Retina Anatomy
advertisement

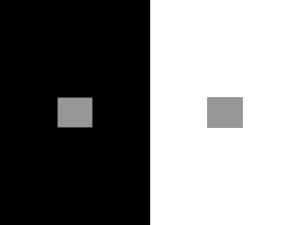
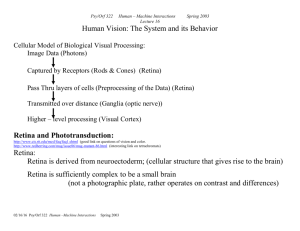
RETINA OUTLINE: PART 1 I. Overview A. Location 1. Circular disc of approximately 42mm diameter 2. A neural layer between the choroids and the vitreous 3. Extends from the circular edge of the optic disc to the ora serrata B. Structure 1. 7 cell types (see section II) 2. 10 layer (see section III) C. Morphological development 1. Neural retina develops from the neural tube ectoderm D. Local Specializations 1. Macula lutea- darkened region in the central retina (5.5mm dia.). (May appear to have a yellow hew because of the pigment xanthophylls). a) Fovea- shallow depression in the center of the macular region (1.5 mm dia.). The curved wall of the depression is known as the clivus. High concentration of cones and is capillary free. b) Foveola- contains the densest population of cones that have the smallest cross-sectional diameter of all the photoreceptors (0.35mm dia.). Red and Green sensitive cones only No rods or Blue cones c) Parafovea- contains the largest accumulation of retinal bipolar and ganglion cells (0.5mm dia.). d) Perifovea- area begins where the ganglion cell layer if four cells thick & ends where it is one cell thick (1.5mm dia.). 2. Ora Serrata- the peripheral termination of the retina. 3. Optic Nerve head - site where ganglion cell axons accumulate & exit the eye. Lacks all retinal elements except NFL and an internal limiting membrane ~ because it contains no photoreceptors, it does not elicit a response, and therefore represents the physiological blind spot. 4. Major blood vessels- The outer retinal layers receive their nutrition from the choroidal capillary bed, the inner layer from the central retinal artery (see section X). E. Photoreceptor distribution 1. Cone peak @ fovea (Cones dominate the central retina.) VS112 Ocular Anatomy UAB School of Optometry Page 1 of 10 2. Rod peak @ ~ 15 degrees temporal retina & 25degrees nasal retina. (No rods located at the center of fovea or optic disc. Rods dominate at the peripheral retina.) F. Central & Peripheral retina The periphery is designed for detecting gross form & motion, while the central area is specialized for visual acuity. The periphery makes up most of the retina, & rods dominate. Central retinal is dominated by cones, has the most ganglion cells per area, & a fairly small area portion of entire retina. G. Role The retina is the site of transformation of light energy into a neural signal & contains the first three types of cells (photoreceptor, bipolar, & ganglion) in the visual pathway, the route where visual information form the environment reaches the central nervous system for interpretation. II. Cell Types A. Vertical/Direct Pathway 1. Photoreceptors: the rods and cones are special sense cells containing photopigments that absorb photons of light. (Rods are more active in dim illumination; cones are more active in well lit conditions.) a) Outer segment—made up of a stack of membranous discs and is enclosed by the plasmalemma of the cell. Visual pigment molecules are located within the disc membranes. b) Connecting cilium—extends from the innermost disc, joining the outer segment with the inner segment. Acts as a conduit between them. c) Inner segment—composed of ellipsoids, closer to the outer segment and contains mitochondria; and myoid, closer to the cell body and is the site of protein synthesis. d) Nucleus—contained within the cell body e) Axon—an inner fiber containing microtubules running inward from the cell body. f) Synaptic terminal—ribbon synapses with bipolar and horizontal cells g) Phototransduction VS112 Ocular Anatomy UAB School of Optometry Page 2 of 10 2. RPE h) Structure of RPE—the outermost retinal layer, is a single cell thick and consists of pigmented hexagonal cells. Basal surface is next to choroids and apical surface faces neural retina. i) Choriocapillaries j) Bruch’s membrane—the basal aspect of the RPE contains numerous infoldings and is adherent to its basement membrane, which forms a part of Bruch’s membrane of the choroid. Therefore, its attachment to the choroid is strong. k) Apical processes—microvillus that extends into the layer of photoreceptors, enveloping the specialized outer segment tips. There are no intercellular junctions that connect RPE and photoreceptor layers. l) Adhering and occluding junctions—join the RPE cells near their apices. m) Photoreceptor renewal 2. Bipolar cells a) Named from shape b) Dendritic end—synapses with photoreceptor and horizontal cells. c) Nucleus—is large and contains little cell body cytoplasm d) Axon terminal end: dyad synapse—synapses with ganglion and amacrine cells. e) Cell body lies between the dendritic end and the axon terminal end. f) They relay information from photoreceptors to horizontal and ganglion cells and receive extensive synaptic feedback from amacrine cells. g) Several types of bipolar cells: (1) Rod (mop) bipolar cell: The only bipolar cell that contacts rods. (2) Midget bipolar cell: Flat midget bipolar cell or invaginating midget bipolar cell. (3) Diffuse cone bipolar cell: Type a (flat bipolars) and Type b (brush bipolars). These contact around 5 neighboring cones in central retina, and around 10-15 neighboring cones in the periphery. (4) Blue cone bipolar cell: These contact widely spaced rather than neighboring cones. (5) Giant cone bipolar cell: Two types-diffuse and bistratified. They differ in their axon terminations. 3. Ganglion cells VS112 Ocular Anatomy UAB School of Optometry Page 3 of 10 a) Can be bipolar (single dendrite) or multipolar. b) Dendrites—classified by branching pattern. These are either stratified, with horizontal branches arranged in one to three layers, or diffuse branching like a tree. c) Cell body d) Axons—each ganglion cell has a single axon e) Types of ganglion cells: (1) Midget ganglion cell (P1): Most common type. Has a single dendrite. Named because it projects to the parvocellular layer of the lateral geniculate body. (2) P2 ganglion cell: Also terminates in the parvocellular layer. (3) M-type ganglion cell: Projects to the magnocellular layer of the lateral geniculate body. B. Lateral Pathways 1. Horizontal cells a) Transfers information in a horizontal direction parallel to the retinal surface. b) Connections—synapse with photoreceptors, bipolar cells, and other horizontal cells 2. Amacrine cells a) Connections—forms complex synapses with axons of bipolar cells, dendrites, and soma of ganglion cells, with processes of interplexiform neurons, and with other amacrine processes. b) They play an important role in modulating the information that reaches the ganglion cells, owing to the extremely broad spread of its process. c) Numerous, distinguishable types (1) Cell size (2) Dendritic spread (3) Branching level (4) NTs/Nmodulators (5) Effects d.) Three main groups: small-field amacrines, medium-field amacrines, and large-field amacrines. III. Retina layers A. Retinal pigment epithelium (RPE) Outermost layer of the retina; lies between the outer segments of the photoreceptors and Bruch’s membrane of the choroid. arises from neural ectoderm VS112 Ocular Anatomy UAB School of Optometry Page 4 of 10 single layer of hexagonal cells, progresses from columnar to cuboidal from posterior pole to ora serrata, respectively melanosomes contain pigment liposfuscin granules contain degradation products of phagocytosis microvilli found on apical surface Gap junctions and tight junctions found at apicolateral cell surfaces B. Photoreceptor cells (rods and cones) Outer segment contains visual pigments in stack of membranous discs Inner segment contains the cellular organelles Projections from the apical surface of Muller cells separate the inner segments. RPE microvilli and outer segments of PRs interdigitate PRs surrounded by adhesive interphotoreceptor matrix that may help orient outer segments for optimum light capture 1. Rods more active in dim illumination discs are made in inner segment, displaced outward as more discs are made, sloughed off and phagocytosed by RPE cells 2. Cones usually cone-shaped with discs wider at base than at tip, though not always outer segment shorter than that of rod and may not reach RPE discs are often shed at end of day C. External limiting membrane consists of intercellular junctions b/w PR cells, and between PR cells and Müller cells at the level of PR inner segments; not a true membrane. tight junctions provide barrier to passage of large molecules looks like a fenestrated sheet under light microscopy D. Outer nuclear layer contains rod and cone cell bodies; Cone cell bodies and nucleus are larger than those of the rod. cone nuclei arranged in single layer close to ELM rod nuclei in several rows inner to cone nuclei E. Outer plexiform layer 1. External band - inner fibers of rods and cones 2. Inner band - synapses between PRs and cells of INL triads - two postsynaptic horizontal cell processes flanking bipolar dendrite at cone pedicle F. Inner nuclear layer Cell bodies of horizontal neurons, bipolar neurons, amacrine neurons, interplexiform neurons, Müller cells, and some ganglion cells Horizontal cell nuclei found next to OPL Amacrine cell nuclei found next to IPL VS112 Ocular Anatomy UAB School of Optometry Page 5 of 10 Bipolar cell dendrite in OPL, axon in IPL G. Inner plexiform layer Inner synaptic layer synaptic connections between axons of bipolar cells and dendrites of ganglion cells Contains the synapse between the first-order and second-order neuron in the visual pathway. midget bipolar cell axon, inner half of IPL, flat midget bipolar cell axon outer half ribbon synapses among bipolar axon, amacrine process, ganglion dendrite H. Ganglion cell layer usually a single cell thick except at macula (8-10 thick) and temporal side of optic disk (2 thick) number of ganglion cells diminishes toward ora serrata contains nuclei of ganglion cells and of some displaced amacrine cells I. Nerve fiber layer ganglion cell axons (run parallel to retinal surface) fibers proceed to optic disc, turn 90° and exit through lamina cribosa as optic nerve papillomacular bundle radiates to disc from the macular area, and carries the information that determines visual activity superficial capillary network Müller cell processes J. Internal limiting membrane Innermost boundary of the retina. terminations of Müller cells (footplates) covered by basement membrane form uneven outer surface of ILM vitreal fibers incorporated at periphery continuous with ILM of ciliary body at anterior present over the macula but undergoes modification at the optic disc, where processes from astrocytes replace those of the Muller cells VI. Sampling Unit = the smallest retinal region containing at least one representative from each type of ganglion cell. CELL TYPES: Photoreceptors—green, red, blue cones; rods for dark Bipolar cells—a class of retinal neurons that receive inputs from photoreceptors in the outer plexiform layer and have outputs to amacrine and ganglion cells in the inner plexiform layer (least 12 types) VS112 Ocular Anatomy UAB School of Optometry Page 6 of 10 Midget bipolar cells—type of bipolar cell that receives input from either red or green cones; in the central retina, the input is from a single cone Diffuse bipolar cells—receive input from several red and green cones ON bipolar cell—cone bipolar cell that depolarizes in response to increasing light intensity (ON) and terminates in the inner half of the inner plexiform layer OFF bipolar cell—cone bipolar cell that depolarizes in response to decreasing light intensity (OFF) and terminates in the outer half of the inner plexiform layer Midget ganglion cells—receives excitatory inputs from midget bipolar cells; in central retina, the input is from a single midget bipolar cell Parasol ganglion cells—a unistratified ganglion cell that receives excitatory inputs from diffuse bipolar cells Horizontal cells—a class of retinal interneurons that receive inputs from photoreceptors and have inhibitory outputs back onto photoreceptors. Blue cones are a major source of input onto H2 horizontal cells. Amacrine cells—a class of retinal interneurons that make connections in the inner plexiform layer among bipolar, ganglion and other ganglion cells (30 types) AII amacrine cells-- a small amacrine cell that receives inputs from rod bipolar cells and passes those signals to both ON & OFF cone bipolar cells. The sampling unit is defined in terms of information output, but its structural basis is determined by the ganglion cells. The ganglion cell type with the largest tiles and lowest density will have a larger sampling unit (i.e. in the periphery). The smallest sampling units are located at the fovea and are dominated by cone signals (Figure 15.35) from red and green cones. (pg 692) A parasol cell of the fovea contains about 35 midget ganglion cell dendritic fields, the highest ratio of midget to parasol cells in the retina. In typical sampling unit of this area, there will be 35 cones (22-25 red, 10 to 13 green). Each cone will synapse onto one ON and one OFF midget bipolar cell, for a total of 70 midget bipolar cells in a sampling unit. This level also contains approximately 18-24 diffuse bipolar cells. Each midget bipolar cell directly inputs onto a midget ganglion cells (therefore there are 70 midget ganglion cells). The diffuse bipolar cells integrate onto 2 parasol ganglion cells. X. Retinal Circulation A. The retina in vivo is thin and delicate. It cannot be seen if healthy. Only vascular system is visible. B. Components of retinal circulation 1. superior temporal vein 2. superior temporal artery 3. Nerve Head 4. Inferior Temporal vein 5. Inferior Temporal artery Fovea indicated because region is darker; vessels also arc around it. Anatomical evaluation of the fundus is concerned with the uniformity of the background, the characteristics of the vessels, and appearance of optic nerve head. C. Central Retinal Artery-end arterial system VS112 Ocular Anatomy UAB School of Optometry Page 7 of 10 1. no connection with any other arterial system 2. no anastosomes between major and minor branches 3. obstruction of any branch, large or small, will deprive the inner retina of blood supply. D. Arterial and Venous branches extend radially into the retina 1. interconnected by capillaries 2. each capillary bed is supply by one venule 3. deepest capillaries extend farthest into the fovea 4. most superficial capillaries enter fovea last The foveal center lacks capillaries. The foveal cones are adequately supplied by the choriocapillaries behind them. Capillaries do appear along the foveal slope. Retinal capillaries are specialized to create a blood-retinal barrier. This is accomplished by the presence of overlapping endothelial cells and tight junctions. Optic Nerve and Nerve Head All ganglion cell axons and all branches of the central retinal artery and vein converge at the optic nerve head -Nerve head is slightly elliptical, elongated vertically -Typically there are 4 arterial and 4 venous branches from the nerve head, creating 2 superior and 2 inferior branches of both the central retinal artery and central retinal vein The optic disc, or optic nerve head, is the site where ganglion cell axons accumulate and exit the eye The nerve head and optic nerve consist primarily of axon bundles separated by sheaths of glial cells and connective tissue -Nerve head can be divided into 3 different parts: 1) laminar portion, 2) prelaminar portion, 3) postlaminar portion Laminar portion- defined by scleral fibers that intersect the axons as they exit the eye at the lamina cribosa Prelaminar portion- the nerve head proper, lying between the lamina cribosa and the vitreous Postlaminar portion- the 1st millimeter or so of the optic nerve just behind the eye -Meniscus of Kuhnt- at the center of the nerve head and is the thickest part of the internal limiting membrane of Elschnig; looks like a cup or depression in the optic disc Ganglion cell axons form a stereotyped pattern as they cross the retina to the optic nerve head -Axons from ganglion cells at retinal locations nasal, superior, and inferior to the optic nerve head follow direct, almost straight-line paths to the nerve. Ganglion cells on the nasal side of the fovea also have axons running directly to the nerve, as the papillomacular bundle. Axons from all other ganglion cells follow paths around the fovea. Temporal to fovea, VS112 Ocular Anatomy UAB School of Optometry Page 8 of 10 the horizontal raphe divides the ganglion cells whose axons run below the fovea from those whose axons run above it Axons from many widely separated ganglion cells are collected in bundles in the nerve fiber layer Axon bundles have an orderly arrangement in the nerve head -Nerve head has been divided into sectors and annuli -The organization of axon bundles in the nerve head is chronotopic ordering which depends on the timing of axon outgrowth during development -blind spot- the counter part of the nerve head. It is temporal to the fovea The lamina cribosa is weaker than the rest of the sclera Behind the lamina cribosa, the optic nerve has two sources of blood supply: 1) central artery branches 2) plexus derived from short posterior ciliary nerves Two theories in origin of field defects in glaucoma 1) vascular defects at the optic nerve head or 2) structural changes in the lamina cribosa Field defects in glaucoma may be due to blockage of axonal transport secondary to deformation of the lamina cribosa -There is progressive deepening of the cup in the nerve head from normal to advanced glaucoma. As the cup deepens and the lamina cribosa becomes more curved, axons passing through are subject to kinking and pressure as they make their way through the lamina cribosa. Pathology 1. Age Related Macular Degeneration (ARMD) - #1 cause of vision loss in the US. Occurs in two forms, wet and dry. Dry is more common than the wet form. ARMD is scarring of macula which distorts or obscures part of the central image that they eye transmits to the brain. Drusen (tiny yellow deposits) build up in Bruch’s membrane signaling degeneration and thinning of nerve tissue. 2. Glaucoma- a group of eye diseases in which a specific pattern of damage to the optic nerve results in loss of eyesight. Three of the most common types are open angle, closed angle, and congenital glaucoma. In most cases, damage to the nerve is thought to be a consequence of increased pressure in the eye. However, damage often occurs without increased IOP. Glaucoma is better thought of as a neurodegenerative disease caused by damage to and loss of nerve cells rather than just a disease of high IOP. 3. Retinitis Pigmentosa-a primary degeneration of the neuroepithelium of the retina, its pigment, and its blood vessels. Main symptoms are night blindness with progressive loss of the visual field (peripheral vision lost first, with central vision lost in the final stages of the disease). Its cause is unknown. 4. Diabetic Retinopathy-eye disease caused by diabetes resulting in damage to small blood vessels in the retina leading to vision loss. Two stages: 1) nonproliferative retinopathy 2) proliferative retinopathy. Nonproliferative is characterized by microaneurysms that develop in small vessels which burst and leak into the retina and vitreous. Proliferative retinopathy’s main feature is the growth of fragile new blood vessels on the surface of the retina. These abnormal blood vessels may break easily, bleeding into the middle of the eye and clouding VS112 Ocular Anatomy UAB School of Optometry Page 9 of 10 vision. They also form scar tissue that can pull on the retina, leading to retinal detachment. 5. Retinal Detachment-occurs when the retina becomes separated (detached) from the RPE and the wall of the eye. Fluid from the eye flows into the space between the two layers, further separating them. Injury to the eye, a blow to the head, eye disease, and conditions such as diabetes can lead to retinal detachment at any age. The direct causes of retinal detachment are: tears or holes in the retina, traction on the retina, and fluid buildup in the potential space under the retina. VS112 Ocular Anatomy UAB School of Optometry Page 10 of 10