Section 2 - Lindley Habilitation Services
advertisement

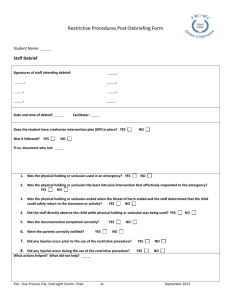
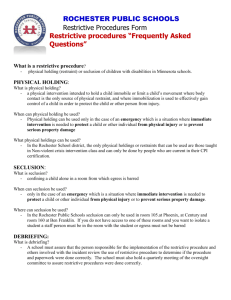
Section 2 Intervention Procedures and Client Rights Committee 2.1 Employment of Interventions The following procedures shall only be employed when clinically or medically indicated as a method of therapeutic treatment Planned non-attention to specific undesirable behaviors when those behaviors are health threatening Contingent deprivation of any basic necessity Other professionally acceptable behavior medication procedures that are not prohibited The determination that a procedure is clinically or medically indicated and the authorization for the use of such treatment for a specific client shall only be made by either a physician or a licensed practicing psychologist who has been formally trained and privileged in the use of the procedure. 2.2 Least Restrictive Alternative The goal of Lindley Habilitation Services is to use the least restrictive, most appropriate and effective positive treatment modality. The use of a restrictive intervention procedure designed to reduce a behavior shall always be accompanied by positive treatment or habilitation methods which shall include: The deliberate teaching and reinforcement of behaviors which are non-injurious The improvement of conditions associated with non-injurious behaviors which as an enriched educational and social environment The alterations or elimination of environmental conditions which are reliably correlated with self injury 2.3 Prohibited Interventions The following interventions will be prohibited: Isolation time out: time out in a room with the door closed Corporal punishment (spanking/hitting): it is against the law to punish consumers Seclusion: placing a consumer in a locked room Chemical restraint: sedating or medicating a consumer w/o authorization as a medical intervention Taking away basic rights: overcorrecting efforts, physical intervention,(except in emergency to prevent injury to consumer or others) Taking away basic rights: taking away meals, bathroom, well ventilated rooms, lights or other basic needs of daily living Abusive verbalization: staff do not tease, ridicule or swear at clients Contingent medical restraint: any object used to restrict movement, seatbelt, helmet, gloves, or tight clothing to restrict movement to client’s body Planned ignoring of threatening behaviors: SIB’s (self injurious behavior), that may cause injury to client’s self Physical restraints or seclusion of client shall be employed only when there is imminent danger abuse or injury to self or others, when substantial property damage is occurring, or when the restraint or seclusion is necessary as a measure of therapeutic treatment. All instances of restraint or seclusion and the detailed reasons for such action shall be documented on an incident/accident report form and kept in the Human Rights Committee file. Each client who is restrained or secluded shall be observed frequently, and written notation of the observation shall be made by the supervisor and kept in the client’s file. LINDLEY HABILITATION SERVICES may adopt additional rules to implement this section. 2.4 Rules for Physical Restriction for Behavioral Control The use of restrictive interventions shall be limited to emergency situations, in order to terminate a behavior or action in which a client is in imminent danger of abuse or injury to self or other persons or when property damage is occurring that poses imminent risk of danger of injury or harm to self or others; or as a planned measure of therapeutic treatment as specified. Restrictive interventions shall not be employed as a means of coercion, punishment or retaliation by staff or for the convenience of staff or due to inadequacy of staffing. Restrictive interventions shall not be used in a manner that causes harm or abuse. 2.5 Staff Training for Physical Restraint Lindley Habilitation Services staff will be certified in NCI standards for restraint policies. The trainer will be responsible to LHS to provide the structure for the class and to certify or not any staff trained in their classes. All LHS staff will attend part A of the NCI standards for prevention techniques. To remain or become eligible for employment under CAP MR/DD regulation, successful completion of part A is mandatory for all staff. To begin a permanent or fill-in position NCI part A must be completed during the training period. Core or Core Plus of NCI standards is required for all direct care staff who work with clients that may become aggressive. The core or Core Plus techniques for NCI will be taught and reported to LHS, Inc. and QPs (Qualified Professional. Records of staff participation shall be maintained for five years. Each staff must pass all NCI testing requirements annually to maintain certification 2.6 Consent for Restrictive Interventions The use of physical interventions may be planned, as written in a behavior plan, or used in an emergency situation to protect a client from hurting themselves or others. Each client regardless, of a history of aggressive behaviors or the presence of a behavior plan with planned physical interventions shall be notified of possible interventions that have been approved for use. This notification shall be in writing and shall be signed by the client and/or legally responsible party at the time the Consent Packet is completed by the Qualified Professional or other designated party. This signature shall be considered consent given for use of approved interventions. If the client is known to have aggressive behaviors or a behavior plan which may require the use of restrictive interventions and the client and/or legally responsible party refuses consent, the admission of the client or continuation of services shall be reviewed by the NCI instructor, Qualified Professional and Regional Director to make a decision if the client can be admitted or continue services due to safety and liability issues for the client and the agency. If there is a medical reason a physical intervention cannot be used, a doctor’s note shall be given to the agency and kept in the client’s permanent file as well as the staff file kept in the client’s home. All staff will be notified and required to sign a statement of understanding that restrictive interventions shall not be used. Lindley Habilitation Services reserves the right to refuse treatment to any client whose behaviors are deemed to be a threat to staff and/or themselves and consent is not given for use of restrictive interventions. This determination shall be made by the NCI instructor after review of the case and history of behaviors. If a client has a physical disability or surgery that would make affected nerves/bones sensitive to injury, Lindley Habilitation Services may choose not to serve these clients. If Lindley Habilitation Services assesses that the client’s safety and health cannot be adequately maintained, the client will be discharged. Any surgery or physical disability will be documented in the client’s record. Reporting of any change in health status is the responsibility of the Legally Responsible Party or Client. Possibilities of limits which would warrant not serving a client are but not limited to: Breathing difficulties Heart related issues Fragile bones Size of client, related to staff size 2.7 Notification of Restrictive Interventions In the event a restrictive intervention is required, either as a planned intervention or used in an emergency situation to protect the client or others, the legally responsible person of a minor or incompetent adult client will be notified after the occurrence and before the staff leaves the shift. Proper documentation will be completed by the staff involved in the intervention and submitted to the agency within 24 hours. The agency will submit the documentation to the LME as directed. 2.8 Monitoring of Client during Intervention Consideration will be given to the client’s physical and psychological well-being before, during and after utilization of a restrictive intervention. This will include: review of the client’s health history or the client’s annual physical received by the agency and reviewed by the agency nurse upon admission to services. The history or physical shall include the identification of pre-existing medical conditions or any disabilities and limitations that would place the client at greater risk during the use of restrictive interventions; continuous assessment and monitoring of the physical and psychological well being of the client and the safe use of restraint throughout the duration of the restrictive intervention by staff who are physically present and trained in the use of emergency safety interventions; continuous monitoring by an individual trained in the use of cardiopulmonary resuscitation of the client’s physical and psychological well being during the use of ,manual restraint; and continued monitoring following the restrictive intervention by an individual trained in the use of cardiopulmonary resuscitation of the client’s physical and psychological well being for a minimum of 30 minutes subsequent to the termination of a restrictive intervention. 2.9 Documentation of Restrictive Interventions Whenever a restrictive intervention is utilized, the correct documentation from the State will be completed and sent to the appropriate LME(s) within the timeframe required by the State. Documentation shall be made in the client record to include: notation of the client’s physical and psychological well being; notation of the frequency, intensity and duration of the behavior which led to the intervention, and any precipitating circumstance contributing to the onset of the behavior; the rationale for the use of the intervention the positive or less restrictive interventions considered and used and he inadequacy of less restrictive intervention techniques that were used; a description of the intervention and the date, time and duration of its use; a description of accompanying positive methods of intervention; a description of the debriefing and planning with the client and legally responsible person if applicable, for the emergency use of seclusion, physical restraint or isolation time out to eliminate or reduce the probability of future use of restrictive interventions; a description of the debriefing and planning w/ the client and the legally responsible person if applicable, for the planned use of seclusion, physical restraint or isolation time out if determined to be clinically necessary; and signature and title of the agency employee who initiated and the of the employee who further authorized the use of the intervention. 2.10 Emergency Restrictive Interventions The use of a restrictive intervention in the case of an emergency shall be limited as follows: An employee approved to administer emergency interventions may employ such procedures for up to 15 minutes without further The continued use of such interventions shall be authorized only by the responsible professional or another qualified professional who is approved to use and to authorize the use of the restrictive intervention based on experience and training; the responsible professional shall meet with and conduct an assessment that includes the physical and psychological well being of the client and write a continuation authorization as soon as possible after the time of initial employment of the intervention. If the responsible professional or qualified professional is not immediately available to conduct an assessment of the client, but concurs with the intervention is justified after discussion with the employee, continuation of the intervention may be verbally authorized until an on-site assessment of the client can be made; A verbal authorization shall not exceed three hours after the time of the initial employment of the intervention; and Each written order for seclusion, physical restraint or isolation time out is limited to four hours for each adult client; two hours for children and adolescent clients ages 9-17; or one hour for clients under the age of nine. The original order shall only be renewed in accordance with these time limits or up to a total of 24 hours. The use of restrictive interventions shall be discontinued immediately at any indication of risk to the client’ health or safety or immediately after the client gains behavioral control. 2.11 Notification of Restrictive Intervention When any restrictive intervention is utilized for a client, notification of others shall occur as follows: The on-call supervisor or the Qualified Professional supervising the case shall be notified within 24 hours The Regional Director or other designee of the agency shall be notified within 24 hours of the next working day after each use of the intervention The legally responsible person of a minor child or an incompetent adult client shall be notified immediately unless she/he has requested not to be notified. Proper documentation shall be completed within 24 hours of the intervention and sent to the LME within 72 hours of the intervention. 2.12 Planned Interventions A restrictive intervention shall be considered a planned intervention and shall be included in the client’s treatment/habilitation plan whenever it is used: More than four times, or for more than 40 hours, in a calendar month In a single episode in which the original order is renewed for up to a total of 24 hours in accordance with the limit specified; or As a measure of therapeutic treatment designed to reduce dangerous, aggressive, self injurious or undesirable behaviors to a level which will allow the use of less restrictive treatment or habilitation procedures. When a restrictive intervention is used as a planned intervention a consent or approval shall be considered valid for no more than 6 months and the decision to continue the specific intervention shall be based on clear and recent behavioral evidence that the intervention is having a positive impact and continues to be needed. Plans will be reviewed as the client’s POC is reviewed every six months. Prior to the initiation or continued use of any planned intervention the following written notifications, consents and approvals shall be obtained and documented in the client record: Approval of the plan by the responsible professional and the treatment and habilitation team, based on an assessment of the client and a review of the documentation Consent of the client or legally responsible party, after participation in treatment planning and after the specific intervention and the reason for it have been explained Notification of an advocate/client rights representative that the specific intervention has been planned for the client and the rationale for utilization of the intervention; and Physician approval, after an initial medical examination, when the plan includes a specific intervention with reasonably foreseeable physical consequences. In such cases, periodic planned monitoring by a physician shall be incorporated in the plan. Within 30 days of initiation of the use of a planned intervention, the Client Rights Committee/Intervention Advisory Committee, by majority vote, may recommend approval or disapproval of the plan or may abstain from making a recommendation. The CRC/IAC, shall be given the opportunity to review the treatment/habilitation plan any time during the use of a planned intervention. If any of the persons or committee do not approve the initial use or continued use of a planned intervention, the intervention shall not be initiated or continued. Appeals regarding the resolution of any disagreement over the use of the planned intervention shall be handled by the Vice Presidents and CEO. Documentation in the client record regarding the use of a planned intervention shall indicate: Description and frequency of debriefing with the client, legally responsible person, if applicable, and staff if determined to be clinically necessary. Debriefing shall be conducted as to the level of cognitive functioning of the client; Bi-monthly evaluation of the planned intervention by the responsible professional who approved the planned intervention; and Review, at least monthly, by the treatment/habilitation team that approved the planned intervention. 2.13 Protective Devices If a protective device is utilized for a client it shall be reviewed by the Client Rights Committee to ensure the necessity for the protective device has been assessed as well as the consideration for the use of positive and less restrictive alternatives have been examined and documented. Any staff using the protective device will have documentation stating they have been trained and have demonstrated competence in the utilization of the device. The staff will assure the client is frequently observed and provided opportunities for toileting, exercise, etc. as needed. When the device limit’s the client’s freedom of movement, the client shall be observed at least every hour. Whenever the client is restrained by the device and subject to injury by another client, the staff shall remain present with the client continuously. The use of any protective device for the purpose or with the intent of controlling unacceptable behavior shall comply with the policy on Behavior Control in this section. 2.14 Client Rights Committee The Client Rights Committee shall also serve as the Intervention Advisory Committee for Lindley Habilitation Services. The membership of this committee shall include at least one person who is or has been a consumer of direct services provided by the governing body or who is a close relative of a consumer and at least three citizens who are not employees of this agency. The committee shall have a member or a regular independent consultant who is a professional, an NCI trainer and has expertise in the use of the type of interventions being utilized and who is not directly involved in the treatment or habilitation of the client. The Intervention Advisory Committee will review planned intervention plans. The Client Rights Committee shall have access to client information only when necessary for committee members to perform their duties. In addition, members shall have access to client records on a need to know basis only upon the written consent of the client or his legally responsible party. Information in the client record shall be treated as confidential. Members of the Client Rights Committee shall be trained on agency policy as well as Client Rights Training. They shall be provided with copies of Client Rights Rules and have access to agency policies and procedures. When reviewing interventions, they shall be provided with information about proposed interventions and alternatives. Minutes shall be maintained by the committee and they shall make an annual written report to the agency on the activities the committee reviewed each quarter of the fiscal year.