ES State Processes - Texas Health and Human Services Commission
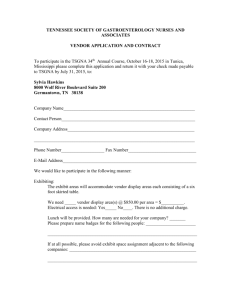
advertisement

ES State Processes December 2013 Eligibility Services State Processes Effective December 2013 ES State Processes I. II. III. IV. December 2013 Introduction Access Channels General Expectations HHSC Eligibility Office Application Registration and Scheduling Tasks Applications/Redeterminations - Received by HHSC Eligibility Office Application/Redetermination – Interview Required or Requested Application/Redetermination – Interview Not Required or Requested Scheduled Interviews Missed Appointments Reschedules Desk Review Children’s Health Insurance Applications/Redeterminations V. Customer Care Center Agency Generated Changes Date Of Death (DOD) Alert Processing Enrollment Broker Expection Task Changes Reported via OIG Failure to Return Review Packet (091 Denials) System Denial Task SNAP Terminated Task Duplicate Applications Client Reported Changes Changes Reported via OIG Returned Undeliverable Mail VI. Texas Women’s Health Program Texas Women’s Health Program (TWHP) - Applications Texas Women’s Health Program (TWHP) – Redeterminations Pregnant Women Medicaid Applications VII. Centralized Benefit Services MTFCY Application/Redetermination Processing FFCC Application Processing MTFCY/FFCC Exception Task HC-FFCHE Request for Review Task SNAP – SSI Application/Redetermination Processing Simplified Nutritional Assistance Program (SNAP - CAP) Processing Medicaid for Breast and Cervical Cancer Processing RMA Processing TYC/TJPC Applications Medicaid for Inmates of a Public Institution Applications CBS Disposition Tasks VIII. Medicaid for the Elderly and People with Disabilities MEPD Applications MEPD Interview Requested MEPD Redeterminations Reschedules LIS MSP Application Processing Medicaid Buy-In (MBI) Medicaid Buy-In for Children Processing MEPD Referrals 2 5 6 8 9 9 10 10 11 11 11 12 13 15 16 16 16 18 18 19 19 19 19 19 20 20 22 22 22 22 23 23 23 23 24 24 24 24 25 26 26 26 29 29 29 29 30 30 30 30 31 ES State Processes MEPD Regional Change Processing Date Of Death (DOD) Alert Processing MEPD Disposition Tasks Failure to Return Review Packet Duplicate Applications Additional Processes IX. Outstationed/Facility Workers MEPD Processing MEPD Facility Requests Texas Works Processing X. Central Processing Center CHIP Perinatal Form H3038P Process XI. Centralized Representation Unit Fair Hearings Processing XII. CHIP Request for Review (RFR) Request for Review Processing Request for Continued Enrollment Processing XIII. Data Integrity Change for a MEPD-SSI Case TLM task Freeze Flag Alerts ME SSI Manual Certifications Medicare Buy In QI-1 Managed Care Newborn Eligibility Merge & Separate Biographical Corrections XIV. ES CBO Regional Office ‘Assisted’ Applications/Redetermination Processing ‘Interviewed’ Application/Redetermination Processing CBO Documents Submission ES CBO Contacts XV. General Processing Duplicate Applications Identical Applications Client Reported Changes Client Inquiries Complaints Missing Information - No Anchor Task Fair Hearings Requests Handling of Inappropriate Documents Disaster SNAP Processing SSP Account Management Escalating Vendor Processing Issues Automatically Routed Tasks TIERS Alerts TIERS Unavailable Texas Health Steps Verification Process TIERS Case Assignment Reporting TIERS/State Portal Tickets Escalation of TIERS Tickets 3 December 2013 32 32 32 32 32 33 34 34 34 34 36 36 37 37 38 38 38 40 40 40 40 41 41 41 41 41 43 44 44 44 46 46 47 47 47 47 48 48 49 50 51 51 51 52 52 53 53 53 54 54 55 ES State Processes Help Desk Ticket Processing Issues Data Broker Resolution Task Failure Processing XVI. Support Tools Document Routing Procedures Complete Action and Disposition Coordination Document Upload First Time Sign-On Procedure for State Portal Ordering ES Materials Re-Linking Images State Portal Supervisor State Portal TLM TIERS/Portal Security Roles – MOR Workload Transfer Escalated Ticket Template Self Service Portal Application Registration Reminders XVII. Glossary of Terms 4 December 2013 57 58 58 60 60 60 60 60 60 60 61 61 61 61 61 61 62 ES State Processes I. December 2013 INTRODUCTION This document focuses on internal state processes and it is designed to identify the core responsibilities of state staff and to further document the processes within those responsibilities. It also provides basic information on key vendor functions. While automation is integral to the overall functioning of eligibility determination and case maintenance in the Texas Integrated Eligibility Redesign System (TIERS), the main focus is on the responsibilities of state eligibility determination staff (workers, clerks and management). The role of the state is to collect, review and ensure the accuracy and completeness of data collected by the vendor. State staff conducts interviews, process changes, determine client eligibility, process request for reviews, process appeals request, and serve as the agency representative for fair hearings. State staff and vendor staff use a work-flow mechanism called "Task List Manager" that is accessible through a common web-based State Portal. This software allows task to be created, claimed, comleted and monitored by staff based on their user roles. This material is divided into ten main work areas: Eligibility Offices, Customer Care Centers (CCC), Assistance Response Team (ART), Medicaid Eligibility for the Elderly and People with Disabilities (MEPD), Outstationed, Children’s Medicaid Centers (CMC), Women’s Health Program (TWHP), Central Processing Center (CPC), Centralized Benefit Services (CBS) and Performance Improvement. ES State Processes cover the procedures unique to those areas and those that cross areas. It also contains terminology related to the Eligibility Support Services process. Included at the end of this document are several Support Tools that are designed for quick reference. Note: Staff must continue to follow all policies and procedures located in the TW and MEPD Handbooks. 5 ES State Processes II. December 2013 ACCESS CHANNELS Access channels are various ways TIERS clients can apply for benefits, check the status of submitted applications, report or check the status of a change and several other options. These channels provide clients options when seeking assistance. Access channels include telephone, fax, mail, Internet and in person at the Eligibility Offices. Telephone Call (2-1-1) A caller has four services available when dialing the 2-1-1 phone number: Option 1 - Information and Referral (local community services) Option 2 - Eligibility (Vendor/Customer Care Centers) Option 3 - Office of Inspector General (OIG) to report fraud/benefit abuse. Option 4 – Register for evacuation and transportation assistance Once a call enters the 2-1-1 phone system, the caller must choose which services they need to access. An Interactive Voice Response (IVR) system prompts the caller for language and services, then routes the call accordingly. The IVR Options Menu is provided below for informational purposes. Option #1: Information and Referral, staffed 24 hours a day, 7 days a week by the local Area Information Center (AIC), provides information about all health and human services available in the community. Callers seeking help can obtain referrals regarding, but not limited to: Immediate needs services such as shelters and food pantries Other state and federal agencies Child care concerns Other community services offered Option #2: Eligibility provides information regarding State benefits and the ability for callers to apply for Texas Works or MEPD services. Services available by phone include: Applying for benefits (excluding FS) Screening for expedited food stamp eligibility Checking the status of applications or benefits Reporting changes Requesting fair hearings Rescheduling interviews Responding to Missing Information letters Checking the status of documents received by HHSC Updating their phone number Option #3: The OIG selection routes callers to state staff who accept and investigate reports of fraud and benefit abuse. Option #4: Allows individuals to register for evacuation and transportation assistance in the event of a disaster. 6 ES State Processes December 2013 Fax & Mail Applications received by the vendor via fax and mail, are processed according to the programs requested on the applications. Clients, authorized representatives, Community Based Organizations, and Eligibility Offices can fax and mail documents and applications directly to the vendor according to the Document Routing Procedures – TIERS Offices. Internet (SSP) The Self Service Portal (SSP) located at: www.yourtexasbenefits.com is available to TIERS clients 24 hours a day, 7 days a week. They can use this website to check the status of documents submitted to HHSC, submit applications, submit redeterminations, report changes, check the status of their benefits, and check future appointments. HHSC Eligibility Office All documents received by the HHSC Eligibility Office are date stamped, reviewed for completeness and processed according to the guidelines for programs requested. They are routed to the vendor when appropriate. Applicants will be given a receipt for any documents submitted in person or by mail at an Eligibility Office. 7 ES State Processes III. December 2013 GENERAL EXPECTATIONS Consistency is essential to the success of the Eligibility Support project. Therefore, state staff must follow these processes as closely as possible. The ES State Processes are designed to provide guidance for day-to-day activities. Although the intent of the procedures are to address common activities, there may be times when it is necessary and appropriate to seek guidance from management and/or follow established local office procedures. As a result of ES, many activities have become centralized. The primary centralized functions include: Document Processing Eligibility Determination for certain programs (both new applications and redeterminations) Change Processing Client/Applicant General Inquiry Support Fair Hearings Processing Request for Review Processing Vendor responsibilities include the following: Document imaging Image assembly and case association Responding to client inquiries and questions from 2-1-1 Rescheduling appointments using the State Portal Scheduler Accepting client reported changes Updating mailing addresses Routing work through State Portal and creating tasks appropriately for Texas Works and MEPD activities Routing and escalating complaints and fair hearing requests Routing Request for Reviews Enrollment Broker for CHIP/CHIP Perinatal 8 ES State Processes IV. December 2013 HHSC ELIGIBILITY OFFICE The Eligibility Offices are state offices where clients will be issued benefit access instruments and participate in ‘Face-to-Face’ or ‘Telephone’ interviews when applicable. Clients will also receive services from workers for ‘Home Visit’ interviews. The Eligibility Office staff will be responsible for several key activities, including, but not limited to: Issuing benefit access instruments (e.g. EBT cards, temporary Medicaid IDs). Performing identification verification and capturing biometric data (e.g., photographs). Conducting Face-to-Face, telephone and home visit interviews via a scheduled appointment. Completing Application Registration (App Reg) for applications when necessary. Completing all work end-to-end through final case disposition. Publishing Office Capacity at least 60 days out. Maximizing published appointment slots in the State Portal Scheduler for applications, expedites and redeterminations to allow the office to schedule and reschedule clients through the portal as needed. This will also allow the vendor staff to reschedule clients. Managing/monitoring office capacity and lead time daily to ensure application/redetermination processing timeframes are met according to policy guidelines. Scheduling and rescheduling appointments for applications, expedites and redeterminations through the State Portal Scheduler. Application Registration and Scheduling Tasks Prior to linking a mailed or faxed application to a case, the vendor will perform inquiry to determine if Application Registration is required and will initiate an Application Registration TLM task for processing. In addition, when clients submit an on-line application via yourtexasbenefits.com, an Application Registration TLM task will be routed to a state global queue based on the household’s residential zip code or the program type (See State Portal Support Tool: Task List Manager (TLM). The following Application Registration tasks are sent to a state TLM global queue: ‘Process a SSP Application Registration‘ ‘Process an Expedited SSP Application Registration’ ‘Process an Application Registration’ ‘Process an Expedited Application Registration’ ‘Process an Application Registration for Form 3038P’ Note: The Application Registration page in TIERS for a Self-Service Portal application will be pre-filled with data submitted via the www.yourtexasbenefits.com website. 9 ES State Processes December 2013 Designated staff will perform Application Registration in TIERS and establish a case number. If an interview is required or requested, staff must schedule the appointment using the State Portal Scheduler. TIERS will initiate the appropriate ‘Process Task’ at the completion of Application Registration if an appointment is not required or requested. If the vendor determines that the household has an existing TIERS case and Application Registration is not needed, the appropriate ‘Process Task’ will be routed to the state as they are today. If an interview is required or requested, the vendor will send a scheduling task. The task will be routed to a state global queue based on the household’s residential zip code or the program type. See State Portal Support Tool: Task List Manager (TLM) for additional information. The following scheduling tasks are sent to a state TLM global queue: ‘Schedule an Application Interview’ ‘Schedule an Expedited Interview’ ‘Schedule a Redetermination Interview’ Applications/Redeterminations - Received by HHSC Eligibility Office Applications/Redeterminations received in the Eligibility Offices are date stamped and screened for completeness and appropriate routing. Eligibility Offices are responsible for end-to-end processing of all Texas Works (TW) applications/redeterminations received in the Eligibility Offices that require or request an interview. Responsibilities include performing Application Registration, scheduling and completing all initial applications and redeterminations end-to-end. Application/Redetermination – Interview Required or Requested The following describes the appropriate processing for applications/redeterminations received in the Eligibility Office and an interview is required by policy or the interview is requested by the client (Food Stamps/TANF/TW Adult Medicaid). Once the application/redetermination screening steps are finished, staff must perform the following activities. Complete Application Registration, if necessary. Schedule the application in the office via the State Portal Scheduler according to program type and policy timeframes. Provide the client with Form H1830 - Application/Review/ Expiration/Appointment Notice. Process the case action end-to-end through final disposition including all associated programs. Process all TLM tasks appropriately. Mail all applications/redeterminations and supporting documents to Midland for imaging once final case action is taken and case is disposed. One Image Only cover sheet must be attached to each client packet. Complete appropriate forms to issue access to benefits when necessary. Issue EBT cards or Medicaid letters when necessary. Maintain communication with client as needed to process case actions. 10 ES State Processes December 2013 Note: If a non-expedite application or redetermination is received in the incorrect office, staff should follow the Document Routing Procedures – TIERS Offices and mail or fax it to the vendor for processing. Application/Redetermination – Interview Not Required or Requested The following information describes the appropriate processing/routing for applications/redeterminations received in the Eligibility Office and the requested program does not require an interview and the client has not requested an interview. These are organized by type of assistance because routing is different. Note: If the household is applying for multiple programs and any of the programs require an interview (i.e. application for Food Stamps and CMA), the application remains in the office for scheduling according to TW program policy timeframes. All programs must be processed end-to-end. Scheduled Interviews Applications/Redeterminations received in the Eligibility Offices are scheduled according to the type of assistance requested and TW program policy timeframes. Scheduling the appointment generates a task in the Eligibility Office TLM Global Queue. This section describes the Eligibility Offices processes and all activities that require an interview (Face-to-Face, Telephone, or Home Visit) and for clients who have requested interviews. These activities are processed end-to-end. The following task types are sent to the Eligibility Office TLM Global Queue based on the interview type: Face-to Face: ‘Check In a Face-to-Face Interview for a (Program) Application’ or ‘Check In a Face-to-Face Interview for a (Program) Redetermination’ Telephone: ‘Check In a Telephone Interview for a (Program) Application’ or ‘Check In a Telephone Interview for a (Program) Redetermination’ Home Visit: ‘Check In a Home Visit for a (Program) Application’ or ‘Check In a Home Visit Interview for a (Program) Redetermination’ Missed Appointments Whenever a client missing their scheduled appointment and the appointment task is marked as a ‘No Show’ one of the tasks below will be created: 11 Face-to Face: ‘No Show on a Face-to-Face Interview for a (Program) Application’ or ‘No Show on a Face-to-Face Interview for a (Program) Redetermination’ Telephone: ‘No Show on a Telephone Interview for a (Program) Application’ or ‘No Show on a Telephone Interview for a (Program) Redetermination’ Home Visit: ‘No Show on a Home Visit for a (Program) Application’ or ‘No Show on a Home Visit Interview for a (Program) Redetermination’ ES State Processes December 2013 Note: SNAP ‘No Show’ tasks will be flagged indicating automatic denial will occur on the associated EDG. Once the SNAP EDG is denied, based on policy, the associated TLM task will be automatically closed. The TLM will automatically create a task when other programs exist at the time of auto denial. When no other program exists and TIERS denies a SNAP EDG but the case is not in ongoing mode due to a case data change, a ‘Process a Change for a System Denial’ change task will be created and routed to the CCC. Note: DO NOT process missed appointments for programs that do not require interviews even if the client requested an interview, but failed to appear. Reschedules Requests for rescheduled appointment will be processed by the entity who receives the request. For instance, clients who request a rescheduled appointment through 2-1-1 will be rescheduled by the vendor staff. Individuals who contact the Eligibility Office to have their appointment rescheduled will be rescheduled by designated staff in that office. Note: Vendor staff can only process a reschedule if the original appointment was scheduled through the State Portal Scheduler. If the original appointment was not scheduled through the State Portal, they will refer the client to the eligibility office for rescheduling. Staff authorized to reschedule appointments must access the State Portal Scheduler to perform this task and must follow reschedule policy guidelines. Reschedule – Agency Error In the event a client is available to participate in a scheduled appointment but the worker/office is unable to process the interview, the appointment must be rescheduled. The process below outlines the steps staff need to follow when handling these reschedules due to agency error. 1. Appropriate staff marks the appointment task as “Show”. 2. Worker claims the “Show” task and completes the task as ‘Not Held – Agency Fault’. This task completion option will create a rescheduling task for the office. Note: Staff can also complete the Check-in task as “Not Held – Agency Fault” to create a reschedule task. 3. Designated staff claims the ‘Reschedule Face-To-Face Appointment for a (Program – Application/Redetermination)’; ‘Reschedule Home Visit Appointment for a (Program – Application/Redetermination); or ‘Reschedule Telephone Appointment for a (Program – Application/Redetermination)’ task. 4. Designated staff reschedules the client through the State Portal Scheduler, setting the “Why is this appointment being rescheduled?” field on the Schedule Appointment page to ‘Agency fault or request’. Once the 12 ES State Processes December 2013 appointment is rescheduled, the reschedule task will be automatically completed. Note: Vendor staff will delay rescheduling telephone appointments when the reschedule request is received on the day of the appointment and the request is due to no contact by the eligibility staff at the designated appointment time. Instead, vendor staff will ask the applicant/client to call the following day to reschedule the appointment if the eligibility staff does not contact them to conduct the interview on the appointment date. This is to allow eligibility staff an opportunity to contact the client/applicant throughout the day of the scheduled appointment to conduct the interview. End-to-End Processing (Including MI Received) Workers are responsible for processing all cases/EDGs end-to-end. Therefore, as tasks are received it is important to monitor the tasks for all EDGs associated with the case. Tasks should remain open until all associated EDGs are processed, and should not be completed prior to the task Due Date. For tasks with multiple EDGs, the EDG with the earliest due date is displayed. MI Received If missing information is received by the vendor, staff will see an open envelope icon on the TLM task. If the icon is present, the worker uses the Case Data Search feature in the State Portal to look for missing information images. The worker enters the information in TIERS Data Collection and runs eligibility to complete the case. After eligibility is run, the worker reviews results for accuracy. If missing information is received at the local office, staff will perform inquiry to determine the worker. If it is a worker in that office, it will be routed to that worker for processing. If the information belongs to someone who is not in the local office, staff completes an MI/Change Routing cover sheet and then the information will be faxed to MI/Change Routing fax line and the system will route the information appropriately. Fax to: 1-877-236-4123 Desk Review Applications/Redeterminations When HHSC receives a food stamp application or redetermination, a ‘Schedule an Interview for an Application or Redetermination’ task is created that informs the local office to schedule an interview. The task will have a ‘Desk Review’ completion option in addition to other current completion options if the application/redetermination potentially meets the following conditions: The task programs include FS, The task programs do not include TANF or MA, 13 ES State Processes December 2013 The associated case includes a FS EDG with a recertification status of Review Ready (RR) or Review Initiated (RI), The associated case does not include approved or pending TANF or MA EDGs, The associated case does not include a pending program request for TANF and The previous Food Stamps certification or recertification was not conducted with an appointment as recorded in TIERS marked as a desk review. Scheduling staff will follow the steps below to create a ‘Desk Review for a (FS/Combined TW) Application or Redetermination’ task. 1. Screen application/redetermination to determine if it meets the Desk Review policy. 2. If it meets the requirements, scheduling staff will select the ‘Desk Review’ completion option. This will result in the ‘Schedule an Interview for an Application or Redetermination’ task being closed and the Task List Manager (TLM) will create a ‘Desk Review for a (FS/Combined TW) Application or Redetermination’ task for the office. 3. The worker will retrieve the ‘Desk Review for a (FS/Combined TW) Application or Redetermination’ and process according to policy. Note: Staff should following local office procedures in the assignment and completion of the ‘Desk Review’ tasks. Applications Received by Eligibility Office If a FS application or redetermination is received by the eligibility office and it meets the desk review criteria, the following steps should be taken: 1. Scheduling staff should access the State Create Task page and manually create a ‘Desk Review for a (FS/Combined TW) Application or Redetermination’ task for the office. 2. The worker will retrieve the ‘Desk Review for a (FS/Combined TW) Application or Redetermination’ and process according to policy. Note: Staff should following local office procedures in the assignment and completion of the ‘Desk Review’ tasks. The TIERS automation changes restrict the ability of workers to select Desk Review as the value for the Appointment Mode field on the Appointment Details page only when the following criteria are met: The associated case currently does not include any approved or pending TANF or Adult Medicaid EDG (TP08), The associated case currently does not include a pending TANF program request, The associated case currently includes a SNAP EDG with a recertification status of Review Ready (RR) or Review Initiated (RI). The previous SNAP appointment was not conducted as a desk review and The appointment does not include TANF and does include SNAP. In addition, TIERS defaults the value of the Appointment Status field on the Appointment – Details screen to ‘Show’ and disables the field for input if the Appointment Mode field is set to ‘Desk Review’. 14 ES State Processes December 2013 Children’s Health Insurance Applications/Redeterminations State workers in centralized Children’s Medicaid Centers (CMC) or designated regional staff are responsible for: Processing Children’s Health Insurance applications and redeterminations for designated regions and Processing client complaints for those actions. For Children’s Health Insurance applications/redeterminations, the vendor sends a ‘Process a CMA Application’, ‘Process a CMA Redetermination’ or ‘Process a CHIP Redetermination’ task, depending on the case action, to the appropriate CMC Region queue based on the client’s residence zip code. In addition, CMC staff will also receive Application Registration tasks from the vendor or through the Self Service Portal for the programs they are responsible for processing. Staff should follow the instructions outlined in IV. HHSC Eligibility Office – Application Registration and Scheduling Tasks. 15 ES State Processes V. December 2013 CUSTOMER CARE CENTER Customer Care Center (CCC) is a virtual region located in six cities across the state. They are located in Athens, Austin, El Paso, Houston, Midland and San Antonio. CCC also includes a variety of centralized areas, including CCC Core, Central Processing Center (CPC), Centralized Benefit Services (CBS) and Texas Women’s Health Program (TWHP). CCC Core staff is responsible for: Processing non-interview activities from end-to-end, including changes, alerts, Process a System Denial, and missing information tasks; Processing certain Medicaid actions that do not require an interview; Evaluate Duplicate Application Tasks to confirm a complete action is or is not needed & address changes when no complete action is needed Handle “Process a Combined Redetermination” tasks. Processing agency-generated changes; Processing client-reported changes; Processing CHIP Six Month income checks; Processing CHIP Enrollment Broker Exceptions; and Addressing client complaints. Agency Generated Changes CCC/MEPD (MEPD CCC/MEPD Region (#) Change) staff is responsible for working all agency reported changes end-to-end. TIERS creates alerts for agency generated changes. ‘Alert (#): (Alert Description)’ (i.e. ‘Alert 106: Intentional Program Violation Disqualification Period Will End the Month’). Many of these alerts are converted automatically to TLM tasks and processed by CCC or other responsible area. There are still TIERS Alerts that staff are responsible for processing such as those related to Second Level Reviews. Staff should continue to check their Welcome to TIERS home page daily, and ensure the TIERS Alerts are processed appropriately. Note: For agency generated changes mailed to the local Eligibility Office, staff faxes the information to the vendor via the non-expedited fax line (1877-447-2839). Date Of Death (DOD) Alert Processing The Office of the Inspector General (OIG) receives reports from the Social Security Administration (SSA) and the Bureau of Vital Statistic (BVS) of individuals who are reported to be deceased. OIG systems match these reports to TIERS eligibility files to determine if the individual is known to TIERS. Once an individual is matched, the Deceased Individual Match information is sent to the TIERS system. The TIERS system will receive and update the TIERS Individual Date Of Death (DOD) information for all active and inactive individuals and will either: Or 16 Deny single household member cases using the (Perfect) BVS DOD Data Match information, ES State Processes December 2013 Create and route an appropriate DOD Action Alert TLM task for ES staff case action processing. TLM Date of Death alert tasks automate the Form 1186 process for Deceased Individual matches for OIG agency generated changes. ES staff does not need to complete the form H1186 or send it in for case record imaging. TIERS Mass Update Process Steps When possible, the TIERS Mass Update (MU) process will complete the following actions to a TIERS case: Populate the Date of Death within the Individual Data Collection page, Set the verification source to “BVS record/death certificate”, and If the case is active and in On-going mode, MU will run EDBC and take the appropriate TIERS case action to reduce or deny benefits. Or • When the Mass Update process is unable to take the appropriate TIERS case action, TIERS will trigger one of the following TLM Date Of Death Alert tasks requesting staff to process the Date Of Death data match information within TIERS for all active and inactive cases: Alert 810 - Process a Date of Death with a Perfect Match for Individual: X (where X is the individual ID) Alert 811 - Process a Date of Death with a Non-Perfect Match for Individual: X (where X is the individual ID) Alert 812 - Verify discrepancy in Date of Death for Individual: X (where X is the individual ID) Created when TIERS receives a record that exactly matches a TIERS individual, and the case is currently being worked (is in a mode other than Ongoing), or the deceased is the Head of Household. Occurs when TIERS receives a death record for an individual who seems to match a TIERS individual, but doesn't match exactly. Occurs when TIERS receives a record that exactly matches a TIERS individual, but the Date of Death does not match the Date Of Death already in TIERS. ES staff Date Of Death (DOD) Data Match Process Steps ES staff must review the task information take the appropriate TIERS case action to pend, reduce, or deny benefits. 1. Claim and review the TLM DOD Data Match information and TIERS case, 2. Document the needed DOD action in TIERS Case Comments, and 2.1. If the DOD TLM Alert source is BVS, then ES staff will: Review and if needed update the TIERS DOD, Review and if needed update the TIERS DOD Verification source, Document DOD action in TIERS Case Comments, and o If the case is active, run EDBC to reduce or deny benefits, accordingly. o If the case is inactive, no further action is needed by DI staff. Note: BVS Date Of Death (DOD) information received from BVS is an acceptable source of valid verification. 17 ES State Processes December 2013 Or 2.2 If the DOD TLM Alert source is SSA, then ES staff will: Pend the case using the Questionable HH Composition VCL to issue form H1020 requesting verification of the current household composition and residence location of the individual in question (the deceased). The notice sent to the decedent’s household will be sensitively composed to verify the individual’s date of death. Staff will document the following: “We have received notice that there is a change in your household composition. We have received a report that (deceased name) may no longer be in your home. Please provide verification of who is living in your home using the enclosed Domicile letter and return this form to us by (Due Date).” Ensure the form H1020-A Sources of Proof have both the “Domicile/Household Composition” and “Death” blocks selected. Note: SSA Date Of Death (DOD) information received from SSA is not an acceptable source of valid verification. 3. Staff is expected to follow existing TLM processing and complete the Date Of Death (DOD) MI TIERS case action and update the Individual page within Data Collection. Enrollment Broker Expection Task When HHSC staff disposes a CHIP/CHIP P EDG, an interface is sent to the Enrollment Broker vendor. If there is an issue that results in an interface expection, an alert is triggered and a TLM task is created and routed to CCC for processing. Clients will not receive their benefits until these actions are resolved. Below are the two exceptions tasks CCC staff will need to process: Alert 748 - CHIP Enrollment Broker Exception Alert 817 - CHIP EB MU Exception This alert is created whenever the information sent by TIERS does not match the Enrollment Broker system information. This alert is created during a mass update process and the Enrollment Broker system does not match the TIERS information. Changes Reported via OIG OIG receives information from Social Security Administration (SSA) and Bureau of Vital Statistics (BVS) Deceased Individual Matches; Texas Department of Criminal Justice (TDCJ) and Prisoner Verification System (PVS) Incarceration Matches; Public Assistance Reporting Information System (PARIS) Interstate Matches; and the Income and Eligibility Verification System (IEVS) Data Matches. Information is also received through the Hotline Call Center or the Waste, Abuse, and Fraud OIG website. OIG creates an Action Notice in ASOIG for the IEVS and Interstate matches that require action by ES staff. The ES Regional IEVS Match Coordinator logs into ASOIG to view the Notice. OIG tasks Region CCC Form 1186 for the TDCJ and PVS match alerts. 18 ES State Processes December 2013 Failure to Return Review Packet (091 Denials) Processing the denials of TANF, TANF-Level Medicaid or adult Medicaid households when the ‘Alert 816: Review Packet Not Returned’ task is received for individuals who fail to return their review packets and the case does not meet the auto-denial criteria. System Denial Task When a SNAP EDG is denied due to a missed appointment, and there are no pending EDGs, but TIERS does not put the case in ongoing mode a ‘Process a Change for a System Denial’ task is generated and assigned to the CCC for processing. CCC staff will need to review the case EDGs and determine the appropriate action needed. SNAP Terminated Task When an individual’s SNAP EDG is terminated, and the same individual is also an excluded member on a separate FS EDG/Case, an ‘Alert 732: SNAP Terminated Determination for FS Necessary’ task is generated for the FS EDG/Case and assigned to the CCC for processing. TW staff will need to make a FS determination according to policy for the individual. Duplicate Applications When applicants submit multiple applications, the vendor determines if the applications are either an identical copy or a duplicate application. If there is an identical application received, the vendor will link the identical application to the case for all programs. No task is routed to the state. If there is a duplicate application received for Texas Works, the vendor creates a ‘Duplicate (Program) Application’ change task and routes appropriately to the CCC. Due date calculation for the TW change task will follow change processing timeframes. If the duplicate application requests both MEPD and TW programs, the vendor will create two tasks; one routed to the appropriate MEPD Region and one routed to TW CCC. If the TIERS case has an active or pending TANF EDG, the vendor creates a ‘Duplicate Combined TW Application’ change task and routes the task to the CCC TANF queue. Due date calculation for the TW change task will follow change processing timeframes. Client Reported Changes CCC/MEPD (MEPD CCC/MEPD Region (#) Change) staff is responsible for working most client reported changes. This section outlines the process. 1. If a client reports a change directly to the staff, the staff takes the change and enters it into the State Portal - Report A TIERS Change portlet if it is received without verification. If the change is received with verification, staff completes an MI/Change Routing Cover Sheet and faxes it to the vendor (1-877-236-4123) without entering the information in the State Portal Report A TIERS Change portlet. 19 ES State Processes December 2013 2. If a client reports a change using the SSP, the information is passed to TIERS for processing. TIERS will attempt to automatically update the case without requiring worker action or create a ‘Change for a (Program) Case’ task. If TIERS determines additional information is required, the case is automatically pended and creates an ‘MI Requested on a SSP Change’ task and generates a Form 1020 – Request for information or action. SSP Exception Task When a TIERS attempt to automatically dispose an SSP change fails, a ‘Process a SSP Change Exception’ task is generated and assigned to the appropriate queue based on program(s) for processing. Staff needs to review the case EDGs and determine the appropriate action. Changes Reported via OIG OIG receives information from Social Security Administration (SSA) and Bureau of Vital Statistics (BVS) Deceased Individual Matches; Texas Department of Criminal Justice (TDCJ) and Prisoner Verification System (PVS) Incarceration Matches; Public Assistance Reporting Information System (PARIS) Interstate Matches; and the Income and Eligibility Verification System (IEVS) Data Matches. Information is also received through the Hotline Call Center or the Waste, Abuse, and Fraud OIG website. OIG creates an Action Notice in ASOIG for the IEVS and Interstate matches that require action by ES staff. The ES Regional IEVS Match Coordinator logs into ASOIG to view the Notice. OIG creates Form 1186 for the TDCJ and PVS matches and e-mails it to the Regional Match Coordinator to take the appropriate action. OIG sends Social Security Administration (SSA) and the Bureau of Vital Statistic (BVS) Date of Death information for individuals who are reported to be deceased to TIERS. The TIERS system will receive and update the TIERS Individual Date Of Death (DOD) information for all active and inactive individuals and will either: Deny single household member cases using the (Perfect) BVS Date Of Death Data Match information, Or Create and route an appropriate Date Of Death Action Alert TLM task for ES staff case action processing. Returned Undeliverable Mail When the vendor staff receives undeliverable mail other than a Form H1830, it is imaged and a task ‘Change for a (Program) Case’ is created and routed to the CCC/MEPD (MEPD CCC/MEPD Region (#) Change) Global Queue for review and processing. If a Form H1830 is returned as undeliverable, it is imaged and sent to the vendor as returned mail. The vendor staff checks the status of the appointment to determine if rescheduling is needed. 20 ES State Processes 21 December 2013 If the Appointment status is “No Show”, the vendor determines if the client reported a change of address. (such as USPS Form 3547, call to 2-1-1 with case comments in TIERS, updated address on application form in state portal). If a change was reported and the address does not match in TIERS, the vendor updates the mailing address in TIERS and attempts to contact the client by phone to reschedule the appointment. If the vendor is unable to make contact via phone, the appointment is rescheduled and the Form H1830 is mailed to the correct address allowing at least seven days for mail time. If they determine that the address on the 1830 matches the reported change information and no data entry corrections are needed, the vendor routes a task to CCC/MEPD (MEPD CCC/MEPD Region (#) Change) TLM Global Queue for appropriate action. ES State Processes December 2013 VI. TEXAS WOMEN’S HEALTH PROGRAM Women’s Health Program (WHP) began as a Medicaid pilot program in 2007. Effective November 1, 2012, WHP was replaced by the Texas Women’s Health Program. Designated TWHP staff located in San Antonio is responsible for processing TWHP applications and redeterminations. In addition, the TWHP staff process TP40 applications received by the vendor and changes for TIERS cases that contain only active WHP or TP40 EDGs. Texas Women’s Health Program (TWHP) - Applications TWHP applications are received by mail or fax from the local office and they are also received by the vendor who will route them via TLM – ‘Process WHP Application’. Texas Women’s Health Program (TWHP) – Redeterminations Women certified for TWHP may receive a Form H1867-R – Texas Women’s Health Program Renewal Application or a Form H1831 - Adjunctive Eligibility Letter for redetermination. Designated TWHP staff is responsible for processing ‘Process a WHP Redetermination’ and ‘Process a WHP Adjunctive Redetermination’ tasks. Pregnant Women Medicaid Applications Upon receipt of an application for Pregnant Women Medicaid, the vendor creates a ‘Process a PW Application’ task and sends it to the WHP TLM Global Queue for processing. TWHP staff will also receive Application Registration tasks for TWHP and Pregnant Women’s Medicaid from the vendor or through the Self Service Portal. Staff should follow the instructions outlined in IV. HHSC Eligibility Office – Application Registration and Scheduling Tasks. 22 ES State Processes December 2013 VII. CENTRALIZED BENEFIT SERVICES The Centralized Benefit Services (CBS) staff is located in Austin and is part of the CCC Region. The staff is responsible for processing SNAP-SSI cases for households in which all members receive Supplemental Security Income (SSI). The staff also processes Simplified Nutritional Assistance Program (SNAP-CAP), applications for Medicaid Breast and Cervical Cancer (MBCC) Program, Medicaid for children under the jurisdiction of the juvenile court and for youth under age 19 in non-secure facilities, Refugee Medicaid Assistance and any associated FS case, and Foster Care Transitional Medicaid. In addition, they process Request for Reviews for Reviews received on HCFFCHE and will assist with fair hearing requests received on some of their specialized programs. MTFCY Application/Redetermination Processing Designated CBS staff will be responsible for processing FM H1011 applications and redeterminations for the Medicaid for Transitioning Foster Care Youth Program from end-to-end. They will receive ‘Process MTFCY Application’ and ‘Process a MTFCY Redetermination’ tasks. FFCC Application Processing Designated CBS staff will be responsible for processing FFCC applications. They will receive ‘Process an FFCC Application’ tasks. MTFCY/FFCC Exception Task In some instances, a TIERS case containing MTFCY or FFCC EDG will contain an exception from interface files which must be cleared by CBS staff. Below are the exception tasks that are generated for CBS: Task Type Program MTFCY MTFCY Exception Task Name Alert 827: MTFCY Mass Update Exception Alert 822: MTFCY Citizenship/Alien Status Exception Alert 820: FFCC Mass Update Exception FFCC Alert 821: FFCC Citizenship/Alien Status Exception FFCC HC-FFCHE Redetermination Processing HC-FFCHE redeterminations received by the vendor will be routed via TLM to CBS staff responsible for processing the HC-FFCHE rederterminations from end-to-end. The staff will receive either a 'Process a HC-FFCHE Redetermination' task for these actions. 23 ES State Processes December 2013 HC-FFCHE Request for Review Task Clients who disagree with a decision on their HC-FFCHE case must submit a written request for a review of their case. Upon receipt of a request for review the vendor creates a ‘Request for Review for a HC-FFCHE Case’ task and sends it to the CBSHC-FFCHE Global Queue. CBS staff must review the information provided and take the appropriate action based on whether the client does or does not qualify for coverage. SNAP – SSI Application/Redetermination Processing Clients certified for SNAP -SSI may receive a Form H1840 – Recertification for SNAP – SSI Benefits. The vendor will create a ‘Process a FS-SSI Redetermination’ for timely redeterminations and a ‘Process a FS-SSI Application’ task if the packet is received after the 15th day and on or before the last day of the last certification month. These tasks will be routed to CBS staff responsible for processing the SNAP-SSI redeterminations from end-to-end. Note: Eligibility office staff is authorized to dispose SNAP-SSI applications interviewed at the local office, including untimely SNAP-SSI redeterminations. SNAP - SSI Interviews CBS staff will be responsible for scheduling and rescheduling face-to-face, telephone, or home visit interviews for SNAP-SSI according to policy. Simplified Nutritional Assistance Program (SNAP - CAP) Processing HHSC outreach potential SNAP clients by mailing them a SNAP – CAP application, Form H1841. CBS staff responsible for processing the SNAP – CAP applications from end-to-end will receive a ‘Process a FS-SNAP Application’ task in the CBS-FS-SNAP Global Queue. They will also receive a ‘Process a FS-SNAP Redetermination’ task for renewal packets received timely. Medicaid for Breast and Cervical Cancer Processing A woman applies for MBCC through a BCCS provider who forwards the MBCC Form H1034, Application for Medicaid for Breast and Cervical Cancer to a Department of State Health Services (DSHS) contact. DSHS then faxes the application to the vendor creates a ‘Process an Application Registration for TW’ or a ‘Process a MBCC Application’ task that is routed to CBS for processing. In addition, when a Form H2340 – Medicaid for Breast and Cervical Cancer Renewal is received, the vendor creates a ‘Process a MBCC Redetermination’ task that is routed to the CBS-MBCC queue. Individuals who received MBCC in another state and move to Texas will apply for MBCC using form H2340-OS, Out of State Application for Medicaid for Breast and Cervical Cancer. The vendor will create either ‘Process an Application Registration for TW’ or ‘Process a MBCC Out of State Application’ for these actions. 24 ES State Processes December 2013 In addition, CBS staff will also receive Application Registration tasks from the vendor for the programs they are responsible for processing. Staff should follow the instructions outlined in IV. HHSC Eligibility Office – Application Registration and Scheduling Tasks. RMA Processing Publishing Office Capacity RMA requires an interview; slots must be published using the Publish Office Capacity function in the State Portal. Supervisors are responsible for publishing the office capacity, and can refer to the State Portal – Supervisor Support Tool for further instructions. RMA must publish a sufficient amount of slots in the CBS-RMA queue to accommodate application volume. RMA Applications Designated CBS staff is responsible for processing RMA applications from end-to-end. A VolAg assists refugees in the application process and faxes form H1001, Application for Benefit Assistance from the Voluntary Agency (VOLAG) Fax Coversheet, along with form H1010, Texas Works Application for Assistance - Your Texas Benefits, to the vendor for routing. CBS staff will receive Application Registration tasks or Scheduling tasks from the vendor for the programs they are responsible for processing. Staff should follow the instructions outlined in IV. HHSC Eligibility Office – Application Registration and Scheduling Tasks. Note: RMA appointments must be scheduled as telephone interviews for routing to the CMA-RMA queue. Face-to-face and home visit interviews will be routed to a local office based on client zip code and must be coordinated with local office staff. Form H1001 & H1010 submitted Prior to or at the scheduled appointment time, the clerk must assign the ‘Check In a Telephone Interview for a RMA Application’ or ‘Check In a Telephone Interview for a Combined Application’, depending on the programs requested, task to a designated worker from the CBS-RMA TLM Global Queue. This moves the task to the worker’s TLM Personal Queue. The worker is then responsible for determining if the client is a "Show" or a "No Show" and marks the task accordingly. At the scheduled appointment time, the worker attempts to contact the client via telephone. If contact is made, the worker conducts the interview, initiates TIERS Data Collection, runs EDBC and sends MI if additional information is required, or certifies/denies the case. If all necessary information is available, an eligibility determination is made. The worker disposes the case in TIERS and sets the task in their TLM Personal Queue to ‘Task Completed’. This clears the task out of the worker’s TLM Personal Queue. 25 ES State Processes December 2013 VolAg Conservatorship Verification Task In instances when an unaccompanied refugee minor turns age 18, the month following the 18th birthday TIERS will trigger an alert which automatically creates an ‘Alert 802: Verify VolAg Conservatorship’ task. CBS staff will need to take the appropriate action based on whether the client is or is not under the conservatorship of a Volag. TYC/TJPC Applications CBS will mail form H1014, Application Information for Children's Health Insurance Program (CHIP), Children's Medicaid, and CHIP Perinatal Coverage, prior to the youths release from a facility. Upon receipt of form H1014, CBS staff will be responsible for performing Application Registration in TIERS, if required. Staff should follow the instructions outlined in IV. HHSC Eligibility Office – Application Registration Tasks This section outlines the process: Form H1014 Submitted Upon receipt of a Form H1014, CBS staff will perform Application Registration which upon submittal creates a ‘Process a TYC/TJPC Application’ task and sends it to the CBS Global Queue. A designated CBS worker claims the ‘Process a TYC/TJPC Application’ task from the CBS Global Queue. This moves the task to the worker’s TLM Personal Queue and the task is no longer visible in the CBS Global Queue. Medicaid for Inmates of a Public Institution Applications Incarcerated children and pregnant women who are admitted to a hospital that is not under the control of the Texas Department of Criminal Justice (TDCJ) for overnight treatment of a medical condition are potentially eligible for Medicaid coverage during their stay. TDCJ agent’s use the TDCJ fax coversheet and fax the coversheet and application to the non-expedite fax line. Upon receipt of a Form H1010 with the TDCJ Fax Coversheet, vendor staff will create a ‘Process a TYC/TJPC Application’ task and sends it to the CBS Global Queue. Designated staff will be responsible for processing these Medicaid for Inmates of a Public Institution applications submitted by TDCJ from end-to-end prior Medicaid. CBS Disposition Tasks In some instances, a TIERS case containing TW and/or MEPD EDGs will have a specialized CBS EDG associated to it and it may require CBS staff to dispose those benefits. Below are the tasks that are generated for CBS: 26 ES State Processes Task Type Disposition Program MTFCY HC-FFCHE FS-SSI SNAP MBCC RMA FFCC December 2013 Task Name Alert 801: MTFCY Has Not Been Disposed Alert 760: HC-FFCHE Has Not Been Disposed Alert 727: FS SSI Has Not Been Disposed Alert 730: SNAP Has Not Been Disposed Alert 791: MBCC Has Not Been Disposed Alert 799: RMA Has Not Been Disposed Alert 826: Has Not Been Disposed Note: The disposition tasks must be disposed the same day of receipt in order for the case to be moved to ongoing mode. Client Reported Changes SNAP - SSI Client Reported Changes SNAP-SSI recipients can report changes to HHSC in person, by phone, mail, or fax. Specialized CBS staff is responsible for processing the reported changes from end-toend. They will receive a ‘Change for a FS-SSI Case’ task in the CBS-FS-SSI TLM Global Queue for clients report changes to the vendor. SNAP – CAP Client Reported Changes The vendor will route a ‘Change for a FS-SNAP Case’ task to the CBS-FS-SNAP TLM Global Queue for SNAP – CAP client reported changes they receive. 27 ES State Processes December 2013 Agency Generated Changes In some instances, CBS staff will receive Agency Generated Alerts for the programs they process. Below is a list of tasks that will be routed to the appropriate CBS queue. Task Type Program MTFCY Task Name Alert 762: MTFCY TPR Information – nnnnnnnnn Alert 800: MTFCY – USCIS Alien Documentation is Expired Alert 761: HC-FFCHE TPR Information – nnnnnnnnn Alert 763: Verification of HC-FFCHE School Enrollment’ HH-FFCHE Agency Generated MBCC SNAP - CAP 28 Action Determine if adequate medical coverage needs to be updated for MTFCY clients TIERS automatically extends MTFCY certification period if the USCIS alien documentation is expired or will expire during the first month of the new certification period. Determine if adequate medical coverage needs to be updated for HC-FFCHE clients TIERS automatically extends HC-FFCHE certification periods and send a H1870, School Enrollment Verificaiton form to validate higher education information and create a task. Staff will take appropriate based on whether the form is received or not. Alert 803: HC-FFCHE – USCIS Alien Documentation is Expire TIERS automatically extends HC-FFCHE certification periods if she USCIS alien documentation is expired or will expire during the first month of the new certification period and staff will need to take appropriate action based on whether the client’s alien documentation has or hasn’t been renewed. Alert 792: MBCC TPR Information – nnnnnnnnn’ TIERS will generate an alert when TPR data is received for an MBCC cas. CBS staff will need to review these EDGs and determine if adequate medical coverage needs to be updated for MBCC clients. Alert 731: Dormant Advisor Action Necessary In the event a SNAP – CAP EDG account becomes dormant, TIERS will generate a Form H1030, SNAP Lone Star Card Assistance. If the client does not respond to Form H1030 within 10 days, TIERS will generate an alert that automatically creates an ‘Alert 731: Dormant Advisor Action Necessary’ TLM task is automatically created and routed to the CBS-FS-SNAP Global Queue. Staff will be responsible for processing these tasks according to policy. ES State Processes December 2013 VIII. MEDICAID FOR THE ELDERLY AND PEOPLE WITH DISABILITIES MEPD staff is located in the Customer Care Centers, throughout the state in Eligibility Offices and outstationed facilities. MEPD staff located in the CCC assist the regions with processing changes, alerts, and MEPD complaint tasks as well as take all escalated MEPD Vendor calls. The San Antonio CCC has the sole responsibility of working all IEVS that were generated since July 15, 2012. MEPD staff located in Eligibility Offices are responsible for processing all MEPD applications/redeterminations and changes (including MSP, MBI, Referral, and Facility application/redeterminations and changes), and MEPD staff located in outstationed facilities are responsible for processing applications/redeterminations and changes for clients in those facilities. MEPD Applications All MEPD applications received in the local offices will be mailed or faxed to the vendor for imaging and task creation. A ‘Process a (Program) Application’ TLM task is created and routed to the appropriate MEPD regional queue based on the client’s zip code. In addition, the vendor or Self Service Portal will create a ‘Process a MEPD Application Registration’ task for the programs they are responsible for processing. Staff should follow the instructions outlined in IV. HHSC Eligibility Office – Application Registration and Scheduling Tasks. MEPD Interview Requested Face-to-face, telephone or home visit interviews are not required for MEPD. It is however, good casework practices to contact the client or authorized representative on every application. MEPD Management prefers this practice. If a client requests an interview, the scheduling process will follow the TW processes. Since interviews are not required, MEPD EDGs cannot be denied for failure to keep an appointment. MEPD Redeterminations MEPD redeterminations follow the same processes as MEPD application processing. Once the ‘Process a (Program) Redetermination’ TLM task is complete and the redetermination disposed in TIERS, the worker sets the task in their TLM Personal queue to ‘Task Completed’. This clears the task out of the worker’s TLM Personal queue. Note: When a MEPD worker discovers that a TLM task being worked includes a request for MBI, the worker completes the task using a new task completion option called ‘Transfer to MBI Queue’. By doing so, the existing MEPD task is automatically routed to the MBI Global Queue, and is re-named as a MBI task, with the Program and Location set as MBI. 29 ES State Processes December 2013 Reschedules Requests for rescheduled appointment will be processed by the entity who receives the request. For instance, clients who request a rescheduled appointment through 2-1-1 will be rescheduled by the vendor staff. Clients who contact MEPD staff to have their appointment rescheduled will be rescheduled by designated MEPD staff. Note: Vendor staff can only process a reschedule if the original appointment was scheduled through the State Portal Scheduler. If the original appointment was not scheduled through the State Portal, they will refer the client to the eligibility office for rescheduling. LIS MSP Application Processing The Medicare Improvements for Patients and Providers Act (MIPPA) of 2008 requires the Social Security Administration (SSA) (with the consent of those filing) to transmit LIS (Low Income Subsidy) application data to the States. Once received, the LIS data would serve as a protective filing for MSP (Medicare Savings Programs), with State agencies being required to complete appropriate MSP development and make eligibility determinations. The LIS MSP applications are processed by a single unit located in El Paso. This unit is tasked with processing all LIS MSP applications. When a Form H1200EZ-MSP is returned for an individual known to TIERS or that is LTC converted in TIERS, a ‘Process a LIS MSP TIERS Application’ task will be generated in the LIS MSP Global Queue. In addition, if one is returned for an individual unknown to the system, a ‘Process a LIS MSP Unknown Application’ task. Medicaid Buy-In (MBI) Applications with requests for MBI, as well as other MBI-related work, will be routed to the statewide MBI TLM work queue. Staff will receive a ‘Process a MBI Application’ or a ‘Process a MBI Redetermination’ task. Note: When a case that has only a MBI EDG as the active MEPD program and a change or a complaint is received for the case, then separate change or complaint tasks shall be created and routed to the new MBI Global Queue. Medicaid Buy-In for Children Processing When an application or redetermination for MBIC is received and imaged, a ‘Process a MBIC Application’ or ‘Process a MBIC Redetermination’ task is created and routed to the corresponding MBIC regional queue based on the applicant’s residence address zip code. Note: If a disability determination is requested, staff can Select ‘Awaiting Disability Determination’ and the task completion option which will update the task name and due date. 30 ES State Processes December 2013 MEPD Referrals A referral must be made with any request for eligibility for any of the DADS wavier or Community Attendant (CA) services. Upon receipt of the Form H1746-A - MEPD Referral Cover Sheet, the vendor will generate a ‘Process a MEPD Referral Application (or Redetermination, or Change)’ TLM task for MEPD Referral applications, redeterminations, and changes, which will be routed as appropriate. Note: Until the messaging function of the DADS system is operational, the MEPD worker will continue to notify DADS of the eligibility result using the established DADS communication tool found at: http://dadsview.dads.state.tx.us/me-to-dads/ The MEPD worker will only indicate if the client’s case has been certified or denied and the denial reason. Agency and Client Generated Change / Significant Change Processing This section outlines the steps for processing MEPD client reported and agency generated changes for waiver and Community Attendant (CA) cases. When a significant change occurs, such as a denial of any of the functional eligibility components, or a change in living arrangement, Adverse Action from Appeals, or Death of the client, the DADS System (when operating) will communicate this change for TIERS to populate the required pages. A ‘Change for a (Program) Case’ TLM task, including the appropriate change type related to the TIERS data update being performed, is generated for the worker to review eligibility, run EDBC, and dispose. The distinction between different change types will be seen in a change type attribute value associated with each task. This attribute is viewable when a specific task is “expanded” to look at its details, and is also available as a search criterion in the Advanced Filter. TLM will support the following new change types for TLM Change tasks: Discharged from Facility Admitted to Facility LTSS Functional Assessment Update LTSS Monthly Cost of Care Change CC Waiver Denied CC Waiver Transfer Demographic Change ISP Update Income and/or Resource Update Note: Upon receipt of Form H1263, Certification of Medical Necessity, the vendor will generate and route a ‘Process a MEPD IME Change’ TLM task to the appropriate MEPD regional queue for processing. 31 ES State Processes August 2013 MEPD Regional Change Processing Each region will be responsible for processing client reported and agency generated changes received in their MEPD Region (#) Change queue from end-to-end. They will be responsible for processing the complaints routed to these queues as well as MEPD dispositions tasks. Note: CCC MEPD will be responsible for processing tasks that the system is unable to route to a MEPD Region (#) Change queue. Changes and Returned Mail MEPD staff processing client reported changes, agency generated changes and returned mail from the MEPD Region (#) Change queue should following instructions outlined in Section V. Customer Care Center – Client Reported Changes, Agency Generated Changes and Returned Undeliverable Mail sections. Date Of Death (DOD) Alert Processing MEPD staff processing DOD related alerts should follow Section V. Customer Care Center – Date Of Death (DOD) Alert Processing section. MEPD Disposition Tasks In some instances, a TIERS case containing HC-FFCHE, FS-SSI and/or SNAP EDGs will have an associated TW and/or MEPD EDG. Upon running EDBC, TIERS will generate an alert that automatically creates an ‘Alert 729: MEPD EDG Has Not Been Disposed’ TLM task when disposition is needed. This task will be sent to the MEPD Region Change MEPD Regional staff will need to review these EDGs and determine the appropriate action needed. Note: The disposition tasks must be disposed the same day of receipt in order for the case to be moved to ongoing mode. Failure to Return Review Packet MEPD Change Regions are responsible for processing the denials of MEPD households when the ‘Alert 816: Review Packet Not Returned’ task is received for individuals who fail to return their review packets and the case does not meet the auto-denial criteria. Duplicate Applications When applicants submit multiple applications, the vendor determines if the applications are either an identical copy or a duplicate application. If there is an identical application received, the vendor will link the identical application to the case for all programs. No task is routed to the state. If the duplicate application received is for MEPD, the vendor creates a ‘Duplicate MEPD Application’ change task and routes appropriately to the MEPD Region queue. Due date calculation for the MEPD change task will follow change processing timeframes. If the duplicate application requests both MEPD and TW programs, the vendor will create two tasks; one routed to the appropriate MEPD Region and one routed to CCC. 32 ES State Processes December 2013 Additional Processes For more MEPD detailed processes, including the most recent version of the MEPD Operating Procedures, please refer to the MEPD Website. Refer to the "Processes for MEPD Virtual Staff" found in the appendices of the MEPD Operating Procedures for specific information on processing forms related to transferred resources and subrogation. 33 ES State Processes IX. December 2013 OUTSTATIONED/FACILITY WORKERS HHSC currently contracts with over 300 health care providers (hospitals, clinics, nursing homes, etc) for approximately 600 Outstationed Worker Program (OWP) positions. These positions are filled by Texas Works and MEPD staff who determines eligibility for all ES programs, with an emphasis on the medical programs. Staff in these outstationed facilities is responsible for processing work from end-to-end and routing completed work to the vendor as Image Only. Texas Works and MEPD staff is responsible for performing inquiry and Application Registration as needed. MEPD staff will use the State Portal to view images, access TIERS and Datamart reports. Texas Work staff will also use the State Portal to view images, access TIERS and Datamart reports and they will also use the State Portal Scheduler and TLM for their scheduled appointments. Texas Works staff will also be responsible for publishing appointment slots for their outstationed facility in the State Portal Scheduler – Publish Office Capacity. MEPD Processing When an MEPD application is received, MEPD outstationed/facility staff will ensure the appropriate MEPD task is created when performing Application Registration or manually creating a process task using the State Create Task page. Within 24 hours after the appropriate task is created, staff must route the application/redetermination/supporting documents to the vendor as Image Only. MEPD Facility Requests The vendor will screen Forms H1200, H1200EZ, and H1200PFS to determine if the applicant is requesting Facility services. A ‘Process a MEPD Facility Application (or Redetermination)’ TLM task will include one of four designated MAO Types (State School, Nursing Facility, ICF-MR, or State changes, alerts and MEPD complaint tasks will be routed to the MEPD Region Facilities queue based on the client’s residence zip code and program hierarchy. If the EDG is assigned to an individual other than the TAAGeneric Worker, the system will automatically assign the task to that individual in their personal queue. If the EDG is assigned to the TAAGeneric Worker, the task will be routed as unassigned in the global queue. Note: If MBI is included as a program, the task is routed to the MBI Queue. If MBI is not present but MBIC is included as a program, the task is routed to the MBIC Regional Queue. Texas Works Processing When a Texas Works application is received, Texas Works outstationed will ensure the appropriate Texas Works task is created when performing Application Registration, manually creating a process task using the State Create Task page or scheduling an appointment. They will also ensure it is assigned to the appropriate outstationed location. 34 ES State Processes December 2013 NOTE: Staff can only schedule appointments to a specific outstationed facility if they have a portal role for that outstationed facility. Once the eligibility decision is made, the completed paper forms are routed to the vendor as Image Only. 35 ES State Processes December 2013 X. CENTRAL PROCESSING CENTER The Central Processing Center (CPC) is comprised of ES staff located in Austin and are part of the CCC Region. These staff is responsible for processing all children's Medicaid referrals and steam lined Forms H3038P CHIP Perinatal Emergency Medical Services Certification. CHIP Perinatal Form H3038P Process CHIP Perinatal clients whose income is below 185% of the Federal Poverty Income Limit (FPIL) are not required to complete an application to apply for Emergency Medicaid for the birth of their child. Instead, a Form H3038P is generated by TIERS and mailed to the client to complete and return. All Forms H3038P are routed to CPC for processing. Once a Form H3038P is received by the vendor, a ‘Process a Form 3038P’ or a 'Process an Application Registration for Form 3038P' task will be systematically created and routed to the CPC TLM global queue. If the Form H3038P is received in the local eligibility office, staff should follow the instructions in the Document Routing Procedures - Support Tool and fax to the vendor. Note: When a Form H3038P is returned sixty (60) days after the child’s due date listed in TIERS, inform the client they must reapply for benefite. 36 ES State Processes December 2013 XI. CENTRALIZED REPRESENTATION UNIT The ES-Centralized Representation Unit (ES-CRU) staff represents the agency in ES Texas Works and MEPD fair hearings. Note: CBS is responsible for processing MTFCY and RMA fair hearing requests and FFCHE Requests for Review. Fair Hearings Processing Individuals may request a fair hearing in person, in writing, or over the phone to appeal a case action or to dispute policy. All TIERS fair hearing requests will be entered in to the State Portal and routed to the ES-Centralized Representation Unit (ES-CRU) for processing. Initial Fair Hearing Request The ES-CRU will receive a ‘Appeal Request for (program/TOA)’ and review the case, perform case corrections if appropriate and will create a fair hearing request in TIERS that is sent to the Hearing Division. Scheduled Fair Hearing Request Once the fair hearings request has been scheduled by the Hearings Division staff, a ‘Fair Hearing Appointment for a (Program) Case’ task will be routed to the Fair Hearings Centralized Unit TLM Global Queue. Note: A “Star” icon will appear on the task if the Fair Hearings Officer assignment changes. Fair Hearing Decision Once the fair hearing has been held and a decision has been rendered, the hearings officer records the decision in TIERS and a TLM task is created and routed to the Fair Hearings Centralized Unit TLM Global Queue for processing. If the decision is reversed, a ‘Process Fair Hearings Reversal Decision for (Program/TOA)’ TLM task is created and routed to Fair Hearings Centralized Unit TLM Global queue. If the decision is sustained and the conditions below are met, a ‘Fair Hearings Sustain Decision for (Program/TOA)’ task will be created and routed to the Fair Hearings Centralized Unit TLM Global Queue and for processing. 37 Conditions include: A decision is made that does not “reverse” the previous agency determination, the case is eligible for continued benefits and the client has not waived the right to continued benefits. A ‘ Fair Hearings Decision Issued for (Program/TOA)’ task will be created for decisions issued that do not typically require an agency action. ES State Processes December 2013 XII. CHIP REQUEST FOR REVIEW (RFR) The CHIP Request for Review Unit represents HHSC in CHIP and CHIP Perinatal Request for Reviews. Request for Review Processing A request for review is any expression of dissatisfaction with an adverse action for a CHIP or CHIP Perinatal case. Households have thirty (30) business days from the date the notification letter was sent to the household. The request for review must be submitted in writing. The following task is created by the vendor and routed to the Fair Hearings global queue: ‘Initiate Request for Review’ Once the CHIP RFR staff claim and mark the above task as ‘Complete’, one of the tasks below will be created and assigned to them in their personal TLM queue. ‘Process a Request for Review for a CHIP Case for EDG: XXX’ ‘Process a Request for Review for a CHIP-P Case for EDG: XXX’ RFR Questions If state staff has questions or concerns about an RFR, they can contact the RFR staff listed below: CHIP RFR Questions: Merlin Crow: merlin.crow@hhsc.state.tx.us, Dayo Aliu: dayo.aliu@hhsc.state.tx.us. CHIP-P RFR Questions: Yvette Mathews: Yvette.matthews@hhsc.state.tx.us If a client has a question about their RFR, they can contact 2-1-1 or their local office. Request for Continued Enrollment Processing If the child's physician or health plan determines that a suspension or termination of enrollment could seriously jeopardize the child's life or health, the household can request Continued Enrollment. The following task is created and routed to the Fair Hearings global queue: ‘Initiate Request for Review with CE’ Once the CHIP RFR staff claim and mark the above task as ‘Complete’, one of the tasks below will be created and assigned to them in their personal TLM queue. 38 ES State Processes December 2013 ‘Process a Request for Review with CE for a CHIP Case for EDG: XXX’ ‘Process a Retro Request for a CHIP Case for EDG: XXX’ ‘Process a Retro Request for a CHIP-P Case for EDG: XXX’ The following tasks are used to communicate between Medicaid CHIP Division (MCD) and CHIP RFR when a Health Plan Retro Coverage Request or CHIP Enrollment Fee Extension Request comes directly to HHSC. When the CHIP RFR needs to inform MCD that a Health Plan Retro Coverage Request or CHIP Enrollment Fee Extension Request has been requested they will send the following manual task to MCD Any detail information MCD needs to complete their task will be entered in the comments. ‘Process a CHIP/CHIP-P Health Plan Retro Coverage Request’ ‘Process a CHIP Enrollment Fee Extension Request’ When MCD has completed their step for either the Health Plan Retro Coverage Request or CHIP Enrollment Fee Extension Request they will send the following manual response task back to CHIP RFR. Any detail information HHSC needs to complete their task will be entered in the comments. 39 ‘Process a CHIP/CHIP-P Health Plan Retro Coverage Response’ ‘Process a CHIP Enrollment Fee Extension Response’ ES State Processes December 2013 XIII. DATA INTEGRITY Data Integrity is responsible for processing manual certifications for ME-SSI and processing certain changes on those benefits. They add Medicare Cost Share for SSI client’s only, clear rejections from interface files, and process Managed Care corrections. In addition, they are responsible for processing Medicaid for newborns, Merge/Separate actions, as well as processing demographic changes on individuals who have been file cleared and certified. Change for a MEPD-SSI Case TLM task When a change for an ME-SSI EDG is reported, the vendor creates a ‘Change for a MEPD-SSI Case’ TLM task. The change task will have one completion option: ‘Task Completed’, with a due date of one business day. Upon receipt of a change for a ME-SSI EDG, the vendor creates a ‘Change for a MEPD-SSI Case’ task and sends it to the DI Global Queue for processing. Freeze Flag Alerts Since SSI cases are the responsibility of DI, they will be given the option to set an indicator called ‘Freeze SDX Update’ on the EDG address in TIERS that will prevent the SDX interface from updating the EDG address. DI will be the only group with access to set and release the ‘freeze’ indicator. Note: The ‘freeze’ indicator when set, will not limit other authorized users’ ability to update EDG addresses. When the SDX interface attempts to update the address of an EDG with the ‘freeze’ indicator set, TIERS will not allow the transaction. In addition, the TLM task, ‘Alert 764: SDX Address Update Not Processed Due to Freeze’, will be created and sent to DI for processing. The task will require DI to review the SDX update and determine if the Social Security Administration (SSA) requires notification of the change. ME SSI Manual Certifications DI ME SSI Eligibility staff is responsible for ME SSI Medicaid and ME SSI Facility Medicaid certifications, disposals, and denials. They also make corrections to addresses and county codes for eligible SSI recipients statewide. Staff can send these ME SSI requests to the following mailbox: HHSC CCC Data Integrity Program @hhsc.state.tx.us All emails sent to the HHSC TIERS Disposition Request mailbox should include the following information: 40 Client name Case number Nursing facility name ES State Processes December 2013 Date client entered/discharged from the nursing facility (if appropriate) Brief description of the action that is needed Medicare Buy In Data Integrity Buy In staff adds Medicare Cost Share for SSI clients only and clear rejections from interface files. If field staff receives inquiries/complaints in the local office for client’s whose Medicare Cost Share has been certified for 120 days or more and their Medicare premium continues to be deducted or SSI client who have Medicare Part A and their QMB coverage has not been established, emails should be sent to HHSC CCC Data Integrity Program @hhsc.state.tx.us. All emails sent to the HHSC DI_Buy In mailbox should include the following information: Client name Case number Brief description of the action that is needed QI-1 Data Integrity QI-1 staff process a monthly billing voucher for the HHSC accountants to charge or reimburse for monthly premiums paid for coverage that has started or ended. The DI staff is informed of the coverage that is granted or terminated via the Form 3081. MEPD field staff is responsible for sending a completed Form 3081 to Data Integrity by mail, fax, or email to the following mailbox: HHSC CCC Data Integrity Program @hhsc.state.tx.us. Managed Care DI Managed Care staff is responsible for reviewing and correcting discrepancies in Managed Care coverage. These requests are received from the Managed Care Operations Enrollment Broker Managed Care Specialists. Requests are sent to the following mailbox: HHSC CCC Data Integrity Program @hhsc.state.tx.us Newborn Eligibility Data Integrity Newborn Eligibility staff are responsible for researching and correcting discrepancies in Medicaid eligibility for newborns whose mother is Medicaid eligible. They also clear exceptions from interface files and process referrals received from hospitals. The hospitals are responsible for sending these requests to Data Integrity by mail, fax, or email to the following mailbox: HHSC CCC Data Integrity Program @hhsc.state.tx.us. Merge & Separate All merge or separate requests need to be requested in TIERS via the Data Integrity functional area on the Left Nav. When merge or separate requests are made in TIERS, the corresponding TLM tasks are created for Data Integrity (DI) staff. DI merges client individual numbers only. Case numbers cannot be merged. If it is determined that additional case actions are needed by eligibility staff, prior to processing the merge or 41 ES State Processes December 2013 separate action, DI will complete the merge or separate task with the appropriate completion option which will result in the following tasks: If further case actions are needed to process the merge or separate the system will create a ‘Perform Requestor Pre-merge/separate Casework’ task and assigns the task to the individual who made the initial merge or separate request. If the system is not able to assign a TLM task to the individual who requested the merge or separate, a task will be routed to the requestor’s primary TLM location. If further case action is needed by field staff other than the initial requestor the system will create a ‘Perform Field Staff Pre-merge/separate Casework’ task and assigns the task to the global queue of the office who serves the case residential zip code. If the merge or separate action results in a change in benefits the system will create a ‘Perform Disposition Casework for a Merge/Separate’ task and assigns the task to the individual who made the initial merge or separate request. If the system is not able to assign a TLM task to the individual who requested the merge or separate, a task will be routed to the requestor’s primary TLM location. Note: The disposition tasks must be disposed the same day of receipt in order for the merge or separate process to resume. If a merge or separate request is determined invalid the system will create a ‘Merge/Separate Request Not Successful’ task and assigns the task to the individual who made the initial merge or separate request. If the system is not able to assign a TLM task to the individual who requested the merge or separate, a task will be routed to the requestor’s primary TLM location. Once the merge or separate process is determined successful the system will create a ‘Merge/Separate Request Successfully Completed’ task and assigns the task to the individual who made the initial merge or separate request. If the system is not able to assign a TLM task to the individual who requested the merge or separate, a task will be routed to the requestor’s primary TLM location. Note: All case work must be completed prior to requesting the merge. All cases need to be denied or in Ongoing Mode prior to requesting the merge. Staff should review the “Preventing and Resolving Multiple ID Numbers in TIERS Cases” job aid for client individual numbers on multiple active cases. Staff follows the steps below: The worker reviews the task comment to determine what case action is needed. The worker completes case processing in TIERS and disposes the case, if necessary. The worker marks the TLM task to ‘Task Completed’. This clears the task out of the worker’s Personal Queue and releases the ‘on hold’ status of the ‘Process a Merge/Separate Request’ task if applicable. 42 ES State Processes December 2013 Biographical Corrections All Texas Works and MEPD staff have the ability to correct name, phone numbers, and address information in TIERS. Data Integrity Bio Corrections staff process gender, SSN, SSCN, and DOB corrections. If file clearance has occurred and the individual certified, staff can send requests to DI at the following mailbox: HHSC CCC Data Integrity Program @hhsc.state.tx.us. All emails sent to the HHSC DI Biographical Corrections mailbox should include the following information: 43 Client name Client number Case number Brief description of the action that is needed ES State Processes December 2013 XIV. ES CBO REGIONAL OFFICE ES CBO Regional Office is comprised of eligibility staff located in Region 8 and they are responsible for processing applications/redeterminations from one of five food banks within Texas that are authorized to conduct interviews on behalf of HHSC. These five food banks are a part of the Community Partner Interviewer pilot (CPI). These CPIs have the ability to submit applications and redeterminations via the Community Partner (CP) Self Service Portal (SSP), e-mail, paper or fax and they will designate the CBO Mode as ‘Assisted’ or ‘Interviewed’. The CPI Interviewer is responsible for identifying the CBO Mode on the CBO Non-Interviewed, Non-Expedited Application Cover Sheet or within the SSP. ‘Interviewed’ applications means the CPI Interviewer conducted a SNAP program interview on behalf of HHSC, and either obtained or informed the applicant of the required program verifications necessary for HHSC to determine eligibility. The CPI Interviewer can only conduct interviews for the SNAP program. ‘Assisted’ Applications/Redetermination Processing ‘Assisted’ applications means the CBO helped the applicant with completing the application, accessing the SSP, gather supporting documents, and informed the applicant of the general information HHSC will need to determine benefit eligibility using HHSC Form H1858. If an ‘Assisted’ application or redetermination is received from the CBO by FAX or mail, the designated Region 8 staff will process the action by either scheduling an appointment or manually creating a ‘Process a [Program] Application’ or ‘Process a [Program] Redetermination’. If an ‘Assisted’ application is received from the CPI via the CP SSP, TLM automatically creates a ‘Process a SSP Application Registration‘ or ‘Process an Expedited SSP Application Registration’ task and routes to the local ES office based on the applicant’s zip code. Staff will follow current SSP procedures to process the application. ‘Interviewed’ Application/Redetermination Processing If an ‘Interviewed’ application or redetermination is received from the Region 8 staff by FAX or mail, designated staff will review the application to determine if the client has requested other programs besides FS that requires an interview. If an additional interview is not required on the faxed or mailed document, the staff will: 1. Perform Application Registration and enter the CBO information is entered correctly and answer the CBO question appropriately if needed. 2. If Application Registration performed, TLM will automatically create a ‘Process a [FS or Combined TW] CBO Interviewed Application’ tasks. If Application Registration is not needed, staff manually create a ‘Process a CBO Interviewed Application for [FS or Combined TW]’ or ‘Process a CBO Interviewed Redetermination’ for [FS or Combined TW]’ task. 44 ES State Processes December 2013 3. The worker claims the task and processes the application appropriately. If an additional interview is required on the faxed or mailed document, the staff will 1. Perform Application Registration and enter the CBO information is entered correctly and answer the CBO question appropriately if needed. 2. Schedule the appointment in the State Portal Scheduler to create a ‘Check in a [Face-To-Face or Home Visit or Telephone] Interview for a CBO Interviewed Combined TW Application’ or ‘Check in a [Face-To-Face or Home Visit or Telephone] Interview for a CBO Interviewed Combined TW Redetermination’ task. 3. The worker claims the task and processes the application appropriately. If an ‘Interviewed’ application is received from the CBO via the CP SSP, TLM automatically creates and routes a ‘Process a CBO SSP Interviewed Application Registration for [’TW’ or ‘Combined TW-MEPD’]’ or ‘Process an Expedited CBO SSP Interviewed Application Registration for [’TW’ or ‘Combined TW-MEPD’]’ The designated staff reviews the application to determine if the client has requested other programs besides FS that requires an interview. If an additional interview is not required, the staff will 1. Complete Application Registration and ensure the CBO information is correct and answer the CBO question appropriately. 2. Once App Reg is complete, TLM will automatically create a ‘Process a [FS or Combined TW] CBO SSP Interviewed Application’ task. 3. The worker claims the task and processes the application appropriately. If an additional interview is required, the staff will 1. Perform Application Registration and ensure the CBO information is correct and answer the CBO question appropriately. 2. Schedule the appointment in the State Portal Scheduler to create a ‘Check In a [phone, face, home] Interview for a CBO Interviewed ’Combined TW’ Application’. 3. The worker claims the task and processes the application appropriately. Note: Staff performing Application Registration must ensure that the CBO related information is entered correctly within Application Registration. In addition, staff processing CBO related actions must ensure all CBO related information is correctly entered within the TIERS CBO Logical Unit of Work. If an ‘Interviewed’ SNAP redetermination, which does not include TANF or Adult Medicaid, is received from the CBO via the CP SSP, TLM automatically creates and routes the following: ‘Process a CBO SSP Interviewed Redetermination for [’FS’ or ‘Combined TW’]’ If an ‘Interviewed’ SNAP redetermination is received from the CBO via the CP SSP, and another interview is needed for TANF or Adult MA, TLM automatically creates and routes the following: 45 ES State Processes December 2013 ‘Schedule a Redetermination Appointment Task for [’FS’ or ‘Combined TW’]’ Reschedules In instances where applicants request a rescheduled appointment by contacting the local office or through 2-1-1, the caller will be re-directed to the designated ES CBO Regional contact person to reschedule the ES CBO Regional appointment. Note: Only authorized ES CBO Regional staff may reschedule CBO appointments. CBO Documents Submission The CBO routes paper applications, supporting documents and Missing Information (MI) directly to their assigned HHSC CBO Regional Office via Encrypted Voltage e-mail, fax or hand-delivery. If a document is routed to the vendor, it follows normal business flows and is not identified as a CBO document. All documents received by DPC will follow existing processes. CPs can also upload support documents via SSP during the application and redetermination submission process or later when a case number exists for the SSP application. ES CBO Contacts Region Contact Name Karen Gordon – TW Supervisor Melissa Torres – Program Manager Dee Ann Smith – Lead Program Manager Grace Moser – Regional Director 8 46 Phone Number Community Partner (210) 646–3516 (210) 619-2946 (210) 619–8260 (210) 619–8019 North Texas Food Bank (NTFB) San Antonio Food Bank (SAFB), South Plains Food Bank (SPFB), Tarrant Area Food Bank (TAFB), Houston Food Bank (HFBO) ES State Processes December 2013 XV. GENERAL PROCESSING This section provides information that is used by Eligibility Office, ART, CCC and MEPD staff. Duplicate Applications In the event an application is received by the vendor and it is identified as a ‘Duplicate’ as outlined by policy, a task is created and routed to the appropriate CCC or MEPD Region (#) queue for processing as outlined in V. Customer Care Center – Duplicate Applications. If a ‘Duplicate’ application is received in an eligibility office or outstationed facility, staff should follow the steps below: 1. Designated staff will access the State Create Task page and manually create a ‘Duplicate (Program) Application’ task and select the appropriate location they have access to from the Routing Location drop down menu. 2. Once the task is created for the appropriate eligibility office or outstationed facility, the worker will claim the task and process the duplicate application/redetermination appropriately. 3. Once the action is complete, the document will be routed to the vendor following the Image Only document process. Identical Applications If an application is received by the vendor and it is determined to be an ‘Identical’ application as defined by policy, the vendor will classify the document as an ‘Identical’ application and link it to the appropriate TIERS case. In addition, comments will be automatically added to TIERS Case Comments and a task will not be routed to the state. If an application is received by the eligibility office or outstationed facility and it is identified as an ‘Identical’ application as defined by policy, staff must write ‘Identical Application’ on the front page and route to the vendor following the Image Only document process. Client Reported Changes CCC and MEPD (CCCMEPD/MEPD Region (#) Change) staff are responsible for working most client reported changes from end-to-end. If a client reports a change directly to the staff without verification, the staff takes the change and enters it into the State PortalReport A TIERS Change portlet and the system will automatically create and route the change task appropriately. with verification, staff must complete a MI/Change Routing cover sheet and then fax it to the vendor at 1-877-236-4123. The system will create and route the change tasks appropriately. Note: Others may be responsible for processing a change if they are processing an application or redetermination action. 47 ES State Processes December 2013 Client Inquiries Clients may dial 2-1-1 for case status inquiries. Follow the same process regardless of the point of entry. Make an initial good faith effort to respond to the client no matter the point of entry. Vendor action for phoned, faxed or mailed inquiries: Check inquiry in TIERS. Check schedules through State Portal Scheduler search. Respond to the individual if the initial inquiry can be resolved. If the initial inquiry cannot be resolved, it may be routed to the centralized Special Escalation Unit (SEU) for the vendor to assist. The SEU staff views all the logs, all inquiry systems, case data entered, or comments documented. The SEU worker makes every possible attempt to respond to the inquiry. If the inquiry cannot be resolved, escalate it to the designated state escalation queue to provide assistance or use the escalate flag within TLM which flags the open TLM task. Eligibility Office (TIERS) staff action for walk in clients. Check inquiry in TIERS. Check schedules through State Portal Scheduler search. Complaints Complaints can be received from clients and Authorized Representatives via phone, fax or in person. These complaints can be received by vendor or Eligibility Office staff at any time. Complaints Received by ES Staff Complaints received at the Eligibility Offices are reviewed to determine if the complaint is for the receiving office. If the complaint is for the receiving office or another Eligibility Office, staff follows established procedures to resolve the complaint locally. These complaints are not routed to the vendor for resolution. If the complaint received is regarding the vendor and/or its staff, the Eligibility Office staff logs the complaint through the State Portal, using the Complaints Tab portlet. This complaint information will be routed to the vendor’s escalation unit for investigation/resolution. Complaints Received by Vendor Complaints received by the vendor will be entered into the State Portal Complaints portlet and they will attempt to resolve them. Complaints they are not able to resolve and therefore require escalation to the state, will be routed to the appropriate location through TLM. Vendor staff will manually create one of the following two TLM tasks below. 48 ES State Processes December 2013 A ‘Complaint for a TW Case’ TLM task for TW complaints will be routed to the following locations: Office (eligibility office based on client’s zip code) CCC ART WHP CBS-MTFCY Fair Hearings (TW and MEPD) FFCC CBS-FS-SSI CBS-FS-SNAP CBS-HC-FFCHE CMC CPC CBS-MBCC CBO CBS-RMA A ‘Complaint for a MEPD Case’ TLM task for MEPD complaints will to be routed to the CCC MEPD or the MEPD Region (#) Change TLM Global queue. Note: If MBI is included as a program, task will route to MBI Queue based on case zip code If MBIC is included as a program and MBI is not, task will route to MBIC Regional Queue based on case zip code Staff should follow their regional or local office procedures when processing and resolving complaints. Once the complaint is resolved, staff should mark the TLM task as ‘Complete’. Missing Information - No Anchor Task When clients submit missing information or postponed verification to the Eligibility Office, clerical staff date stamp and perform inquiry to determine if ownership of the MI is for a worker in that office or if there is an outstanding task associated to that case still in any other locations TLM Queue. If it is determined that the MI belongs to that office, the information is routed to the appropriate worker. Once the case is completed, the MI is sent in for Image Only. If it is determined there is no associated task for the information received, or if it is determined that the MI belongs to another office, it is faxed to the vendor at 1-877-236-4123. The vendor reviews all information received and documents the receipt of the information in TIERS Case Comments. Once the vendor classifies the information as Missing Information, the system will flag all open TLM tasks with an MI flag. If there are not any open TLM tasks, the system will determine if there are any active, pending, suspended or denied TIERS EDGs and determine the appropriate TLM task assignment and routing. Staff will need to review the information to determine the appropriate case action. 49 ES State Processes December 2013 If all TIERS EDGs are currently active, the system creates a ‘Change for a (Program) Case’ task to the CCC TLM Global Queue for processing. If there is a pending TIERS EDG(s), the system will create a ‘Missing Information for a (Program) Case’ task and assign and route the task to the individual who pended the EDG(s). If the system is not able to assign a TLM task to the individual who pended the EDG(s), a task will be routed to CCC or to the MEPD Regional queue as unassigned. If there is an EDG(s) that has been denied for failure to provide, the system will create a ‘Missing Information for a (Program) Case’ if the denial occurred within re-open policy timeframes. The system will automatically assign and route the task to the individual who denied the EDG(s) for failure to provide. If the system is not able to assign the TLM task to the individual who denied the EDG(s), the task will be routed to CCC or to the MEPD Regional queue as unassigned. Staff will be responsible for determining the appropriate action needed, if any, based on policy guidelines. This section outlines the process. Fair Hearings Requests Individuals may request a fair hearing in person, over the telephone, or in writing. If the request for a fair hearing is received in person or via telephone by state staff, the person who receives the request must: Contact the supervisor or worker in charge to speak with the client or Authorized Representative. Explain the action taken and the reason for the decision and, Inform the client of his/her rights. If the client still chooses to continue the fair hearing process: The worker/supervisor enters the fair hearing request in the State Portal Appeals tab in the Add New Appeal portlet. These entries will automatically create an ‘Appeal Request for (Program/TOA)’ for the ES-Centralized Representation Unit (ES-CRU) staff. The information entered into this section will be used by the ES-CRU for processing the request and completing the Form H4800 - Fair Hearing Request Summary. If HHSC staff receives fair hearing requests via fax or mail, staff follows established office processes for reviewing the action being appealed. If the client still chooses to appeal: The worker/supervisor faxes the appeal using the fair hearing cover sheet via the expedited fax line (1-866-559-9628) for processing. DO NOT complete and submit a Form H4800 or enter the fair hearing request in the State Portal. This information is used by specialized staff to process the fair hearing packet. 50 ES State Processes December 2013 Handling of Inappropriate Documents An inappropriate document is information provided by a client that is not related to a case and is deemed inappropriate in nature; such as threats, pornography etc. Documents may be received by mail, in person, or a client may upload a document via www.yourtexasbenefits.com . If an inappropriate document is linked electronically to a case, whether by vendor staff or via client upload, staff must send an email to OES_Vendor_OPS_Oversight@hhsc.state.tx.us and request the delinking of the information from the case. Staff should include a detailed description of the issue in the body of the e-mail and include the information below: Case Number MAXeIE App ID or DCN if it is related to an Application Registration task Staff should notify their supervisor and worker III, who in turn should report the incident to the Regional Director, regional officer and their Regional Administrative Services (RAS) representative. Additionally, any document regarding threats to HHS regional staff should mirror the enterprise Safety and Security for Regional/Local Offices policy number SSS/RAS-002 which can be found at: http://hhscx.hhsc.state.tx.us/Admin/ras/ServiceGuideForms/Safety%20_Security_v1_7.p df Disaster SNAP Processing In the event a major disaster is declared, clients not currently receiving SNAP can apply for assistance by submitting a Disaster SNAP Application to an Eligibility Office or application intake site in the impacted area or at identified satellite locations that are serving persons affected by the disaster. Eligibility Office – When a Disaster SNAP Application is received from the client at an Eligibility Office, staff accepts the application, conducts the interview, processes the request, and sends the application for imaging. Eligibility Office staff will receive detailed location(s) information from ES Management staff once the disaster is declared. Intake Site – When a Disaster SNAP Application is received from the client at an intake site, intake site staff conducts the interview, and ship the application to the DPC for imaging. Once imaged, a “Process a Disaster Application” task will be created automatically and routed to the Disaster Global queue for processing in TIERS by designated staff. If an eligibility office is overwhelmed by the volume of Disaster SNAP applicants, it may change the process to function as an intake site. SSP Account Management Clients must set up an SSP Case Visibility account in order to view case information and report changes by going through advanced authentication. If a client loses their SSP password or is unable to set up a case visibility account because they cannot correctly 51 ES State Processes December 2013 respond to the authentication security questions via the SSP, they may request assistance from HHSC or the vendor. Reason Alternate Account Set Up/Password Reset If the client is… In the office… Contacting the office by phone… Action Then, verify the client’s identity and use the State Portal SSP Account Management tab to grant case visibility access or password reset. Then, refer the client to 2-11 for assistance. Escalating Vendor Processing Issues In the event staff identifies issues related to vendor processing, they should escalate them to their supervisor or person acting in a supervisory capacity. Supervisory staff will be responsible for reviewing the issue to determine if further escalation is needed. If escalation is needed, supervisory staff should route the issue to the ES Vendor Operations staff at the e-mail address below: Mailbox Display Name: HHSC OES Vendor Operations Oversight E-mail address: OES_Vendor_Ops_Oversight@hhsc.state.tx.us The subject line should include the following information: Action Needed or Informational Identify error: Scheduling, Rescheduling, Imaging, etc. Region Example: Action Needed: Reschedule-Reg 7 Staff should include a detailed description of the issue in the body of the e-mail and include the information below. Case Number MAXeIE App ID or DCN if it is related to an Application Registration task. Automatically Routed Tasks Tasks automatically routed by the system are not considered vendor errors. If the system incorrectly creates a task during the auto-routing process, staff should follow regional escalation processes for additional clarification and guidance. The list below includes some forms that are automatically routed to the state queues: 1010R – Your Texas Works Benefits: Renewal Form 1014R – Children’s Medicaid Renewal Texas Women’s Health Program o 1831 – Adjunctive Eligibility Letter o 1867R – Texas Women's Health Program Medicaid Application 1840 – Recertification for SNAP Benefits 1842 – SNAP-CAP Renewal Application 52 ES State Processes December 2013 1869 – Renewal for Health Care Benefits (FFCHE) SSP Applications SSP Redeterminations SSP Changes MI/Change Routing Cover Sheet Note: The system routes the 1010R and 1014R to the benefit office or CMC queue based on the client’s residence zip code contained within TIERS. The queue that receives the task is responsible for processing the task. TIERS Alerts TIERS creates alerts for agency generated changes. Many of these alerts are converted automatically to TLM tasks and processed by CCC or other responsible area. There are still TIERS Alerts that staff are responsible for processing such as Second Level Reviews. Staff should continue to check their Welcome to TIERS home page daily, and ensure the TIERS Alerts are processed appropriately. TIERS Unavailable There are two different types of ‘TIERS unavailable’ cases. 1. TIERS Down When TIERS is completely unavailable, the application cannot be accessed. When TIERS is unavailable, it is unavailable statewide. TIERS access is unavailable; therefore TIERS specific data will be missing. The only complete dataset is in TIERS. Typically when TIERS is unavailable, the State Portal is still available and staff can access documents that have been imaged and appointments that have been scheduled. When TIERS is available in a read only mode, staff should be able retrieve a task from the Task List Manager (TLM) and read the TIERS Data Collection screens. TIERS cannot be updated when in read only mode. When TIERS is unavailable benefits may be issued on the web-based EBT system with appropriate approval. In order to issue benefits on the webbased EBT system, the client must complete a Form H1855 - Affidavit for Non-receipt or Destroyed Food Stamp Benefits. Expedited or timely benefits may be issued using the web-based EBT system. However, access is controlled by security measures, therefore only appropriate staff are to carry out these tasks with appropriate approval. 2. TIERS Read-Only When TIERS is in read-only mode, workers can access the TIERS application, but data cannot be entered or edited. Texas Health Steps Verification Process In some instances, state staff must obtain verification of compliance with Texas Health Steps. Below outlines the process. 53 Texas Works worker prepares and faxes Form H1087 to the vendor for processing. Staff faxes Form H1087 to 512-533-3867 or 512-533-3869. ES State Processes December 2013 The vendor obtains the verification, completes the form and returns the verification to the requestor. If the requestor is unknown/unclear, the vendor faxes the complete form to the appropriate Regional THSteps Liaison who will forward to the appropriate individual. TIERS Case Assignment All Texas Works EDGs need to be assigned to the TAAGeneric worker and transferred to the vendor office once a case is finished. This is done automatically by TIERS when the case is disposed. All MEPD staff has the ability to manually assign MEPD EDGs to a specific worker. If the MEPD EDG is not assigned to a specific MEPD worker, the system will automatically assign the EDG to the TAAGeneric worker upon disposition. TLM will only consider MEPD EDG assignments, when routing tasks to the MEPD Region Facilities queue for the programs listed below: TA12 TP10 TP15 TP16 TP17 ME - State Group Home ME – State School ME – Non-State Group Home ME – State Hospital ME – Nursing Facility If one of the above EDGs is assigned to an MEPD worker, the system will automatically assign the task to the EDG owner and it will display in their personal queue. If the EDG is assigned to the TAAGeneric worker or to someone who no longer is active in the system or has access to TLM, the task will be routed to the MEPD Region Facility TLM global as an unassigned task. All other TLM task for MEPD will be routed to the appropriate MEPD Region, MEPD Region Change queue based on case zip code regardless of TIERS case assignment. Reporting TIERS/State Portal Tickets When issues or problems arise in case processing through TIERS or the State Portal, staff calls in tickets to get the problem resolved. There are two levels of help desk staff that are available to assist. Level 1 – ES Technical Help Desk Level 1 staff can assist with the following items: 54 TIERS system resets (“user already logged in” message) TIERS password unlocks (“Account is locked for … Contact System Administrator” message) TIERS outages or system unavailability MAXe CHIP issues ES State Processes December 2013 To reach the ES Technical Help Desk, call (800) 214-4175 or (512)438-4720 and press option ‘1’ for assistance. The ES Technical Help Desk is staffed from 8:00 a.m. to 8:00 p.m. Central Standard Time, Monday through Friday. Non-urgent issues can also be reported to the ES Technical Help Desk by sending an email to: IEE_HELP@hhsc.state.tx.us. The e-mail must contain employee name, phone number, office location and description of the problem employee is experiencing. Level 2 – TIERS Help Desk Level 2 staff can assist with the following items: TIERS/Portal functionality questions TIERS/Portal software defects TIERS/Portal data entry errors that cannot be corrected within the TIERS application (Production Support Requests -PSRs) TIERS/Portal escalations EA TIERS Help Desk staff are responsible for requesting additional information and provide instructions/resolutions to End Users. When sending TIERS/Portal issues via e-mail to the EA TIERS Help Desk at Tiersapplicationsupport@hhsc.state.tx.us, staff must complete the TIERS Help Desk Issues Template. Escalation of TIERS Tickets Only tickets meeting the following criteria may be designated as "Escalated" and must be processed using special procedures. While all issues are important, escalated issues, by definition, have the potential to drastically impact our clients adversely. These criteria apply to both Texas Works (TW) and Medicaid Eligibility for the Elderly and Persons with Disabilities (MEPD). Priority 1: High level complaints (Legislative, Executive Commissioner, Ombudsman, etc.) Priority 2: Office level complaints Priority 3: Cases that are overdue and the resulting disposition would grant benefits Priority 4: Timeliness – resulting action would be certification of benefits and would meet timeliness Priority 5: Timeliness – resulting action would be denial and would meet timeliness; within this priority level – case due date will also be used Priority 6: Cases that are overdue and resulting disposition would be denial (unless complaint) Steps for Escalated Tickets Staff must take the following actions when escalating tickets: 1. Follow established procedures to obtain first level triage/help from a supervisor or designee. 55 ES State Processes December 2013 2. If the problem cannot be resolved and the issue is not policy-related, report the issue to the HHS Consolidated Help Desk and provide the information included in the template (Escalated Ticket Template – February 23, 2010). 3. Note: It is extremely important to provide as much information as possible in order to accurately diagnose the issue and provide timely resolution. 4. Document the Help Desk ticket number in “Case Comments” and do not make any additional changes to the case until instructed to do so by Help Desk staff. 5. When a solution has been received, staff must report results back to the Enterprise Applications (EA) TIERS Help Desk as soon as possible to ensure timely resolution. Help Desk staff will remain available to receive the results of the solution unless they were not able to contact the user initially to report the proposed solution. 6. If a user does not respond to e-mail and/or voice mail messages from the EA TIERS Help Desk staff on an escalated ticket, Help Desk staff have been instructed to contact the secondary contact listed on the ticket. 7. If the case is due and a solution has been provided, the user will be required to remain in the office until the case is disposed; may have to remain after close of business hours. 8. If no one is available to dispose the case, the user or supervisor must notify the EA TIERS Help Desk immediately. 9. If an escalated ticket has not been resolved within two days or more, then staff must follow the Elevated Escalated Ticket Procedures noted below. Elevated Escalated Tickets Procedures End User Action 1. Employees must ensure the original ticket was escalated to the EA TIERS Help Desk via phone or e-mail at IEE_Help@hhsc.state.tx.us 2. When it has been verified that the ticket was properly escalated, the user must provide the following information to their supervisor via e-mail with "Elevated Escalation Needed for <Ticket #>" in the subject line and use the established ticket escalation Excel document – (Escalated Ticket Template – February 2010): Employee location Region Worker name Case name Case number Ticket number Due date of case action Date ticket opened Date ticket escalated Date ticket closed without resolution (if applicable) Brief summary of the issue Escalation Criteria Supervisor Action 1. Verify the ticket was previously escalated to the EA TIERS Help Desk based on the escalation criteria. 56 ES State Processes December 2013 2. Ensure the employee provides the required Ticket Escalation documentation and that the information is complete. 3. Route the information via e-mail to the appropriate regional escalation contact(s) listed below: Region Point of Contact Phone Number Back Up Point of Contact Phone Number 1 Francis Pena 806-457-5231 Patrice Price 806-766-2728 2/9 Kathy Weber 325-866-7506 Melody Trimble 325-659-7650 3 Linda Autry 972-337-6147 Sherry Pressnell 972-337-6241 4 Robert Heflin 903-927-0227 Bob Kupke 903-581-9243 5 Steve Allison 936 544-3850 x224 Bonita Gosey 409-423-7551 6 Margaret Boehme 713-767-2443 Jackie Ross 713-696-3679 7 Melba Hills 512-897-7940 Sandra Dillett 512-788-4397 8 Dee Ann Smith 210-619-8260 David Garcia 210-619-8030 10 Kate Hill 915-759-3477 Mary Tovar 915-872-5901 11 Henry Howell, Jr. 956-316-8143 Juan Gonzalez 956-316-8274 CCC Craig Pauler 512-533-3655 Sandy Holguin 210-304-5719 MEPD Martha Meazell 254-629-1713 x3077 Sally Lopez 830-426-7543 ART Willann Thomas 979-776-7417 Bill Brown 281-597-5214 Escalation Contact Action 1. Verify the ticket meets the escalation criteria. 2. Verify the employee/supervisor provided all the necessary information noted previously. 3. Route the information to Enterprise Application contacts for investigation. 4. Monitor escalated tickets to ensure resolution and escalate any unresolved issues to regional management. EA Help Desk Action 1. EA TIERS Help Desk employees ensure ticket resolution and response is provided to the user, their supervisor, and the escalation point of contact as soon as possible. 2. The TIERS vendor is required to respond to escalation requests within 48 hours. Help Desk Contact and Hours of Operation Contact the HHS Consolidated Help Desk at (800) 214-4175 (option “1”) from 8:00 am to 8:00 pm Central Standard Time (CST) or email tiersapplicationsupport@hhsc.state.tx.us. This is the TIERS Application Support mailbox in Outlook. The mailbox is monitored until 7:00 pm CST on workdays until 3:00 pm CST on Saturdays. Help Desk Ticket Processing Issues Staff should apply the process below when encountering issues related to the processing of Help Desk tickets. Help Desk ticket processing issues include, but are not limited to, the following: 57 ES State Processes December 2013 Tickets closed without resolution Pressing issues not addressed in a timely manner Tickets for which inaccurate or insufficient information is given, etc. Escalation Process If a Help Desk processing issue is encountered, follow the steps below. 1. Staff member escalates the issue to their supervisor or person acting in a supervisory capacity. 2. Supervisory staff reviews the issue to determine if further escalation is needed. 3. If escalation is needed, supervisory staff routes the issue to the Enterprise Applications staff at the email address below: Mailbox Display Name: HHSC EA Business Automation E-mail address: EA_BusinessAutomation@hhsc.state.tx.us Email Format The subject line of the email should include the following: Action Needed or Informational Help Desk ticket number Identify issue: Closed but not resolved, Not addressed timely, Inaccurate information, etc. Example: Action Needed: Ticket #1426921, Closed but not resolved The body of the email should include the following: Region Case Number Detailed description of the issue User ID and contact information of the worker experiencing the issue Data Broker Resolution All Data Broker issues need to be escalated to the state Data Broker Coordinator via the Regional Data Broker Coordinator to determine the best solution resolving the issue. The Regional Data Broker Coordinator e-mails the information gathered to the state Data Broker Coordinator, Laurie Hoelscher at laurie.hoelscher@hhsc.state.tx.us, who will jointly resolve the issue with Dallas Computer Systems (DCS). The regional coordinator is notified via e-mail when the issue is resolved. All Regional Data Broker Coordinators will receive notification on significant issues and be instructed to inform their regional users of these issues. Regional users DO NOT need call the Help Desk to report known problem issues that are in the process of resolution. Note: DCS is not to be contacted directly by regional users or Regional Data Broker Coordinators. Task Failure Processing In some instances, the system is unable to determine which queue to route certain tasks such as Application Registration or Schedule Appointment tasks because the client’s zip code is not mapped to a location. The system will create and route a ‘Process a TLM Task Failure’ to the Task Failure location when this occurs, Designated staff will be responsible for reviewing the information to determine the reason for the task failure. 58 ES State Processes December 2013 Out-of-State Zip Code If the client’s zip code was an out of state zip code, they will process the action as an Out of State application in TIERS. Once processed, the staff will mark the task as ‘Complete’. Incorrect Zip Code Entry If the client entered an incorrect zip code and the client’s correct zip code is currently mapped to an office, the staff will determine the correct zip code and enter the new zip code information on the address screen when performing application registration. Using the correct zip code will ensure the task is routed to the appropriate queue based on the client’s zip code and program(s) requested. Once processed, the staff will mark the task as ‘Complete’. Zip Code Not Mapped If the client’s zip code was correct but had not been mapped to an office, they will mark the task as ‘Update Zip Code’. This will create a ‘Process a Zip Code Update’ task to be processed by designated State Office staff. The designated State Office will: Claim the ‘Process a Zip Code Update’ task. Work with the region and update the Office Locator appropriately. Once the Office Locator is updated, staff will register the application in TIERS so the process task is created and routed to the appropriate queue based on the client’s zip code and program(s) requested. Once the appropriate task is created, they will mark the ‘Process a Zip Code Update’ task as ‘Complete’. 59 ES State Processes December 2013 XVI. SUPPORT TOOLS The State Processes document contains specific instructions and also refers to several Support Tools for ease of use and quick reference. Use both documents to ensure proper processes are followed. Below is a brief overview of each Support Tool. The TIERS Help Desk Issues Template should also be used when sending TIERS issues to Level 2 TIERS Help Desk staff. Also, if additional information is needed; other Reference Guides and Job Aids may be accessed from the OFS website at: http://ofs.hhsc.state.tx.us/TAC/ESASK_Materials.aspx . This information is provided by the Enterprise Applications Application Support and Knowledge (ASK) team and it can be viewed online, saved in Favorites or to your desktop, or printed for future reference. Document Routing Procedures This Support Tool communicates the procedures for scheduling and routing documents for TIERS clients in TIERS Eligibility Offices. Most documents will be processed in the Eligibility Office from end-to-end. Complete Action and Disposition Coordination This Support Tools provides staff with expectations regarding Complete Action processing and disposition coordination. Document Upload This Support Tools provides staff with information on how clients can upload verifications to yourtexasbenefits.com from their home computer or other external location. The document upload functionality cannot be performed on the HHSC lobby computers. It also includes basic system operating requirements needed for this activity. First Time Sign-On Procedure for State Portal This Support Tool walks first time users through signing in to the State Portal. Users will have to change the default password. Ordering ES Materials This support tool provides an overview of the process through eligibility staff will order and receive new eligibility system/ES envelopes, applications and forms. Re-Linking Images This Support Tool instructs users on how to re-link imaged documents in the State Portal to the correct TIERS case. 60 ES State Processes December 2013 State Portal Supervisor This Support Tool assists Supervisors in performing managerial functions using the State Portal. It includes instructions on how to publish, update, and view office schedules, and will aid in managing and monitoring workloads. State Portal TLM This Support Tool aids workers in using the State Portal to manage daily workloads. It assists users in effectively navigating in the Task List Manager. TIERS/Portal Security Roles – MOR Workload Transfer This Support Tool provides information on steps needed to handle TIERS and Portal Security Roles when an individual is resigning from HHSC or moving to a new TIERS location. Staff must following these steps as well as complete the MOR Workload Transfer Sheet and Form 4743A appropriately. Escalated Ticket Template This document is used to provide detailed information regarding TIERS/Portal ticket information. Self Service Portal Application Registration This document serves as a quick reference for staff responsible for performing Application Registration for applications submitted via SSP. Reminders This document provides information on the steps client’s follow if they wish to sign up for electronic reminders. 61 ES State Processes December 2013 XVII. GLOSSARY OF TERMS Term Application Support (AS) Area Information Centers (AIC) Assistance Response Team (ART) Automated System for Office of Inspector General (ASOIG) Budgeted Job Number (BJN) Central Processing Center (CPC) Centralized Benefit Services (CBS) Children’s Medicaid Center (CMC) Community Based Alternatives (CBA) Community Based Organizations (CBO) Community Partners (CP) Contingency Processing Method (CPM) Customer Care Centers (CCC) 62 Description Vendor employee’s who link scanned or faxed images to TIERS cases, reschedule appointments, review verification documents and route work to state staff. Available via 2-1-1, their primary purpose is to maintain information about human service resources in the community and to link people who need assistance with appropriate service providers. In Texas, this service is provided through certified staff at twenty-five contracted Area Information Centers. State staff responsible for assisting other regions. The automation system that distributes Income and Eligibility Verification System (IEVS) data matches and Interstate matches to OIG and MEPD staff to clear and create overpayment referrals in the ASOIG Investigations module. Overpayment and fraud referrals are entered into ASOIG or transmitted through an interface from TIERS. The system allows users to track referrals, manage investigations, and establish overpayment claims through an interface to the Accounts Receivable Tracking System (ARTS). A unique set of numbers for an employee that identifies the particular location and budget the employee’s position is assigned to. Centralized staff responsible for processing TIERS CHIP to Medicaid referrals that are received from the CHIP vendor. They also process emergency Medicaid benefits for CHIP perinatal mothers. Centralized staff responsible for processing statewide applications/redeterminations for FS-SSI, MTFCY, HC-FFCHE, RMA, SNAP, TYC/JPC youth and MBCC. Centralized regional staff responsible for processing Children’s Medicaid applications and renewals for designated region(s). Provides a wide variety of home and community-based services to the elderly and persons with disabilities as cost-effective alternatives to institutional care in nursing facilities. Approved organizations that connect individuals in need with services available in their communities or provide a service directly. Organizations that operate at the local level to provide services and assistance to community members in need. They also applicants filing for benefits and authorized contracted Partners may perform SNAP interviews. These organizations are also called Community Based Organizations (CBOs). An alternate method of processing cases when there are outstanding system issues. Customer Care Center (CCC) is a virtual region located in six cities across the state. They are located in Athens, Austin, El Paso, Houston, Midland and San Antonio. CCC also includes a variety of centralized areas, including CCC Core, Central Processing Center (CPC), Centralized Benefit Services (CBS) and Texas Women’s Health Program (TWHP). ES State Processes Term Customer Care Representatives (CCR) Dallas Computer System (DCS) Data Integrity (DI) Document Imaging Document Processing Center (DPC) Drug and Alcohol Treatment Facility (D&A) Eligibility Services Staff (ES) Eligibility Support (ES) ES-Centralized Representation Unit (ES-CRU) Former Foster Care Children (FFCC) HHSC Eligibility Office Health Care for Former Foster Care in Higher Education (HCFFCHE) Income and Eligibility Verification System (IEVS) In-Flight Queue MAXe IE Medicaid Buy-In (MBI) Medicaid Buy-In for Children (MBIC) Medicaid for Breast and Cervical Cancer (MBCC) 63 December 2013 Description Vendor employees who provide clients with an overview of eligibility programs and services, answer application and eligibility questions, take changes and assist with screening and application completion. Vendor who provides data broker information to the state. Specialized unit within ES that processes ME SSI Medicaid, Medicaid for newborns, Biographical corrections, Spend-Down, Merges/Separates, Buy-In, QI-1 and Managed Care corrections. Process of scanning documents and saving them as electronic files in the new eligibility system for online access and viewing. Located in Midland, vendor staff in this facility receive, process, and image all inbound documents. Facility that provides treatment for alcohol and chemical dependency. Staff is individuals who provide eligibility determination services as part of their primary job responsibilities. This includes Texas Works and MEPD staff. Process of integrating the application and eligibility determination for applicants seeking assistance with Medicaid, Food Stamps, TANF and MEPD services. Staff who process fair hearing packets and serve as the agency representative for most fair hearings. Type of assistance under ACA that covers former foster care children up to age 26 who were receiving federally funded Medicaid when they aged out of Foster Care. Full-service offices where HHSC staff use TIERS to provide eligibility determination and benefit issuance services. (Previously known as “local offices” or “field offices”) A program to provide health coverage to an individual who: Is at least 21 years of age plus one month, through the month of their 23rd birthday; must have been in Foster Care on their 18th birthday; is enrolled in an institution of higher education in Texas. An automated system that matches various types of benefits and income with other state and federal agencies. (Ex: wages, unemployment compensation, special benefits, SSA and SSI benefits, and IRS records of unearned income) A view displaying details of the task being worked including any outstanding tasks associated with the case. The database that the vendor uses to collect, process and store data. The MBI program allows people of any age who have a disability and who are working to receive Medicaid by paying a monthly premium. The program is worked solely in TIERS by MEPD staff. The MBIC program allows children up to age who have a disability and with gross family income of up to 300% FPL to receive Medicaid by paying a monthly premium. The program is worked solely in TIERS by MEPD staff. A special Medicaid program authorized by federal and state laws to provide access to cancer treatment services for qualified women. ES State Processes Term Medicaid for Pregnant Women (TP40) Medicaid for Transitioning Foster Care Youth (MTFCY) Missing Information (MI) Office of the Attorney General (OAG) Outstationed Workers Process Redeterminations Refugee Medical Assistance (RMA) Refugee Voluntary Agency (VolAg) Request for Review (RFR) Service Authorization System (SAS) Simplified Nutritional Assistance Program (SNAP) Social Security Administration (SSA) Special Escalation Unit (SEU) State Portal (STP) 64 December 2013 Description Medicaid coverage for pregnant women to assist in the prenatal care and birth of the child. Coverage is received two months following the birth of the child. Medical coverage for youths aging out of foster care. The Texas Department of Family and Protective Services (DFPS) administers the foster care program. Youths who age out of foster care may receive Medicaid from age 18 through the month of their 21st birthday if they meet all of the eligibility criteria. Incomplete or missing information needed to complete an eligibility determination. (Previously known as “pending information”) Serves as legal counsel to all boards and agencies of state government, issues legal opinions when requested by the Governor, heads of state agencies and other officials and agencies as provided by Texas statutes, sits as an ex-officio member of state committees and commissions, and defends challenges to state laws and suits against both state agencies and individual employees of the State. HHSC workers located at hospitals, clinics, or nursing facilities who determine eligibility for applicants in these facilities. Some of the outstationed workers are also housed in the Eligibility Offices. A defined set of steps/procedures for completing common agency tasks. Term used to define applications submitted to renew/review all program certifications. The Refugee Medical Assistance (RMA) program is100% federally funded. RMA program provides medical assistance to refugees who have lived in the United States for eight months or less from the date of entry. An agency that contracts with the U.S. Department of State to help the refugee/entrant with basic needs for up to 90 days. As a rule, every refugee/entrant is represented by a VolAg. A process by which a FFCHE or CHIP client who disagrees with the results of their case processing may formally request in writing that the results be reviewed. This is a part of the payment system for the Department of Aging and Disability Services (DADS) and MEPD providers. A six-year demonstration project that outreaches elderly SSI recipients who are not currently certified for Food Stamps. Aka SNAP-CAP Is an independent agency of the United States government that manages the United States' social insurance program, consisting of retirement, disability, and survivor’s benefits. Specialized vendor staff assigned to investigate issues that cannot be resolved at a lower level. These issues may include but are not limited to complaints, scheduling and interview errors, and phone calls from clients needing assistance. A single sign-on application where HHSC staff initiate tasks or work assignments, launch TIERS, view images and schedules, record complaints/ requests for fair hearings and perform other activities related to eligibility determination. ES State Processes Term Task Task List Manager (TLM) Task List Manager (TLM) Global Queue 65 December 2013 Description An eligibility related work item that is sent to state staff via the State Portal and visible in the TLM Global Queue or TLM Personal Queue. An online software application that lists tasks for state staff in Eligibility Offices, ART, MEPD and CCC. Staff selects tasks based on workload availability or assignment. The TLM Global Queue and TLM Personal Queue are used to receive and monitor activities and due dates. The user role determines the tasks staff can view. A list of tasks that may be claimed based on user roles and location.