Should we stop ovarian crypreservation?
advertisement

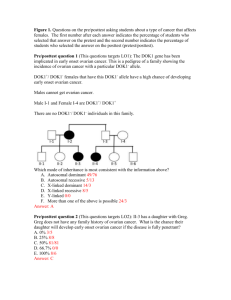
Ovarian Tissue Cryopreservation: Current Experience Ariel Revel MD. Joseph G Schenker MD,FRCOG,FACOG (Hon) Department of Obstetrics and Gynecology. Hebrew University Hadassah Medical Center P.O.Box 12000, Jerusalem, 91120, Israel. schenker@cc.huji.ac.il 1 Introduction Progress in cancer treatment improves survival and cure. The extensive advance in oncology, hematology and bone marrow transplantation (BMT) have resulted in a 90% remission rate in various diseases. Nevertheless, exposure of the ovaries to chemotherapy and radiotherapy during the reproductive years predisposes patients to ovarian failure. The remarkable improvement in the survival rates due to progress in cancer treatment has resulted in a large population of cancer survivors which require special medical treatment. The National Cancer Institute estimated that about 1 per 1000 population will be survivors of childhood cancers. Due to the limited possibilities of fertility preservation methods and the significant risk of ovarian failure, childhood cancer patients request special attention. This is especially important when taking the high 5 y survival rates in pediatric hemato-oncology patients (combined ~ 80 %, ALL 80-86%, Hodgkin’s disease>90%) (1-4) . A list of pediatric patients who face the risk of ovarian failure due to cytotoxic treatment is detailed in table 1. Whereas the cytotoxic-induced damage is reversible in other tissues of rapidly dividing cells such as bone marrow, gastrointestinal tract and thymus, it appears to be progressive and irreversible in the ovary, where the number of germ cells is limited, fixed since fetal life, and cannot be regenerated (3) (5) . Cyclophosphamide is the most commonly implicated agent in causing damage to oocytes and granulosa cells in a dose dependent manner (6) . Relative risk of POF was reported between 4 and 9.3 in patients receiving cyclophosphamide (7) 2 Radiotherapy is utilized to improve prognosis or to achieve local tumor control in solid tumors presenting in the pelvis such as Ewing sarcoma, osteosarcoma, retroperitoneal sarcomas, and in some benign bone tumors (8-11) . A common concern of female patients and their families is the effect of chemotherapy and radiotherapy on future fertility. An 8-fold increase in the risk of premature ovarian failure (POF) has been observed in cancer survivors (12) . Women who undergo bone marrow transplantation have a 99% risk for ovarian failure (13) . Whereas menopausal symptoms and signs can be treated medically, no solution is available to preserve female gametes. The resulting infertility and premature menopause produces physical, psychological, and social consequences. Options for Fertility Preservation Embryo cryopreservation: Women may be offered in vitro fertilization (IVF) for embryo cryopreservation prior to chemotherapy. This approach is the most successful one as pregnancy rates following embryo cryopreservation. Results are reasonable, although lower by one-third when compared with fresh IVF embryo transfer (14) and are standard in IVF units. IVF should be offered prior to chemotherapy and not afterwards, since diminished ovarian response was reported in women who underwent IVF after systemic cancer treatment (15) . Although women with significant systemic disease are reported to have poor ovarian response to ovulation induction (16) , most cancer patients can expect an average of 11 embryos cryopreserved (15) . Since a male partner is required for IVF, this option is inappropriate for single women who reject the use of donor sperm. In addition, ovarian stimulation requires deferment of chemotherapy and could be hazardous to estrogen-sensitive malignancies (e.g. breast carcinoma). A sufficient number of viable embryos cannot be guaranteed, and a repeat 3 IVF cycle may be contraindicated. Finally, ethical issues such as the fate of stored embryos, should the patient die, must be resolved at the outset of treatment. Oocyte Cryopreservation Oocyte cryopreservation would be an ideal technique for fertility preservation in single patients. Its advantages include no need for a partner, which avoids legal, regulatory and religious dilemmas. Nevertheless, this method has a very low success rate. Although attempted for more than a decade (17) , only a few pregnancies have been achieved from frozen–thawed human oocytes. While the introduction of new cryoprotective agents (18) and intra-cytoplasmic sperm injection (ICSI), as a means of bypassing the zona pellucida, has improved pregnancy rates of cryopreserved oocytes, pregnancies and deliveries derived from cryopreserved human oocytes have only resulted in a success rate averaging 2% per frozen oocyte (19) . The disappointing success rates can be attributed, in part, to the human oocytes biological properties (20) . Three major alternatives have been proposed in order to prevent chilling damage to oocytes: cryopreservation of immature oocytes, oocyte vitrification and ovarian cryo-preservation. Banking of germinal vesicle (GV) stage oocytes involves cryo-preservation at prophase I before oocytes resume nuclear maturation and progress to metaphase II. At this stage, a reduced risk of cytogenetic errors is theoretically expected since the chromosomes are not aligned along the spindle. Membranes of oocytes at the GV stage are, however, more sensitive to chilling injury (21) . Vitrification refers to a form of cryopreservation where cooling rates are so rapid (>20 000°/min) that ice does not have a chance to form, and the mixture of cryoprotectant and oocyte forms a ‘glass-like’ gel. From a practical standpoint, vitrification is simple and removes the need for expensive programmable controlledrate freezers. Following the first case report of pregnancy after oocyte vitrification 4 (22) , eight more pregnancies were reported (23, 24) . The need for high concentrations of cryoprotectants and the paucity of human clinical data require caution in the use of vitrification in clinical practice. A 2–4 month delay in cancer treatment would be required to obtain enough oocytes to enable a single pregnancy. This method cannot, at present, be routinely proposed to cancer patients. Ovarian Tissue Cryopreservation The emergence of ovarian tissue cryopreservation (OTCP) for fertility conservation has led to a new worldwide trend of ovarian tissue banking for reproductive cancer patients, scheduled to undergo chemotherapy or radiotherapy. Since the survival of young women and children who undergo such curative anticancer treatment is increasing, it is imperative for the consulting clinician to have an updated and accurate understanding of the proven benefits and the limitations of this new and hitherto evolving technique. OTCP was shown to be successful in several animal models during the last decades. In 1960, Parrot (25) reported successful pregnancies in mice after implantation of frozen-thawed ovarian grafts. Other studies reproduced the similar results in mice (26) and in sheep (27) . Despite these promising preliminary animal outcome, the efficiency of ovarian tissue auto-grafting whether orthotopic (the auto-transplantation to the ovarian pedicle) or heterotopic (the auto-transplantation to a different site) has not yet been demonstrated in humans. The initial hypothesis was that OTCP would be successful in humans, since the primordial and primary follicles can survive the freezing-thawing procedures. It was hoped that in vitro maturation (IVM) would be an important source for harvesting mature oocytes (28) . However, the in vitro maturation of both animal and human follicles was equally disappointing than auto-grafting. There still are no reports of harvesting mature oocytes from in vitro culturing and maturation of primordial and primary 5 follicles. Hence, there is increasing interest in improving the cryopreservation, autografting and the in vitro culturing and maturation techniques, necessitating further intensive research to increase their efficiency and to test their safety (29) . Ovarian Tissue Cryopreservation Clinical Application Human ovarian tissue banking is proposed as a method of preserving female fertility and offers the potential of restoring normal ovarian function and natural fertility. This procedure is applied in several medical centers worldwide. Indications for ovarian tissue cryobanking include pre-menarche girls as well as young women facing POF (30) . Cryopreservation of ovarian cortex rich in primordial and primary follicles is a strategy for oocyte banking. The rationale is to cryopreserve immature follicles within the ovarian tissue, before oocytes resume nuclear maturation. The main advantage of this technique is that no ovarian stimulation is required and thus the procedure can be performed on an urgent basis. Moreover, small immature follicles in the ovarian cortex probably withstand cryopreservation better than mature ones (31) . This has led to interest in the procedure as a potential strategy for preserving the fecundity of patients at risk of POF (32) . In order to obtain ovarian cortex, laparoscopic biopsies (33) or unilateral oophorectomy (34) can be carried out at any stage of the menstrual cycle. Women electing ovarian preservation at the time of abdominal surgery for other indications will incur no further risk from the operative procedure. In most cancer patients, laparoscopic oophorectomy does not incur a special surgical risk. Moreover, in many cases, this general anesthesia is used as an opportunity to perform a bone marrow aspiration or to insert a porthacath for the administration of chemotherapy. The technical method of ovarian cortex cryopreservation has been well described (35) . 6 Contraindications for ovarian cryopreservation include patients at high surgical risk and those >40 years old (36) . In order to prevent possible transmission of disease by ovarian grafts, we routinely send samples for pathological and immunohistochemical analysis. In patients with cancer involving the ovary, transplantation should not be performed since this may result in transferring malignant cells back to the patient (37, 38) . Xenotransplantation of human ovarian cortex transmitted cancer in Hodgkin’s disease and leukemia but not in non-Hodgkin’s lymphoma (39) . Frozen–thawed human ovarian tissue xenotransplanted into nude mice enabled follicular maturation and oocyte retrieval (40) . Human Ovarian Transplantation Techniques Ideally, frozen–thawed ovarian cortex should be used for obtaining oocytes by laboratory methods. In-vitro folliculogenesis entails harvesting mature oocytes in vitro from frozen–thawed ovarian cortex by isolating small follicles (41) or oocytes (42) from the surrounding stroma and growing them to maturity. Oocyte in-vitro maturation (IVM) is currently feasible only in the latest stages of follicular development and requires a lot of optimization before widespread clinical implementation. Freshly aspirated GV stage (prophase I) oocytes can be matured successfully in the laboratory to re-initiate and complete the first meiotic division to metaphase II, including accompanying cytoplasmic maturation and fertilization. This has resulted in the achievement of pregnancies and live births in polycystic ovary syndrome (PCOS) patients (43) . It should be remembered, however, that the capacity for oocyte maturation will be significantly lower when cryopreserved immature (GV stage) oocytes are used. With the advancement in IVM of primordial follicles (44) , one could envisage the possibility of safely obtaining oocytes from cryopreserved ovarian cortex. Oocytes competent for meiotic maturation, fertilization and 7 implantation could develop in vitro from primordial follicles. However, oocyte development in vitro beginning with the primordial follicles is a complex and prolonged process which includes follicular recruitment, tonic gonadotropin growth and gonadotropin-dependent stages. The first live offspring produced proved that development of oocytes in vitro from the primordial follicle stage is possible. A recent revised protocol presents a significant advance in oocyte culture technology (45) . Human Ovarian Transplantation Techniques Although human data do not substantiate fertility resumption after ovarian transplantation, animal data have demonstrated more success. Ovarian transplantation has been tested with various animal models (25, 27, 46-48) . Xenotransplantation of mouse ovarian cortex has enabled pregnancy (49) . The main obstacle to the wide application of ovarian cortex cryopreservation is that the majority of transplanted follicles are lost by ischemic damage by the time sufficient neoangiogenesis has supplied the graft. A significant fraction of the follicles are lost, however, during the ischemic phase present until neovascularization takes place (50, 51) . Ischemic damage is more pronounced in frozen–thawed than in fresh grafts (52) . However, the majority of ischemic damage observed in frozen–thawed avascular grafts occurs after transplantation, confirming that grafting procedures are more deleterious for follicle survival than cryopreservation (53) . Thus, optimal conditions have not yet been established and the success of ovarian tissue transplantation depends on the ability of the graft to support oocyte maturation and ovulation. It appears that ovarian slices can convey only short-term function due to loss of most follicles by ischemia. Ovarian transplantation preserving blood vessels could prevent ischemic follicular loss. Lessons from nature demonstrate the feasibility of intact ovary 8 freezing. One such example is the Canadian wood-frog (Rana sylvatica) which undergoes slow cooling and freezes for 6 months of winter (54) . Allografting vascularized rabbit ovaries with their oviducts by microsurgical techniques resulted in a vascular failure rate of only 5% of 40 grafts (55) . Intact ovarian freezing and transplantation preserving blood vessels has been reported recently in rats (56) and sheep (57, 58) . Until intact ovaries are successfully transplanted in humans, this technique should also be considered an experimental one. To our knowledge no pregnancy or embryo transfer was reported so far in humans as a result of utilizing cryopreserved ovarian tissue. At present the clinical experimental data showed the following results. Oktay reported two cases of a forearm heterotopic ovarian transplantation technique in two patients (59) . Both patients were menopausal immediately after oophorectomy. One patient developed a dominant follicle 10 weeks after transplantation, and her gonadotropin levels decreased to nonmenopausal levels. Percutaneous aspiration of ovarian follicles yielded a metaphase I (M-I) oocyte that was matured to metaphase II (M-II). The graft was functional for at least 21 months. In the second patient, ovarian follicle development was detected 6 months after transplantation, and periodic menstruation occurred thereafter. Spontaneous ovulation was confirmed by a midluteal increase in her progesterone levels. Menstruation and follicle development continued for more than 2 years after the transplant. The same group recently reported a case where ovarian tissue was cryopreserved for six year in a patient following chemotherapy and was transplanted beneath the skin of her abdomen. Ovarian function returned in the patient 3 months after transplantation, as shown by follicle development and estrogen production. The 9 patient underwent eight oocyte retrievals percutaneously and 20 oocytes were retrieved. Of the eight oocytes suitable for in-vitro fertilization, one fertilized normally and developed into a four-cell embryo (60) . Ethical Aspects The results of the attempts to achieve pregnancy by the use of ovarian tissue banking as a method to preserve fertility in cancer treated female patients confirm that this technique is still in its early stages. We believe that at this stage of experience and outcome, OTCP should not be routinely proposed to patients as a treatment modality. Cancer patients are a priori in a suboptimal health state and hence, the risk of invasive surgical procedures for retrieving ovarian tissue may not be justified. When applying this experimental approach women should be informed of the current state of data concerning the success rates in order to prevent developing false expectations and further disappointments. Furthermore, it should be taken into consideration that ovarian transplantation might be unsafe in some malignancies (e.g. acute leukemia) because of the risk of ovarian involvement and the possible reseeding of malignant cells through the implant On the other hand, other studies have shown that ovarian tissue harvested before high dose chemotherapy for lymphomas may not carry a risk of disease transmission by auto-transplantation (38, 39) . However, even in these low risk cases (e.g. lymphomas), transmission of the malignant cells is difficult to exclude completely. Thus, if auto-grafting is considered, testing for malignant cells in the tissue must be performed using adequate techniques. The current techniques are still unequivocal and inadequate and need further extensive research. 10 Studies on full organ cryopreservation (ovarian freezing and transplantation) are in their first phase of research and are thus not applicable at present. This modality may be a fertility conserving measure in the future. Since OTCP is yet to be yielding and in the absence of other more promising modalities, we believe that in order to preserve potential fertility in cancer patients, they should be advised with one of the following: Adult women with partners should be advised to undergo one cycle of ovarian super-ovulation with subsequent IVF before chemotherapy or irradiation in order to obtain embryos for cryopreservation. This strategy can be suggested to stable couples in order to achieve embryos with the partner’s sperm. Frozen zygotes have an acceptable rate of viability and are so far the only proven modality ensuring delayed pregnancy. To our experience one cycle of ovarian super-ovulation, is adequately safe and is equally acceptable by patients in most malignancies without significant deleterious influence of the delay in chemotherapy or radiotherapy on patient’s prognosis. In single adolescent women donor sperm can be used for oocyte fertilization and embryo cryopreservation. According to their desire and in the absence of any clinical contraindication to get pregnant due to their malignancy, those single women will have the option of embryo transfer. According to the present state of knowledge, embryos can be cryopreserved and achieve pregnancy for several years (61) and in some countries according to legislation or regulation even to ten years. Hence, women can decide whether they are interested in the sustained cryopreservation and transfer of these embryos. 11 In patients refusing to use donor sperm due to ethical, religious or traditional attitudes, oocyte harvesting and cryopreservation might be attempted despite low fertilization and pregnancy rates. This modality is still in its early experimental stages and only few cases of pregnancies were achieved. At the present time, oocyte cryopreservation is still more promising than OTCP in which no cases of pregnancies were reported. In pre-pubertal girls suffering from malignancies who are candidates for chemotherapy or radiotherapy, a different approach for fertility preservation is needed. In such girls, in whom ovulation induction can not be performed and mature oocytes can not be achieved, the above mentioned recommendation for embryo cryopreservation is impractical. The only option in this group is OTCP. If such a recommendation is given, these patients and their parent’s ought to be informed that this clinical approach is still in its early stages of experimentation and their chance to preserve fertility can not be guaranteed according to present knowledge. A detailed and up-to-date informed consent in such circumstances is crucial and mandatory. In conclusion, we believe that OTCP should be used in experimental set up and only when other modalities fail or cannot be implemented. Large scale human transplantation studies should be investigated in order to improve their efficacy and safety. Until then, OTCP should not be performed as routine therapeutic approach. This is of utmost importance in order to avoid creating false expectations and disappointments in these patients. 12 Table 1 Pediatric patients who face the risk of ovarian failure due to cytotoxic treatment • • • • • • • • 13 Leukemias Hodgkin’s lymphoma Neuroblastoma non- Hodgkin’s lymphoma Wilm’s tumor Ewing’s sarcoma Osteosarcoma of the pelvis genital Rhabdomyosarcoma. References 1) Brenner H, Kaatsch P, Burkhardt-Hammer T, Harms DO, Schrappe M and Michaelis J. Long-term survival of children with leukemia achieved by the end of the second millennium. Cancer 2001;92:1977-83. 2) Jemal A, Murray T, Samuels A, Ghafoor A, Ward E and Thun MJ. Cancer statistics, 2003. CA Cancer J Clin 2003;53:5-26. 3) Pui CH, Cheng C, Leung W, Rai SN, Rivera GK, Sandlund JT, et al. Extended follow-up of long-term survivors of childhood acute lymphoblastic leukemia. N Engl J Med 2003;349:640-9. 4) Robison LL and Bhatia S. Late-effects among survivors of leukaemia and lymphoma during childhood and adolescence. Br J Haematol 2003;122:345-59. 5) Gougeon A. Dynamics of follicular growth in the human: a model from preliminary results. Hum Reprod 1986;1:81-7. 6) Meirow D, Lewis H, Nugent D and Epstein M. Subclinical depletion of primordial follicular reserve in mice treated with cyclophosphamide: clinical importance and proposed accurate investigative tool. Hum Reprod 1999;14:1903-7. 7) Byrne J, Fears TR, Gail MH, Pee D, Connelly RR, Austin DF, et al. Early menopause in long-term survivors of cancer during adolescence. Am J Obstet Gynecol 1992;166:788-93. 8) Bacci G, Ferrari S, Mercuri M, Longhi A, Giacomini S, Forni C, et al. Multimodal therapy for the treatment of nonmetastatic Ewing sarcoma of pelvis. J Pediatr Hematol Oncol 2003;25:118-24. 9) Ozaki T, Flege S, Kevric M, Lindner N, Maas R, Delling G, et al. Osteosarcoma of the pelvis: experience of the Cooperative Osteosarcoma Study Group. J Clin Oncol 2003;21:334-41. 10) Pisters PW, Ballo MT, Fenstermacher MJ, Feig BW, Hunt KK, Raymond KA, et al. Phase I trial of preoperative concurrent doxorubicin and radiation therapy, surgical resection, and intraoperative electron-beam radiation therapy for patients with localized retroperitoneal sarcoma. J Clin Oncol 2003;21:3092-7. 11) Rodl RW, Hoffmann C, Gosheger G, Leidinger B, Jurgens H and Winkelmann W. Ewing's sarcoma of the pelvis: combined surgery and radiotherapy treatment. J Surg Oncol 2003;83:154-60. 12) Byrne J, Nicholson HS and Mulvihill JJ. Absence of birth defects in offspring of women treated with dactinomycin [letter; comment]. N Engl J Med 1992;326:137. 13) Mertens AC, Ramsay NK, Kouris S and Neglia JP. Patterns of gonadal dysfunction following bone marrow transplantation. Bone Marrow Transplant 1998;22:345-50. 14) ASRM/SART-registry. Assisted reproductive technology in the United States: 1999 results generated from the American Society for Reproductive Medicine/Society for Assisted Reproductive Technology Registry. Fertil Steril 2002;78:918-31. 15) Ginsburg ES, Yanushpolsky EH and Jackson KV. In vitro fertilization for cancer patients and survivors. Fertil Steril 2001;75:705-10. 14 16) Pal L, Leykin L, Schifren JL, Isaacson KB, Chang YC, Nikruil N, et al. Malignancy may adversely influence the quality and behaviour of oocytes. Hum Reprod 1998;13:1837-40. 17) Chen C. Pregnancy after human oocyte cryopreservation. Lancet 1986;1:884-6. 18) Boldt J, Cline D and McLaughlin D. Human oocyte cryopreservation as an adjunct to IVF-embryo transfer cycles. Hum Reprod 2003;18:1250-5. 19) Porcu E. Oocyte freezing. Semin Reprod Med 2001;19:221-30. 20) Fabbri R, Porcu E, Marsella T, Rocchetta G, Venturoli S and Flamigni C. Human oocyte cryopreservation: new perspectives regarding oocyte survival. Hum Reprod 2001;16:411-6. 21) Arav A, Zeron Y, Leslie SB, Behboodi E, Anderson GB and Crowe JH. Phase transition temperature and chilling sensitivity of bovine oocytes. Cryobiology 1996;33:589-99. 22) Kuleshova L, Gianaroli L, Magli C, Ferraretti A and Trounson A. Birth following vitrification of a small number of human oocytes: case report. Hum Reprod 1999;14:3077-9. 23) Yoon TK, Kim TJ, Park SE, Hong SW, Ko JJ, Chung HM, et al. Live births after vitrification of oocytes in a stimulated in vitro fertilization-embryo transfer program. Fertil Steril 2003;79:1323-6. 24) Katayama KP, Stehlik J, Kuwayama M, Kato O and Stehlik E. High survival rate of vitrified human oocytes results in clinical pregnancy. Fertil Steril 2003;80:223-4. 25) Parrot DM. The fertility of mice with orthotopic ovarian grafts derived from frozen tissue. J Reprod Fertil 1960;1:230 –41. 26) Carrol N and Gosden RG. Transplantation of frozen-thawed mouse primordial follicles. Hum. Reprod. 1993;8:1163-67. 27) Gosden RG, Baird DT, Wade JC and Webb R. Restoration of fertility to oophorectomized sheep by ovarian autografts stored at -196 degrees C. Hum Reprod 1994;9:597-603. 28) Hovatta O, Silye R, Krausz T, Abir R, Margara R, Trew G, et al. Cryopreservation of human ovarian tissue using dimethylsulphoxide and propanediolsucrose as cryoprotectants. Hum Reprod 1996;11:1268-72. 29) Picton HM, Kim SS and Gosden RG. Cryopreservation of gonadal tissue and cells. Br Med Bull 2000;56:603-15. 30) Donnez J, Godin PA, Qu J and Nisolle M. Gonadal cryopreservation in the young patient with gynaecological malignancy. Curr Opin Obstet Gynecol 2000;12:1-9. 31) Hovatta O, Silye R, Abir R, Krausz T and Winston RM. Extracellular matrix improves survival of both stored and fresh human primordial and primary ovarian follicles in long-term culture. Hum Reprod 1997;12:1032-6. 32) Newton H. The cryopreservation of ovarian tissue as a strategy for preserving the fertility of cancer patients. Hum Reprod Update 1998;4:237-47. 15 33) Meirow D, Fasouliotis SJ, Nugent D, Schenker JG, Gosden RG and Rutherford AJ. A laparoscopic technique for obtaining ovarian cortical biopsy specimens for fertility conservation in patients with cancer. Fertil Steril 1999;71:948-51. 34) Radford JA, Lieberman BA, Brison DR, Smith ARB, Russell SA, Watson AJ, et al. Orthotopic reimplantation of cryopreserved ovarian cortical strips after high-dose chemotherapy for Hodgkin's lymphoma. Lancet 2001;357:1172-1175. 35) Newton H, Fisher J, Arnold JR, Pegg DE, Faddy MJ and Gosden RG. Permeation of human ovarian tissue with cryoprotective agents in preparation for cryopreservation. Hum Reprod 1998;13:376-80. 36) Oktay K. Evidence for limiting ovarian tissue harvesting for the purpose of transplantation to women younger than 40 years of age. J Clin Endocrinol Metab 2002;87:1907-8. 37) Shaw JM, Bowles J, Koopman P, Wood EC and Trounson AO. Fresh and cryopreserved ovarian tissue samples from donors with lymphoma transmit the cancer to graft recipients. Hum Reprod 1996;11:1668-73. 38) Meirow D, Ben Yehuda D, Prus D, Poliack A, Schenker JG, Rachmilewitz EA, et al. Ovarian tissue banking in patients with Hodgkin's disease: is it safe? [editorial] [see comments]. Fertil Steril 1998;69:996-8. 39) Kim SS, Radford J, Harris M, Varley J, Rutherford AJ, Lieberman B, et al. Ovarian tissue harvested from lymphoma patients to preserve fertility may be safe for autotransplantation. Hum Reprod 2001;16:2056-60. 40) Revel A and Laufer N. Protecting female fertility from cancer therapy. Mol Cell Endocrinol 2002;187:83-91. 41) Smitz J and Cortvrindt R. Oocyte in-vitro maturation and follicle culture: current clinical achievements and future directions. Hum Reprod 1999;14 Suppl 1:145-61. 42) Abir R, Franks S, Mobberley MA, Moore PA, Margara RA and Winston RM. Mechanical isolation and in vitro growth of preantral and small antral human follicles. Fertil Steril 1997;68:682-8. 43) Cha KY and Chian RC. Maturation in vitro of immature human oocytes for clinical use. Hum Reprod Update 1998;4:103-20. 44) Vand Hur R, Abir R, Telfer EE and Bevers MM. Primate and bovine immature oocytes and follicles as sources of fertilizable oocytes. Hum Reprod Update 2000;6:457-74. 45) O'Brien MJ, Pendola JK and Eppig JJ. A revised protocol for in vitro development of mouse oocytes from primordial follicles dramatically improves their developmental competence. Biol Reprod 2003;68:1682-6. 46) Harp R, Leibach J, Black J, Keldahl C and Karow A. Cryopreservation of murine ovarian tissue. Cryobiology 1994;31:336-43. 47) Aubard Y, Newton H, Scheffer G and Gosden R. Conservation of the follicular population in irradiated rats by the cryopreservation and orthotopic autografting of ovarian tissue. Eur J Obstet Gynecol Reprod Biol 1998;79:83-7. 48) von Eye Corleta H, Corleta O, Capp E and Edelweiss MI. Subcutaneous autologous ovarian transplantation in Wistar rats maintains hormone secretion. Fertil Steril 1998;70:16-9. 16 49) Snow M, Cox SL, Jenkin G, Trounson A and Shaw J. Generation of live young from xenografted mouse ovaries. Science 2002;297:2227. 50) Newton H, Aubard Y, Rutherford A, Sharma V and Gosden R. Low temperature storage and grafting of human ovarian tissue. Hum Reprod 1996;11:1487-91. 51) Candy CJ, Wood MJ and Whittingham DG. Effect of cryoprotectants on the survival of follicles in frozen mouse ovaries. J Reprod Fertil 1997;110:11-9. 52) Nisolle M, Casanas-Roux F, Qu J, Motta P and Donnez J. Histologic and ultrastructural evaluation of fresh and frozen-thawed human ovarian xenografts in nude mice. Fertil Steril 2000;74:122-9. 53) Aubard Y, Piver P, Cogni Y, Fermeaux V, Poulin N and Driancourt MA. Orthotopic and heterotopic autografts of frozen-thawed ovarian cortex in sheep. Hum Reprod 1999;14:2149-54. 54) Storey KB and Storey JM. Freeze tolerance and intolerance as strategies of winter survival in terrestrially-hibernating amphibians. Comp Biochem Physiol A 1986;83:613-7. 55) Green CJ, Simpkin S, Grimaldi G and Johnson A. Pregnancy after autografting and allografting vascularized ovaries and en bloc vascularized ovaries with adnexa in rabbits. Br J Obstet Gynaecol 1982;89:645-51. 56) Wang X, Chen H, Yin H, Kim SS, Lin Tan S and Gosden RG. Fertility after intact ovary transplantation. Nature 2002;415:385. 57) Revel A, Elami A, Bor A, Yavin S, Natan Y and Arav A. Whole ovary cryopreservation and transplantation in sheep. Fertil Steril 2001;76:S42-43. 58) Jeremias E, Bedaiwy MA, Gurunluoglu R, Biscotti CV, Siemionow M and Falcone T. Heterotopic autotransplantation of the ovary with microvascular anastomosis: a novel surgical technique. Fertil Steril 2002;77:1278-82. 59) Oktay K, Buyuk E, Rosenwaks Z and Rucinski J. A technique for transplantation of ovarian cortical strips to the forearm. Fertil Steril 2003;80:193-8. 60) Oktay K, Buyuk E, Veeck L, Zaninovic N, Xu K, Takeuchi T, et al. Embryo development after heterotopic transplantation of cryopreserved ovarian tissue. Lancet 2004;363:837-40. 61) Revel A, Safran A, Laufer N, Lewin A, Reubinov BE and Simon A. Twin delivery following 12 years of human embryo cryopreservation: case report. Hum Reprod 2004;19:328-9. 17