Blood - SuddenLink
advertisement

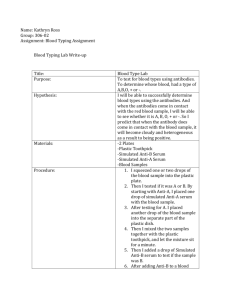
Blood Erythrocyte transports oxygen Basophil 0.5-1% WBCs; inflammatory & allergic rxns Eosinophil 2-4% WBCs; anti-helminth and phagocytic actions Lymphocyte 20-25% WBCs; specific immune rxns, B & T cells Monocyte 3-8% WBCs; becomes macrophage phagocytic activity Neutrophil 60-70% WBCs; major phagocyte antibacterial defenses Characteristics of Blood: A. Temperature: approx. 38oC B. pH: 7.35-7.45 C. Ave. Volume: 5-6 liters (11 pints) D. Amount/Body Weight: 8% of body weight E. Composition: 1. 55% Liquid portion 2. 45% Formed elements Soluble Components of Blood: A. Serum (liquid portion without clotting factors) B. Plasma (liquid portion + clotting factors) 1. Plasma contains many sorts of proteins including albumins, globulins, clotting factors, complement, regulatory enzymes, as well as electrolytes and hormones. 2. Albumins: most abundant plasma proteins; carriers for many molecules (sterols, bilirubin, hormones, ions...) 3. Globulins: many different types of proteins including immunoglobulins and... a. alpha1-anti-trypsin (AAT): major globulin; inactivates proteases; important in counteracting endogenous proteolytic activity such as during coagulation, inflammation; AAT-deficency associated with emphysema and liver disease; b. Haptoglobulin: binds free hemaglobin from lysed RBCs; increases under stress, acute inflammation, infections; decreases with massive hemolysis, burns, transfusion mismatches c. Transferrin: binds free Fe3+, transports in blood, III. Blood cells (Formed Elements): All blood cells are produced in red bone marrow A. Erythrocytes: produce about 2.5 million/sec; 120 day lifespan 1. Reticulocytes: immature RBCs (>1%) 2. Hematocrit = % RBC in blood (volume); male = 40-54%; female = 38-46% 3. Anemia: decreased hematocrit; many forms and causes: a. Iron-deficiency anemia: most common, inadequate iron absorption or excessive excretion b. Pernicious anemia: lack of intrinsic factor needed for B12 absorption c. Hemolytic anemia: destruction of RBCs leaving "ghosts" d. Thalassemia: inherited form of hemolytic anemia - altered form of Hb e. Aplastic anemia: loss of erythropoesis in red bone marrow f. Sickle-cell anemia: misshapen RBCs from altered Hb causes poor vascular circulation and hemolysis E. Polycythemia: increased hematocrit (over 65%); may be spurious or secondary to renal disease F. Erythropoetin: hormone to stimulate RBC synthesis; given to counteract bone marrow deficits (chemoth.) G. Erythrocyte and Hemoglobin (Hb) Production and Recycling: 1. Spleen, liver, red bone marrow - macrophage phagocytize damaged/dead RBCs; globin & heme are separated; globin digested & amino acids recycled; 2. The Fate of Heme... > a. Fe3+ separated from heme ---> biliverdin ---> bilirubin ---> into blood to liver b. bilirubin added to bile into small intestine... c. bilirubin ---> urobilinogen in lrg int. ---> into kidney (excreted as urobilin) or lrg int. (excreted as stercobilin) 3. The Recycling of Fe3+... a. Fe3+ bound by transferrin ---> into blood ---> transport to liver... b. stored in the "F &H Wharehouse" (ferritin & hemosiderin) to be used later... c. bound again to transferrin ---> into blood to bone marrow for new Hb synthesis. H. Factors required for RBC synthesis: 1. Fe3+: necessary diet nutrient 2. Vit B12: used for erythropoeisis in red bone marrow 3. Intrinsic factor: produced by stomach parietal cells - aids Vit B12 absorption in small intestine 4. Erythropoetin: hypoxia induces kidneys to increase erythropoetin secretion 5. Protein: amino acids used to produce globin Leukocytes: A. Granulocytes: 1. Neutrophils (50-70%); 3 day lifespan; major phagocyte & granulocyte; attracted by inflammatory factors and complement; granules with hydrolytic enzymes; cell dies after degranulation/phagocytosis a. Neutrophilia: increase %; common with acute bacterial infections b. Neutropenia: decrease %; common with anemias, viral infections, radiation/chemotherapy; i) Neutropenia can result in lowered immune protection especially to bacterial/fungal infections. 2. Eosinophils (2-4%); major anti-helminth protection (myelin basic protein released); also contributes to some hypersensitivity reactions and phagocytosis of bacteria. 3. Basophils (<1%); granulocytic, nonphagocytic; major inflammatory cell, releases histamines, proteases and granulocyte-attracting factors. 4. Monocytes (2-8%); only last 8-12 hrs in circ. then migrate to tissue = major function to become macrophage in tissue; play key role in "antigen presentation", express MHC-II. 5. Platelets (thrombocytes) (240-400,000/mm3); crucial to help activate blood clot formation, for platelet plug; spleen acts as reserve site; 6. Lymphocytes (20-30%) mononuclear cells; mediate/regulate specific immune responses (antibody formation, anti- viral and antitumor protection) a. B-cell: produce immunoglobulins (mature in bone marrow) b. T-cell: activate/regulate B-cells, major immune regulatory cells (mature in thymus) c. NK cell: natural killer cell; non-specific anti-tumor cytolytic cell Major Blood Group Antigens: A. ABO Antigens Individuals with Type A blood contain antibodies to Type B blood (anti-B antibodies) Individuals with Type B blood contain antibodies to Type A blood (anti-A antibodies) Individuals with Type AB blood contain no antibodies to either Type A or Type B blood Individuals with Type O blood contain antibodies to both Type A or B blood (anti-A and anti-B antibodies) B. Inheritance of Blood Types If person with AB blood and O blood have children, a Punnett square illustrates possible offspring blood types: A B i Ai Bi i Ai Bi This shows 50% offspring will be A i (A blood type) and 50% will be B i (B blood type) More Examples: Parents: heterozygous B type heterozygous A type Parents: homozygous A type AB type B i A AB Ai i Bi ii Offspring: 25% AB type 25% A type 25% B type 25% O type Parents: heterozygous B type heterozygous B type A A A AA AA B AB AB Offspring: 50% A type (homozyg.) 50% AB type B i B BB Bi i Bi ii Offspring: 25% B type (homozyg.) 50% B type (heterozyg.) 25% O type C. ABO Compatibility in Blood Transfusions Individuals with Type A blood contain antibodies to Type B blood (anti-B antibodies) Individuals with Type B blood contain antibodies to Type A blood (anti-A antibodies) Individuals with Type AB blood contain no antibodies to either Type A or Type B blood Individuals with Type O blood contain antibodies to both Type A or B blood (anti-A and anti-B antibodies) This table summarizes ABO tranfusion compatability: Donor blood type: Can safely donate to: Recipient blood type: Can safely receive blood from: A A or AB A A or O B B or AB B B or O AB AB only AB A, B, AB or O O A, B, AB and O O O only Rh+ Rh+ only Rh+ Rh+ or Rh- Rh- Rh+ or Rh- Rh- Rh- only D. Rh Antigen Rh expression is designated as Rh + (thus A+ blood has expression of A and Rh) Lack of Rh expression is designated as Rh - (thus B - blood has expression of B but no Rh) Important for Rh- mother pregnant with Rh+ child Sensitization of mother during delivery induces high levels of anti-Rh IgG antibodies; (block with Rhogam) During pregnancy with subsequent Rh+ child, anti-Rh IgG can cross placenta and cause hemolytic disease of newborn (less problem if Rhogam is administered during first delivery) Transfusions are typically restricted to matching Rh+ donor to Rh+ recipient. Rh - recipients should not be given Rh+ blood transfusion. Rh - blood can be transfused into Rh- or Rh+ recipient. (much like O blood can be given to any blood type) "Universal Donor" = O - "Universal Recipient" = AB + E. Blood Typing A small sample of blood is mixed with known reagents containing anti-A, or anti-B or anti-Rh. A positive reaction is where clumping (agglutination) occurs (antibody binds to RBCs in the blood) A negative reaction is where no agglutination occurs (antibody does not bind to RBCs) Severe (life-threatening) mismatch transfusion reactions can occur if donor and recipient do not match ABO type