Oral Hypoglycemic Agents in Pregnancy
advertisement

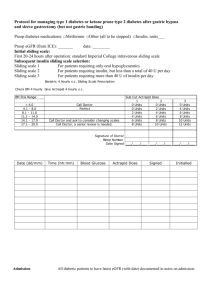
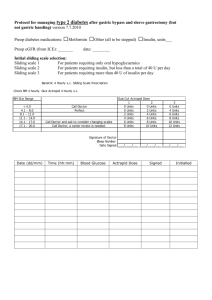
Oral Hypoglycemic Agents in Pregnancy Nafisa Dajani, M.D Department of Obstetrics and Gynecology Maternal Fetal Medicine Division University of Arkansas for Medical Sciences Feb 2005 History of Oral Hypoglycemic agents in obstetrics • First generation sulfonylurea (e.g. chlorpropramide,tolbutamide)became available in 1955 • Second generation sulfonylurea (e.g. glypizide, glyburide) introduced in 1984 • Why do we still not know what to do in 2005 Oral hypoglycemics • Several initial reports with the first generation oral hypoglycemic agents associated with congenital malformations, hyperbilirubinemia, neonatal hypoglycemia, polycythemia and neural tube defects both in vitro mouse model and in limited observational studies in humans Oral Antidiabetic Agents Sulfonyl ureas Generic Glyburide name Glipizide Chlopropr. Tolbutam. Glimepride Action Incr. pancreatic insulin secretion chronically Biguanides Alpha Glucosida se inhibitors Metformin Acarbose Miglitol Thiazolidi Meglitini nediones des Rosiglitaz one Pioglitazo ne Repaglin ide Nateglini de Dec.HGP Dec. PIR Dec. IG absorption DEC.PIR Incr. Glucose disposal Dec HGP Incr.pan creatic insulin acutely Delays PP CHO digestion & IG absorption Sulfonyl ureas • Stimulate secretion of insulin from the pancreatic beta cells Glyburide • Sulfonylurea • Enhance insulin sensitivity in peripheral tissue • Reduces glucose output from the liver • Insulin increases 15-60 minutes after injestion, peaks in 2-4 hours ,duration is <24 hours, elimination half life 5-16 hours Glyburide- cont’d • Adverse effects: headache, dizziness, pruritis, rash, photosensitivity, hypoglycemia, hyponatremia, nausea, hepatitis, arthralgia, blurred vision, aplastic anemia and agranulocytosis • 2.5-5mg initial, increase by 2.5mg q week to a maximum of 20 mg/day after 11 weeks gestation • Crosses the placenta in negligible amounts due to high protein binding and short half life Comparison Of Glyburide and insulin in women with GDM • RCT • N=404 • Randomized between 11-33 weeks • Singleton, FBS 95-140 ( OGTT ) • No difference in the LGA (12%), hypoglycemia ,NICU admission and congenital anomalies • Failure rate 4%-needed insulin Glyburide • Glyburide was not detected in cord serum • The study did not evaluate first trimester use • Did not evaluate use in type 2 diabetics • Did not evaluate other hypoglycemics Langer NEJM2000oct19;343(16):1134-8 Other glyburide study • N=197 , beyond the first trimester, diet • 124 responded to diet, 73 glyburide • 81% satisfactory control, 75% required 7.5mg/day or less. • 19% macrosomic infants • 11% side effects Kremer,AJOG2004may;190(5):1438-9 Does stimulation of beta cells eventually lead to pancreatic cell failure ? Does the use of sulfonylureas eventually lead to Type 2 DM? Metformin • Biguanid • Decreased hepatic glucose production, decreased glucose intestinal absorption, increased peripheral utilization • maximum effect may take 2 weeks • Dose: starting 500 mg daily up to max 2550mg/day Metformin –2 • Most common side effects are gastrointestinal, the potentially lethal side effect is lactic acidosis. Contraindicated in patients with renal failure and should be avoided in patients with liver dysfunction or excessive alcohol intake. Avoid in situations leading to hypoxemia such as CHF • Crosses the placenta. Negligible protein binding Metformin-3 • Metformin concentrates in the jejunal and ileal wall 10x higher than liver and 60x higher than muscle or fat. These high concentrations can result in anaerobic metabolism of glucose and release of lactic acidosis into the portal vein • Vitamin B12 defficiencey 10-30% with >3month treatment duration • B12, folic acid and other micronutrient defficiencies may have serious perinatal effects Why is Metformin attractive? • Cellular uptake of glucose is the primary • • mechanism , therefore hypoglycemia is not a side effect Fortunately the cellular uptake of glucose does not appear to occur in the placenta (Elliott and langer 1997) Unfortunately because of its low protein binding and low molecular weight it partially crosses to the fetus Classified as category B, with no anomalies in animals, however it did cause a delay in neural tube closure or growth in mouse embryos that was overcome with continued growth. Are there fetal implications for micronutrient deficiencies of B12, folic acid , iron and calcium that may occur with metformin use ? Experience with Metformin • South Africa has used metformin for 30 years • with no bad effects, the reports are small however . Australia have been using metformin for years also, no reported bad effects however no good studies either. The first RCT has been initiated in Australia MiG trial aiming to recruit 750 patients S. Afr. Med. J 56,467(1979) MJA vol180 3 may 2004 The Australian DIP Group • Metformin is not to be used routinely in women • • • with pregnancies complicated by diabetes ( type 2, or GDM ) When benefits from metformin therapy outweigh the risks e.g. patient refusing insulin, or requiring large doses of insulin, then its use may be appropriate Diabetics conceiving on metformin: discuss risk and options for other therapies, do not discontinue metformin until other treatments are started, reassure patient no teratogenesis No comment On PCO and first trimester use MJA 3may2004 volume 180,number9 ACOG cautions against Metformin Use Metformin and PCOS Systematic review • Cochrane systematic review confirmed that metformin increases the ovulation rate by a factor of 3.9 and the pregnancy rate by 3.3 • Combined with clomide it improves ovulation and the pregnancy rate by a factor of 6.7 • The evidence of metformin in decreasing miscarriage rate is weak and based on few observational studies. Cochrane review issue 3 2003,BMJ oct25 2003 Metformin and PCOS-Systematic Review • Associated with nausea, vomiting • • • • ,gastrointestinal disturbances, vitamin B12 deficiency No literature about the safety of long term use in young women with PCO Safety in the first trimester needs further evaluation, does not appear teratogenic No evidence it reduces BMI Equal or better ovulation rate has been reported by using lifestyle changes to achieve weight loss Should Insulin Sensitizing Drugs be used for women with Type2 or GDM • No randomized control trial available. there are only small pilot studies of 30-40 patients • All the available published data are of small number and the results are all reassuring EXCEPT for one study Cohort Study type 2 pregnant 50 metformin 68 sulfonyl ureas 42 insulin Preeclampsia 32%,7%,10% Perinatal mortality 11.65%,1.3% Criticism: Not blinded, not well controlled ,death cannot be attributed to metformin Hellmuth,Diabetic med July 2000,17 ;507-511 Should metformin be used prophylactically to decrease the incidence of GDM in PCOS • Most ,but not all studies agree that the incidence of GDM is higher in PCOS than in healthy women (20%-40%) • No RCT to date that metformin decreases the incidence of gestational diabetes • The evidence available comes from cohort, non randomized non blinded small pilot studies GDM and PCOS • Cohort study n=33 pts with PCOS conceived and continued metformin, vs a historical control that included the 33 patients in their prior pregnancy total n=72 control • Conclusion: 10 fold reduction in GDM from 31-3% Glueck,fertilitysterility77(3)march2002 520-525 Are there any adverse effects on the newborn? Neonatal Outcome • 122 live births to 109 patients with PCOS • Conceived on and continued metformin throughout pregnancy • Prospective evaluation of infants for 18 months , with historic controls • No difference in height, weight or motor development scores Glueck, human reprod June 200419(6):1323-30 Are there other insulin sensitizers ? Troglitazone withdrawn due to liver toxicity, had a dose dependent effect on ovulation in a large RCT Rosiglitazone and pioglitazone have been tried in PCOS but are not advisable in pregnancy due to lack of safety data and their long lasting effects Alpha glucosidase inhibitors • Acarbose • Inhibits intestinal alpha glugosidase,increased starch reaches the colon, ,the colonic flora will produce increasedbutyrate, which can upregulate prostaglandin E series production. Lobor inducing potential of PG E . To be avoided in pregnancy until safety data is available On study published from Mexico describing six pregnancies with GDM . All fasting and post prandials were normalized. All newborns were normal. Intestinal discomfort persisted throughout the whole pregnancy Ginecologia y obstetrica de mexico 68:42-5 2000jan RCT of adequate power are urgently needed to establish safety of oral hypoglycemics use in pregnancy.