HEENT Exam: History, Techniques, and Findings
advertisement

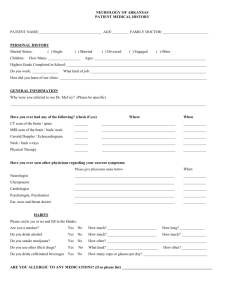
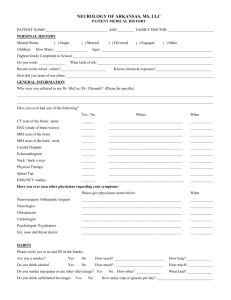
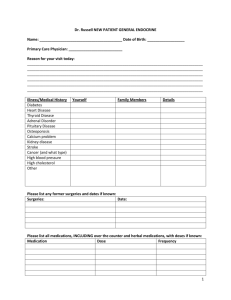
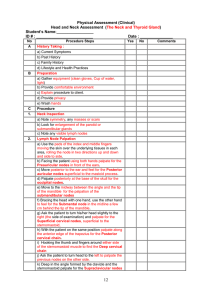
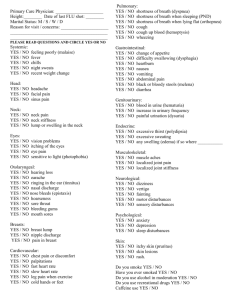
Chapters 10,11,12: HEENT 1. Conduct a history related to the head, neck, eyes, vision, ears, nose and throat 2. Discuss examination techniques for the head, neck, eyes, ears, nose and throat 3. Recognize findings that deviate from expected findings. 4. Relate symptoms or clinical findings to common pathologic conditions. Review of Related History: Head and Neck • Head injury. Relevant data include the nature of the accident, level of consciousness, predisposing factors, symptoms, and medications. • Headache. Patients with headaches should describe onset, duration, location, character, severity, and pattern of pain. Related symptoms and factors such as visual or sinus conditions and treatment attempts should be addressed. • Stiff neck. Pertinent data include signs of swelling, fever, characteristics of discomfort, causes, and treatment attempts. • Thyroid problem. Relevant data include temperature preference, neck swelling, texture of integument, emotional status, eye appearance, and menstrual and bowel patterns. Eyes • Eyelid drooping, difficulty with vision, loss of vision, floaters, eye pain, secretions, or medications used. Visual perception and related symptoms such as double vision should be investigated. ENT • Dizziness or vertigo. The onset, duration, description, and symptoms related to attacks should be listed. Ask patient to describe any related sensation, head movement, nausea, hearing symptoms, or unsteadiness. • Earache. Onset and duration should be explored, along with any signs of pain, fever, discharge, respiratory infection, swimming or trauma data, ear cleaning habits, and any associated symptoms, such as vertigo, and medications. • Hearing loss. Data relevant to hearing loss include gradual or slow onset, sound and speech perception, and type of assistance used, such as a hearing aid, a repeated history of cerumen impaction, and a history of ototoxic medication use. • Nasal discharge. The characteristics of discharge (e.g., amount and odor) and related symptoms (e.g., sneezing, itching, or tenderness) should be described. • Snoring. Pertinent data include snoring pattern and daytime sleepiness. • Nosebleed. Ask patient about frequency, treatment patterns, and predisposing factors (e.g., respiratory infection or tenderness over sinus). • Sinus pain. The following areas should be assessed for fever, malaise, cough, headache, maxillary toothache, eye pain; nasal congestion, colored nasal discharge; pain, including tenderness or pressure over sinuses (pain increases when bending forward); and medications (symptoms change with decongestant use). • Mouth lesions. Duration, pain, and factors prompting onset (e.g., stress, fatigue, or tobacco use) should be listed. Note variations in tongue character: swelling, size change, color, coating, ulceration, and difficulty moving the tongue. Note lesions any place else on the body (e.g., vagina, urethra, anus), and current medications including mouth rinses. • Sore throat. Ask patient to describe any pain from swallowing, associated symptoms (e.g., cough or hoarseness), and exposure to environmental irritants or infection. • Difficulty swallowing. Determine what types of food or drink pose a problem to swallowing. Identify what the patient feels at the time of difficulty. Ask whether patient has a problem with aspiration or with liquids coming out of the nose. Past Medical History Head and Neck • Occurrence of head conditions, previous head or neck pain, medical or surgical treatments, seizure activity, or thyroid conditions. Eye Past eye trauma, treatment and results; previous eye surgery and outcome; any chronic illnesses affecting vision and medications used ENT Related systemic diseases (e.g., diabetes, renal failure); childhood ear problems; strep throat infections: number and frequency; any incidence of nose, sinus, or throat problems; use of ototoxic and/or nasal medications Family History: Head and Neck Headaches or thyroid conditions Eye • Familial occurrence of retinoblastoma or cancer of retina, macular degeneration, color blindness, nearsightedness, or any other condition similar to patient’s eye condition ENT Hearing problems, Ménière disease, allergies, or hereditary renal disease Social History: Head and Neck Risks associated with employment, stress, environmental injuries, nutrition, alcohol, and medication ingestion, including the use of street drugs Eye Employment, activities, allergies, medications, contacts, and protective device use, exposure to irritants and activity risks. Routine care of eyes and eye devices should be explored ENT Exposure to hearing hazards and their use of protective devices. • Nutritional habits (especially sugar intake), oral care patterns, and use of tobacco, alcohol, cocaine Examination and Findings: *Items are required for each student to perform on the SP, other physical examination techniques/maneuvers can be done at your discretion Inspection: Head and Neck • Head and facial features: size, shape, symmetry, lesions, skull characteristics, characteristic facies* • Hair texture, color, and distribution • Salivary glands: size, symmetry* • Check for neck symmetry, fullness, masses and skinfolds; tracheal alignment* • Note jugular vein and carotid artery pulsation, location and prominence* • Evaluate motion range and strength of neck muscles* Eyes • Inspect eyebrow, eyelid, eyeball, conjunctiva, iris, pupil, lens, sclerae, and lacrimal apparatus: note swelling, redness, lesions, discharge etc* • Eye tests: visual acuity (Snellen and Rosenbaum testing)*, peripheral vision/confrontation test*, pupillary reaction- direct and consensual light response*, extraocular eye muscle test*, corneal light reflex, cover/uncover test Ophthalmoscope: inspect for red reflex; view cornea, lens, and retina; view optic disc, retinal vessels and surface, and macula/fovea centralis ENT • Inspect external auditory structures: note size, shape, symmetry, position, deformities or lesions* • Using otoscope, inspect auditory canal and tympanic membrane for color, contour and landmarks* • Inspect nose for color, size, structure, and position* • Use nasal speculum to view cavity, septum and middle meatus, and turbinate details; assess for nasal discharge* • Assess lips for symmetry, color, and surface characteristics* • Inspect teeth for occlusion and mucosa and gum characteristics. • Assess oral cavity and oropharynx using otoscope and tongue blade: note color, lesions, swelling, symmetry, presence/absence of tonsils* Palpation: Head and Neck • Feel facial bones and skull from front to back* Palpate salivary glands • Palpate arteries (temporal, carotids)* • Evaluate trachea position with thumb on each side at suprasternal notch. • Identify hyoid bone and thyroid/cricoid. • Palpate thyroid using anterior or posterior technique: note size, shape, consistency, tenderness, nodules* Eyes • Palpate eyelids • Palpate the eye ENT • Palpate auricles, mastoid area for tenderness, swelling and/or nodules* • Palpate nose ridge and soft tissues* • Occlude each nare for patency and smell* • Palpate sinuses for tenderness (transillumination: perform when sinus tenderness is present or infection is suspected)* • Palpate the gums, tongue, and floor of the mouth for abnormalities Ausculation: Head and Neck: • Listen for vascular abnormalities over temporal region when appropriate • Listen for vascular sounds, if thyroid is large Listen for carotid bruits IPC I: HEENT – TIME LINE 2:00 – 2:15 : Quiz 2:15 – 2:30 : Large classroom clinical pearls 2:30 – 3:10 : Open teaching in small group rooms Suggested Topics Quiz Review and/or Power point discussion Anatomy Review: Practice case – nothing fancy; can make up on the spot Briefly prep students for HEENT history taking and exam 3:10 – 3:25 : SP shows up at designated room; begin history taking See above for “Review of Related History” 3:25 – 4:25 : SP physical examination and Group activities Spend no more than 15 minutes demonstrating a physical exam Aim for 10 minutes per group of 2 students practicing the PE or 45 min for all 4. Don’t forget you can also practice PE findings in the activities rooms if you weren’t able to cover everything This leaves 5 minutes total to allot for movement between the small group rooms and SP room 4:25-4:30: closure session back in the small group room. Consider: recap of PE, continuing activities, and/or closing Q and A session. Instructions for Splitting up groups – Organized Chaos 1. Divide your 8 students into 2 groups, A and B 2. A stays in SP room after demonstration of PE by fourth year student a. All students need to perform the PE, but the 4th year has freedom on how they want to run this section. For example: i. One student at a time doing PE while other 3 students watch; teams of 2 students doing exam together, then switching with the other pair. ii. 4th year leader can give advice, positive feedback and constructive criticism, either after each student or after all four. 3. B starts in the small group room to participate in group activities. a. Case studies on activity sheet (HEENT worksheet) 4. After 30 minutes the groups switch a. A goes to B, and vice versa b. If no 4th year - Students in group B who are performing the activities on the worksheet should manage their own time and should remain in their small group room until group A arrives and sends them to SP room. 5. If everything occurs down to the minute the time should be 4:40 at the end of all stations. 6. Meet in small group rooms to review or answer questions until 5:00.