Physiology and pharmacology of blood pressure regulation - Wk 1-2
advertisement
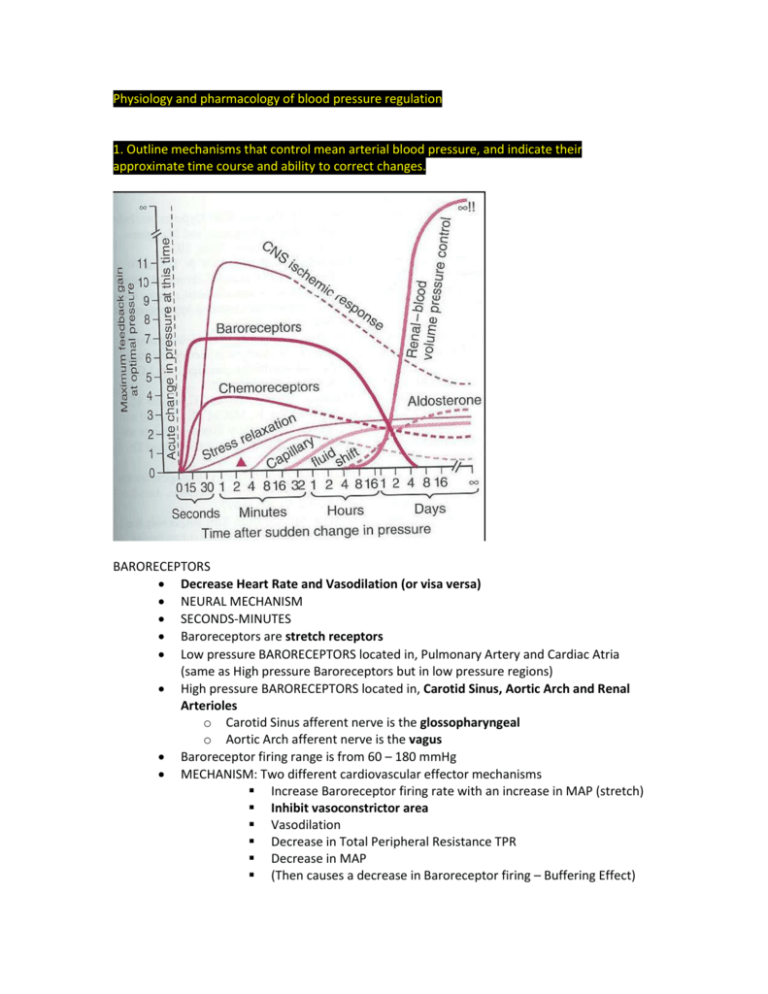
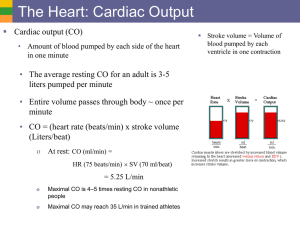
Physiology and pharmacology of blood pressure regulation 1. Outline mechanisms that control mean arterial blood pressure, and indicate their approximate time course and ability to correct changes. BARORECEPTORS Decrease Heart Rate and Vasodilation (or visa versa) NEURAL MECHANISM SECONDS-MINUTES Baroreceptors are stretch receptors Low pressure BARORECEPTORS located in, Pulmonary Artery and Cardiac Atria (same as High pressure Baroreceptors but in low pressure regions) High pressure BARORECEPTORS located in, Carotid Sinus, Aortic Arch and Renal Arterioles o Carotid Sinus afferent nerve is the glossopharyngeal o Aortic Arch afferent nerve is the vagus Baroreceptor firing range is from 60 – 180 mmHg MECHANISM: Two different cardiovascular effector mechanisms Increase Baroreceptor firing rate with an increase in MAP (stretch) Inhibit vasoconstrictor area Vasodilation Decrease in Total Peripheral Resistance TPR Decrease in MAP (Then causes a decrease in Baroreceptor firing – Buffering Effect) Increase Baroreceptor firing rate with an increase in MAP (stretch) Stimulate cardio-inhibitory centre Decrease heart rate and force of contractility Decrease in Cardiac Output CO Decrease in MAP (Then causes a decrease in Baroreceptor firing – Buffering Effect) PROBLEM: Blood Pressure can get ‘reset’ if the blood pressure is chronically elevated CHEMORECEPTORS Vasoconstriction NEURAL MECHANISM SECONDS-MINUTES Chemoreceptors are located on the Carotid (bifurcation in neck)and Aortic bodies (wall of the aortic arch) RESPOND TO: o Decrease in pO2 o Increase in pCO2 o Increase in H+ MECHANISM: Excite vasomotor centre/stimulate vasoconstriction o Decrease in Blood pressure causes; o Decrease in Blood flow; o Decrease in pO2 and Increase in pCO2 Chemoreceptors only sensitive to MAP < 80mmHg (they prevent further decrease in BP) CNS ISCHAEMIC REFLEX Accelerates Heart Rate and Vasoconstriction Very Powerful NEURAL MECHANISM SECONDS-MINUTES MECHANISM o ↓ Decrease in blood flow to vasomotor centre (in medulla oblongata) results in an ↑ increase in pCO2 causing: o Excitation of vasoconstrictor and cardioaccelerator neurons in vasomotor centre DIRECT RENAL MECHANISM Reduce Blood Volume DIRECT MECHANISM HOURS ↑ Increase in Blood volume or Blood Pressure ↑ Increased rate of renal filtration ↓ Decreased rate of renal filtrate reabsorption (as less salt is reabsorbed water follows it out of the body. This is seen as a direct renal mechanism: without use of hormones) ↑ Increased volume of filtrate excreted as urine ↓ Decrease blood volume RAAS SYSTEM – RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM HORMONAL MECHANISM – Indirect Renal Mechanism HOURS ↓ Decrease in Blood Pressure (Renal perfusion pressure) PRORENIN is converted to RENIN in the juxtaglomerular cells of the kidney and ↑ RENIN is secreted into the blood. In the plasma RENIN (enzyme) catalyses the conversion of ANGIOTENSINOGEN to ANGIOTENSIN I In the lungs and kidneys ANGIOTENSIN I is converted to ANGIOTENSIN II by the enzyme ACE (Angiotensin-converting enzyme) ANGIOTENSIN II FUNCTIONS A. Acts on the Adrenal cortex to synthesize and secret ALDOSTERONE. Aldosterone then acts on the principal cells of the renal distal tubule and collecting duct to increase Na+ reabsorption Increase blood volume B. ANGIOTENSIN II acts directly on the EFFERENT arterioles to cause: Vasoconstriction C. ANGIOTENSIN II has a direct action on the kidney. o Stimulates the exchange between H+ and Na+ in the renal proximal tubule o Increases the reabsorption of Na+ and HCO3 Increase blood volume D. ANGIOTENSIN II acts on the hypothalamus to: o increase thirst and water intake Increase blood volume o stimulate secretion of ANTIDIURETIC HORMONE Increases the ability to concentrate urine so more water can be kept in the blood Concentrating urine Helps to increase blood volume E. ANGIOTENSIN II is a HYPERTROPHOGENIC agent causing Smooth Muscle Cell and Myocyte hypertrophy LOW PRESSURE ATRIAL RECEPTORS HORMONAL MECHANISM ↑ Increase in Central Venous Pressure CVP causes distension in the Atria Send afferents to the Hypothalamus ↓ Decreasing secretion of ADH o ANTIDIURETIC HORMONE increases the ability to concentrate urine Helps to decrease blood volume Low Pressure Atrial Receptors secrete NATRIURETIC (produce salty urine) PEPTIDES o ↑ Increases GFR o ↓ Decreases Sodium reabsorption so there is less sodium in the blood to keep water in the blood: decreasing blood pressure o Basically counters the RAAS system: it is a fine tuning system Helps to decrease blood volume 2. Outline the function of the renin-angiotensin system, naming the components, listing the controlling inputs to the system, and listing the principal actions of angiotensin II. 3. Describe nervous mechanisms which defend against rapid changes in blood pressure. See above ↑






![Anti-Angiotensin II antibody [BGN/0856/21] ab35643 Product datasheet Overview Product name](http://s2.studylib.net/store/data/011980713_1-1b1e68585550d552e091ae57faa2980f-300x300.png)