Neuroscience 11a – Structure and Function of the Eye
advertisement

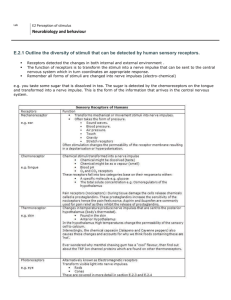
Neuroscience 11a - Structure and Function of the Eye Anil Chopra 1. Draw the main components of the eye, including its focussing apparatus, and describe their principal function(s) 2. Describe the production, circulation and drainage of aqueous humour and explain the importance of its contribution to the maintenance of intraocular pressure 3. Explain how raised intraocular pressure can lead to glaucoma 4. Draw the main layers, cellular components and synaptic connections of the retina, and describe the significance of the macula and fovea, especially in relation to visual acuity 5. Explain the basis of phototransduction, and distinguish the different contributions of rods and cones to the visual process. 6. Explain briefly the most common forms of colour blindness 7. Describe the basis of physiological optics and of the common defects of refraction 8. Draw the binocular visual pathways, from retina to lateral geniculate nucleus to primary visual (striate) cortex, with special regard to the partial decussation at the optic chiasm and its consequences for the visual field representation at higher levels of the pathway. 9. Explain how specific visual field defects can arise from lesions at different sites, including the optic nerve, chiasm and radiation, and at different locations within striate cortex. Give examples of how some of these defects may arise. 10. Outline briefly the basic processes of visual integration occurring at different levels of the visual pathway, and how these relate to interpretation of the retinal image. 11. Explain briefly the concept of functional specialization and the clinical effects of focal extrastriate lesions, especially in relation to the visual perception of colour and motion. 12. Describe the afferent and efferent pathways underlying the pupillary light reflexes (direct and consensual) and the near reflex. 13. Outline briefly the circadian visual system and indicate its significance 14. Explain briefly the simple assessment of visual field 15. List the most common uses of the ophthalmoscope 16. Outline the simple tests for visual acuity and colour blindness 17. Outline the tests for papillary responses 18. Understand the optics of the human eye 19. Know what errors of refraction are common in humans 20. Understand why spectacles do not correct all types of vision loss 21. Understand the optics underlying spectacle correction of vision 22. Know which eye problems are the commonest causes of vision loss 23. Know specifically which parts of the eye are affected by these conditions 24. Learn how to predict the specific nature of vision loss in individual conditions through knowledge of eye anatomy and physiology Purposes of Vision Scene selection (head and eye movement) Light intensity (retina and pupil) Colour (cones) Night vision (rods) Process images (post receptoral pathway) The eye Cornea: principal refraction of light occurs here. It refracts light by 60dioptres. Lens: secondary refraction of light occurs here. Its power varies with age – average is 6 dioptres in adults = accommodation. Anterior Chamber: this is the region between the cornea and the iris. It also provides the flow of the aqueous humour from the ciliary body in the posterior chamber (where it is secreted) round the iris and into the anterior chamber.. It is drained through the trabecular meshwork. This provides the transparency for the lens, nutrient for the cells and maintains intra-ocular pressure. (in glaucoma a tumour in the ciliary body produces too much aqueous humour and intra-ocular pressure increases causing damage to the optic nerve). NB: aqueous humour is plasma like and replaced every 100 mins. Iris: contains circular and radial muscles to allow more or less light to reach the retina. Retina Retinal Function The retina contains photosensitive cells situated at the posterior of the eye with the neurones being anterior. Both photosensitive cells contain outer segments with a pigmented retinal layers, an inner segment containing the nucleus and organelles and a synaptic terminal at their most anterior. As can be seen the photoreceptor cells are attached to the retina itself – therefore the light has to pass through the ganglion cell layer, the bipolar cell layer and through the photoreceptor layer itself before it reaches the light sensitive tips Outgoing nerve impulses then travel back through the cell layers to the ganglion cell layer where the optic nerve is formed at the optic disc which also forms the blind spot (no photoreceptor cells present) Macula = a yellow spot/small depression formed by the outward displacement of vessels and cells. At the centre of the macula is a fovea – a tiny rod free area with the highest concentration of cones. The ratio of ganglion cells to cones is also higher in the fovea – almost 1:1 relationship (improves acuity – the ability to resolve objects close together). The further from the fovea, the reduced numbers of cones and increased numbers of rods. The fovea is the principal focal point. The fovea is also avascular. There are 2 main types of photosensitive cell: Rods Scotopic – can work in low light Monochromatic – non-colour. High sensitivity Low Visual acuity Head is cylindrical in shape and hence arranged in many layers. If one disc does not pick up a photon then the next one in the chain may. Not in fovea, generally in peripheral retina. More pigment than cones. 20 times more rods than cones Cones Photopic – bright light Colour Vision 3 Types with different sensitivity ranges o L – cone – 560nm (red) o M – cone – 530nm (green) o S – cone – 420nm (blue) Low Sensitivity High visual acuity Head is conical which makes it sensitive to light rays along its axis Concentrated in the fovea (macula) – centre of eye Less pigment than rods 20 times fewer cones than rods. Diseases caused: o Protanopia:(protanomally): missing (abnormal) L cone o Deuteranopia :missing (abnormal) M cone o Tritanopia : missing (abnormal) S cone Visual Transduction 1. Light enters the eye through pupil and travels through neurone layers. 2. It hits the visual pigment known as 11-cisretinal. 11-cis-retinal is bound to a photopsin. There are different opsins in the different cells: Opsin – rods (producing Rhodopsin) Erythrolabe – L cones Chlorolabe – M cones Cyanolable – S cones 3. The 11-cis-retinal absorbs a photon of light and is isomerised to all-trans retinal. 4. All-trans-retinal is unable to bind to the opsin and so a G-protein signalling pathway causing a decrease in intracellular cGMP. 5. This results in cGMP gated channels closing and hence the cell becoming hyperpolarised. Normally, in darkness, the cells are depolarised and the Na+ channels are open, maintaining the membrane potential at -40mV. 6. The hyperpolarisation INHIBITS the release of glutamate (neurotransmitter) at the synapse. 7. The inhibition of glutamate can result in one of two reactions in bipolar cells depending on the type: a. In an ON bipolar cell, the reduction of glutamate release causes the cell to depolarise. The depolarisation will then result in the release of neurotransmitter onto a ganglion cell. b. In an OFF bipolar cell, the reduction of glutamate release causes the cell to hyperpolarise. The hyperpolarisation stops the release of neurotransmitter onto the ganglion cell. 8. Signals are then projected onto the brainstem and thalamus. Visual Processing It is initiated in the outer-plexiform layer of the retina Bipolar cells receive direct input at the receptive field centre together with surround input via horizontal cells Centre-surround opponency provides the first spatial processing of visual information. Surround receptive fields result from horizontal and amacrine cells Ganglion Cells: each ganglion cell has a receptive field with a certain number of bipolar and photoreceptor cells. There are 2 types of ganglion cell: “ON Centre” (off surround) o If light is shined only on the centre, the photoreceptor cells stimulate ON bipolar cells the ganglion cell fires more frequently. o If light is shined only on the outer part, the photoreceptor cells stimulate OFF bipolar cells (or horizontal cells) the ganglion cell fires less frequently. “OFF Centre” (on surround) o If light is shined only on the centre, the photoreceptor cells stimulate OFF bipolar cells the ganglion cell fires less frequently. o If light is shined only on the outer part, the photoreceptor cells stimulate ON bipolar cells (or horizontal cells) the ganglion cell fires more frequently. Furthermore, ganglion cells are further divided into: Parvocellular: these have small receptive fields and respond to colour Magocellular: these have large receptive fields and respond to movement and contrast. Bipolar cells receive direct photoreceptor input at the receptive field centre together with surround input fed via horizontal cells. Horizontal Cells also feed into bipolar cells that may not be directly connected to all the photoreceptor cells to create the “centre-surround” organisation of the receptive field bipolar cells. Horizontal cells are also responsible for shifting the spectral sensitivity on the bipolar cell to match illumination. Amarcrine Cells also feed into ganglion cells that may not be directly connected to all the bipolar cells. Electroretinography, is used to measure the electrical responses of various cell types in the retina. Electrodes are placed on the cornea and the skin near the eye. During a recording, the patient is watching a standardized stimulus and the resulting signal is interpreted in terms of its amplitude (voltage) and time course. Stimuli include flashes (flash ERG) and reversing checkerboard patterns (pattern ERG). Colour opponent primate ganglion cells Basic Currency of Parvocellular Pathway Colour perception is created by colour opponency of different cones which are receptive to different wave lengths of light: + - - + R on / G off + R off / G on B on / Y off + - - + G = M cone G on / R off G off / R on B = S cone R = L cone Y=L+M Visual Pathways Axons of the ganglion cell neurones travel posteriorly through the head to the optic chiasm via the optic nerve (II) From here, the neurones from the temporal retina pass on to the ipsilateral lateral geniculate nucleus, and those from the nasal retina pass on to the contralateral lateral geniculate nucleus. From here they project onto the primary visual cortex. In the lateral geniculate nucleus (in the cortex), clear sub-divisions can be seen between left and right eye as well as with differing cell types. the eye on the same side (the ipsilateral eye w.r.t the left or right LGN) sends information to layers 2, 3 and 5 the eye on the opposite side (the contralateral eye w.r.t the left or right LGN) sends information to layers 1, 4 and 6. A simple mnemonic for remembering this is "See I? I see, I see,". (CIICIC) The cells from the lateral geniculate nucleus project onto simple cells. These cells are designed to sense for edges of objects. Different aspects of visual information are carried in parallel pathways and are processed simultaneously by the brain. V1 is the primary visual cortex. It receives the input from the lateral geniculate nucleus. V1 has a very well-defined map of the spatial information in vision. For example, in humans the upper bank of the calcarine sulcus responds strongly to the lower half of visual field (below the center), and the lower bank of the calcarine to the upper half of visual field. Conceptually, this retinotopy mapping is a transformation of the visual image from retina to V1. The correspondence between a given location in V1 and in the subjective visual field is very precise: even the blind spots are mapped into V1. The visual information relayed to V1 is not coded in terms of spatial (or optical) imagery, but rather as the local contrast.