, decreased shaving frequency Dry skin, moist skin, rash, easy/excessive bruising, thin skin, excessive acne For women only: male pattern hair growth Prolonged bleeding, other blood disorders Heat intolerance, cold intolerance Poor muscle strength, previous fracture, osteoporosis, previous foot ulcer, calf cramping Burning/numbness/tingling of feet, tremors, jitteriness Depression, anxiety 2 -------------------------------------------------------FOR STAFF USE ONLY------------------------------------------------------Physical Examination: Pulse Resting Rate Blood Pressure Height Weight BMI Eyes: pupils equal round and reactive to light, injection, proptosis, lid lag, stare, icterus HEENT: moist mucus membranes, no oral lesions, Lymphadenopathy: Palpable abnormal lymph nodes: ant/post cervical, supra/infra clavicular Neck: Thyromegaly _________, trachea deviated Heart: irregular rate _______, irregular rhythm, Chest: lungs clear to auscultation, negative Pemberton’s sign Abdomen: soft, nontender, good bowel sounds, Musculoskeletal: grossly intact muscle strength, no tenderness to palpation along spine/hips, intact distance between pelvic brim and lower ribs Extremities: no edema, palpable peripheral pulses, onychomycosis toenails Neurological: 2 + DTRs, intact monofilament/vibratory sensation, alert, oriented Skin: no ulcers on feet, dry skin, rash, jaundice Psych: normal mood/affect, normal judgment Other: ____________________________________________________________________________ Assessment/Plan: Return to Clinic ___________________ Physician Signature: _________________________________ 3