Amendment to protocol for managing type 2 diabetes post gastric
advertisement

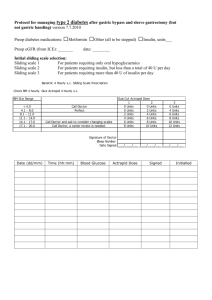
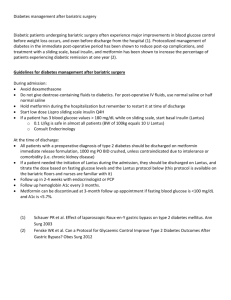
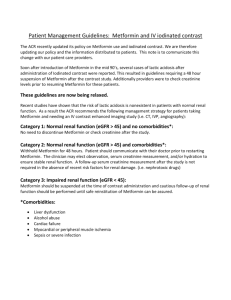
Protocol for managing type 1 diabetes or ketone prone type 2 diabetes after gastric bypass and sleeve gastrectomy (but not gastric banding) Preop diabetes medications: □Metformin □Other (all to be stopped) □Insulin, units___ Preop eGFR (from ICE): _______ date: ________ Initial sliding scale: First 20-24 hours after operation: standard Imperial College intravenous sliding scale Subsequent insulin sliding scale selection: Sliding scale 1 For patients requiring only oral hypoglycaemics Sliding scale 2 For patients requiring insulin, but less than a total of 40 U per day Sliding scale 3 For patients requiring more than 40 U of insulin per day Bariatric 4 Hourly s.c. Sliding Scale Prescription Check BM 4 hourly. Give Actrapid 4 hourly s.c. BM Stix Range < 4.0 4.1 - 8.0 8.1 - 11.0 11.1 - 14.0 14.1 - 17.0 17.1 - 20.0 Call Doctor Perfect Call Doctor and ask to consider changing scales Call Doctor, a senior review is needed. Sub.Cut Actrapid Dose 1 2 0 Units 0 Units 0 Units 2 Units 2 Units 4 Units 4 Units 6 Units 6 Units 8 Units 8 Units 10 Units Signature of Doctor Bleep Number Date Signed ___/____/___ Date (dd/mm) Admission Time (hh:mm) Blood Glucose Actrapid Dose ___/____/___ Signed 3 0 Units 4 Units 6 Units 8 Units 10 Units 12 Units ___/____/___ Initialled All diabetic patients to have latest eGFR (with date) documented in notes on admission Day of surgery/ drugs Start intravenous sliding scale immediately pre-op and stop all oral hypoglycaemic Inform diabetes team Diabetes team to manage fluid and insulin in consultation with surgical team Continue same dose of Glargine or Detemir that patient took pre surgery Postop. day 1 Diabetes team to review and to switch patient to sub cut sliding scale Continue same dose of Glargine or Detemir that patient took pre surgery Two hourly glucose measurements Check blood ketones if glucose >14mmol/L Call diabetes team if glucose <4 or >10 mmol/L Postop. day 2 Diabetes team to review Continue same dose of Glargine or Detemir that patient took pre surgery Give short acting insulin with meals as 1 Unit for every 15g of protein Prescribe Metformin at the same dose as on admission (which in most cases should be 1g twice daily unless poor tolerability) starting the evening 2 days after surgery, unless the latest eGFR is <60mL/min. For these patients, contact obesity physician Discharge 1. No patient to be discharged if last BM >10 mmol/L 2 All diabetic patients to text “Blood glucose mobile phone” (07970719453) with fasting glucose value for 10 days immediately after surgery. If patient does not text before 12:00, the team will contact them Metformin dosage selection: 1. All patients will be restarted on their usual metformin dose (usually metformin 1g twice daily) starting 2 days following surgery, provided that eGFR>60mL/min. Metformin will be started on the second postoperative evening (eg if operation on Tuesday then start metformin on Thursday evening). Patients who can’t tolerate metformin should be reviewed by clinician/nurse specialist. 2. Metformin doses if eGFR <60 ml/min: a. eGFR 45-60 ml/min: All patients will be prescribed metformin 850mg twice daily starting 2 days after surgery. Metformin will be started on the second postoperative evening (eg if operation on Tuesday then start metformin on Thursday evening). b. eGFR 30-45 ml/min: All patients will be prescribed metformin 500mg twice daily starting 4 days after surgery. Metformin will be started on the fourth postoperative evening (eg if operation on Tuesday then start metformin on Saturday evening). c. eGFR < 30ml/min: no metformin to be given. 3. If patients can’t tolerate metformin then continue with insulin therapies alone. After discharge: Daily insulin requirement will be adjusted by 2 to 4 units to achieve a fasting blood glucose of 5.6-7mmol/l. 1. At Day 10 post op clinic review a. Metformin dose at discharge will be continued. b. If FPG is >7mmol/l, increase short acting insulin doses to 1 unit for every 10g of carbohydrate 2. At 3 months, all diabetic patients will be reviewed and hypoglycaemic medication adjusted 3. At 6 months, all diabetic patients will be reviewed by phone and those with HbA1c >7% will be brought back to the diabetes clinic for review of hypoglycaemic medication.