Bariatric surgery and BG mgmt
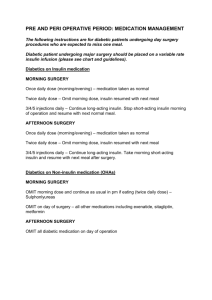
advertisement

Diabetes management after bariatric surgery Diabetic patients undergoing bariatric surgery often experience major improvements in blood glucose control before weight loss occurs, and even before discharge from the hospital (1). Protocolized management of diabetes in the immediate post-operative period has been shown to reduce post-op complications, and treatment with a sliding scale, basal insulin, and metformin has been shown to increase the percentage of patients experiencing diabetic remission at one year (2). Guidelines for diabetes management after bariatric surgery During admission: Avoid dexamethasone Do not give dextrose-containing fluids to diabetics. For post-operative IV fluids, use normal saline or half normal saline Hold metformin during the hospitalization but remember to restart it at time of discharge Start low dose Lispro sliding scale insulin Q4H If a patient has 3 blood glucose values > 180 mg/dL while on sliding scale, start basal insulin (Lantus) o 0.1 U/kg is safe in almost all patients (BW of 100kg equals 10 U Lantus) o Consult Endocrinology At the time of discharge: All patients with a preoperative diagnosis of type 2 diabetes should be discharged on metformin immediate release formulation, 1000 mg PO BID crushed, unless contraindicated due to intolerance or comorbidity (i.e. chronic kidney disease) If a patient needed the initiation of Lantus during the admission, they should be discharged on Lantus, and titrate the dose based on fasting glucose levels and the Lantus protocol below (this protocol is available on the bariatric floors and nurses are familiar with it) Follow up in 2-4 weeks with endocrinologist or PCP Follow up hemoglobin A1c every 3 months. Metformin can be discontinued at 3-month follow up appointment if fasting blood glucose is <100 mg/dL and A1c is <5.7%. (1) (2) Schauer PR et al. Effect of laparoscopic Roux-en-Y gastric bypass on type 2 diabetes mellitus. Ann Surg 2003 Fenske WK et al. Can a Protocol for Glycaemic Control Improve Type 2 Diabetes Outcomes After Gastric Bypass? Obes Surg 2012 Lantus/Levemir Insulin Adjustment (BARIATRIC) Insulin Dose Scale: After surgery discharge instructions: Check fasting AM blood sugar after waking, before eating or drinking anything and write down on “Sugar and Insulin Log” Determine insulin dose based on the “Insulin Dose Scale” and write dose down on “Sugar and Insulin Log” Insulin should be given at the same time everyday Follow up in 2-6 weeks with Dr. Rometo at the Falk Diabetes Clinic. Schedule by calling 412-5869780 Have glucose tablets on hand in case of low blood sugar <70. Take 4 and retest in 15 minutes Call the Falk Diabetes Clinic with questions/concerns, or diabetic supply needs at 412-586-9700 If fasting AM blood sugar is >220 180-220 144-179 120-143 100-119 81-99 72-80 <72 Adjustment compared to dose given YESTERDAY Increase by 6 units Increase by 4 units Increase by 2 units Increase by 1 unit No change. Take YESTERDAY’S dose Decrease by 2 units Decrease by 4 units Decrease by 6 units Starting dose of insulin: ___units Sugar and Insulin Log: Date Fasting AM Blood Sugar (before you eat or drink) Sunday Monday Tuesday Wednesday Thursday Friday Saturday Sunday Monday Tuesday Wednesday Thursday Friday Saturday Insulin dose for today (adjust from yesterday’s dose based on fasting AM blood sugar)