A Clinician`s Guide to Pulmonary Edema
advertisement

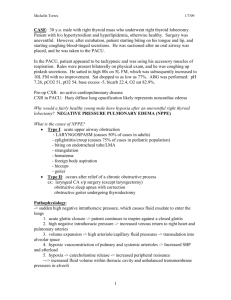
PULMONARY EDEMA HUGH O’BRODOVICH PAGE 1 PULMONARY EDEMA A PHYSIOLOGIC APPROACH TO PEDIATRIC LUNG DISEASES Hugh O’Brodovich MD, FRCP(C) Department of Pediatrics, Stanford University School of Medicine, Stanford, CA, USA 94305 Running Title: PULMONARY EDEMA Hugh O’Brodovich MD, FRCP(C) Arline & Pete Harman Professor and Chairman Department of Pediatrics, Stanford School of Medicine Adalyn Jay Physician-in-Chief, Lucile Packard Children's Hospital Department of Pediatrics Stanford School of Medicine 300 Pasteur Drive , Room H310 Stanford , CA 94305-5208 Ph: (650) 723-5104 Fax: (650)725-7419 Hugh.OBrodovich@Stanford.edu HUGH O’BRODOVICH PULMONARY EDEMA PAGE 2 Improvements in the intensive care and monitoring of patients with serious illnesses led to a greater appreciation of the significance of fluid movement into the lung as a complication of a variety of conditions. This, coupled with an improved understanding of the pathogenesis of pulmonary edema, has enhanced our ability to treat a variety of illnesses in which pulmonary edema develops. Anatomic Considerations1 The lung as an organ of gas exchange is remarkable. Although 300 liters of blood flows through its capillaries every hour the 300-600 million alveoli remain essentially dry and filled with air. Thus gases can diffuse easily across the 2 um thick air-blood barrier that is present throughout the entire 140 m2 of alveolar surface area. The alveolar gas tensions equilibrate with the gas tensions that are present in the 210 ml of capillary blood that is present at any one time in normal lungs. Pulmonary capillaries have a continuous endothelium with relatively tight intercellular junctions (~ 40 Å effective molecular radius). The epithelial tight junctions (zonulae occludentes) are much tighter and have an estimated effective molecular radius of ~ 4 Å. The implication is that while proteins, but not ions, are osmotically active across the endothelial membrane these same ion are osmotically active across the epithelial membrane. Pulmonary edema is defined as excess fluid within the lung’s interstitium or airspaces and it is important to note that these two spaces are dramatically different in their capacity for fluid. While the interstitial space is approximately 200 ml, the alveolar space is equivalent to the individual’s functional residual capacity (FRC) which, for an adult, is several liters. Forces Responsible for Fluid Movement in the Lung The factors responsible for fluid accumulation include intravascular and interstitial hydrostatic and colloid osmotic pressures, permeability characteristics of the fluid-exchanging membrane, and lymphatic drainage. The equilibrium of fluid across fluid-exchanging membranes is generally expressed as the Starling equation as follows: Qf = Kf ((Pmv − Ppmv) − σ(πmv − πpmv)) wherein Qf = the net transvascular flow, Kf = the filtration coefficient of the fluid-exchanging vessels and includes both the contribution of the permeability of the vessels and the surface area across which fluid exchange occurs, Pmv = microvascular hydrostatic pressure, Ppmv = perimicrovascular (interstitial fluid) hydrostatic pressure, πmv = colloid osmotic pressure in the microvasculature, πpmv = colloid osmotic pressure in the perimicrovasculature, the interstitial fluid colloid osmotic pressure, and σ = the reflection coefficient and is a measure of the 1 Values provided are for the adult lung PULMONARY EDEMA HUGH O’BRODOVICH PAGE 3 resistance of the membrane to the movement of protein. Thus, it determines the “effective” osmotic pressure of the protein. If the endothelium were completely impermeant to protein (σprotein = 1) then the 5 g/dL of plasma would yield approximately 28 mm Hg oncotic pressure (each 1 mOsm/L of solute yields 19 mm Hg pressure). Pathophysiologic Consequences of Pulmonary Edema It is important to understand the sequence of excess fluid accumulation within the lung. Once lymphatic drainage is overwhelmed the excess fluid first accumulates within the interstitial space within the bronchopulmonary vascular bundle. As noted above, this capacity of the interstitial space is only a few hundred mls so if the pathologic process continues then fluid will flood into the alveolar space. It is typical for distal lung units in different regions of the lung to be at different stages of fluid accumulation as a result of regional differences in pressure, alveolarcapillary integrity and gravitationally dependent factors. Three different components are responsible for the changes in lung function: The fluid overload component, such as occurs in congestive heart failure, increases the pulmonary vascular volume and engorges the pulmonary vasculature. This engorgement results in stiffening as reflected in a fall in total lung compliance (CL). The interstitial edema component induces tachypnea by two mechanisms. One is the stimulation of juxta-capillary (J) receptors. The other is a secondary effect from an increased small airway resistance. This interstitial edema induced increase in small airway resistance causes changes in ventilation (VA) / perfusion (P) ratios resulting in 0 < VA/Q < 1. This lowers alveolar PO2 (PAO2) with a resultant drops in PaO2. If PaO2 falls to less than 60 mm Hg hypoxia induced hyperventilation will occur. There are two mechanisms for the increase in small airway resistance; vagal nerve stimulation and small airway compression from the excess fluid within the bronchovascular bundle (this latter point is debated in the literature). The alveolar edema component increases pulmonary vascular resistance because of the decrease in PAO2 and the decrease in lung volume (VL). The lung volume decreases because a fluid filled lung unit occupies decreases its volume relative to an air-filled unit. The alveolar edema results in shunt (VA/Q = 0) which further increases the hypoxemia. Clinical Assessment of Pulmonary Edema The patient will be tachypneic from juxta-capillary receptor stimulation and stimulation from the hypoxia sensitive receptors in the carotid body and aorta. Hypoxemia, resulting from both low VA/Q ratios and shunt, will be present. An increase in the work of breathing occurs from the “cardiac asthma”, the decreased CL, and when there is alveolar edema from the proteins contained therein inhibiting surfactant function. Mild pulmonary hypertension will also be present and this occurs from the increased pulmonary blood volume and regional vasoconstriction when PAO2 falls below 60 mm Hg. Standard imaging studies are insensitive in detecting mild interstitial pulmonary edema. Lung water content must increase by at least 35% before changes are seen. The engorgement of the PULMONARY EDEMA HUGH O’BRODOVICH PAGE 4 pulmonary vascular bed causes recruitment and distention of upper lobe vessels. Interstitial edema will be evident by cuffing around the bronchovascular bundle and enhancement of the septal lines (Kerly A and Kerly B lines). Once alveolar edema occurs there will be an acinar pattern within the lung. The actual lung volume can varies dependent on whether it is predominately interstitial or alveolar edema: the former will have increased lung volume whereas the latter will have a reduction in lung volume. Computed axial tomographic (CAT) and magnetic resonance imaging (MRI) studies of the lungs provide more detail of the lung parenchyma and vasculature, respectively. However, similar to plain chest radiographs, CAT evaluation reveals changes in density and not fluid content. Thus an increase in density (opacity) can result from either an increase in fluid content or a decrement in the amount of air. Causes of Pulmonary Edema There are many diseases associated with pulmonary edema, however, there are only two causes: an increase in the transvascular hydrostatic gradient and an increase in the permeability of the alveolar-capillary membrane to fluid and solutes. The former is termed “high pressure”, with the most common cause being heart failure. The latter is termed “high permeability” or “noncardiogenic” pulmonary edema. Although this is useful to some degree, it should be remembered that both abnormal transvascular pressure gradients and increased permeability to solutes are present or subsequently develop in many lung diseases characterized by pulmonary edema. The various diseases leading to pulmonary edema are best understood by re-visiting the Starling equation. For example, heart failure increases Pmv whereas croup or re-expansion pulmonary edema is associated with marked increases in Ppmv. High permeability pulmonary edema is associated with an increase in KF and σ. It is important to note that although a fall in plasma protein, and hence πmv, will exacerbate fluid leakage from other causes it does not by itself cause pulmonary edema. This conclusion is supported by an analysis of the Starling equation and the clinical observation that patients with nephrotic syndrome do not have either interstitial or alveolar edema. Clearance of Pulmonary Edema It is important to emphasize that although further generation of edema fluid is diminished, alveolar edema is not cleared by any of positive airway pressure, increasing the colloid osmotic pressure nor the administration of diuretics. How quickly pulmonary edema resolves, once the basic condition producing the edema is reversed, depends on whether the fluid is confined to the interstitium or is also located in the alveolar space. Interstitial edema is cleared by the lymphatics whereas the alveolar edema is cleared by the active transport of Na+, with Cl- and water following, by the distal lung epithelium. It is estimated that the human lung clears airspace fluid at a rate of 25% per hour. Treatment of Pulmonary Edema PULMONARY EDEMA HUGH O’BRODOVICH PAGE 5 Understanding the underlying mechanisms for pulmonary edema leads to a pragmatic approach to therapy. These can be summarized into four key areas: 1. Reversal of hypoxemia: a. Increase FIO2 to treat 0 < VA/Q < 1; b. Recruit lung volume by increasing mean airway pressure when shunt (VA/Q = 0) is present. 2. Optimize lung volume to improve: a. VL by positive airway pressure and/or prone positioning; b. PVR. Note that PVR is at its minimum at FRC; c. Ppmv (since Ppmv is related to pleural pressure for extra-alveolar vessels). 3. Reduce the rate of fluid filtration out of the vascular bed: a. Decrease Pmv by i. Decreasing intravascular volume ii. Relieving pulmonary (veno) vasoconstriction iii. Optimizing pulmonary blood flow b. Decrease Ppmv by reducing the work of breathing and hence pleural pressure; c. Increase KF and σ by treating the underlying process (eg. infection, pancreatitis), minimizing volu-trauma or other deleterious processes, etc) 4. Increase the rate of airspace fluid clearance. EXTRA READING In addition to the references indicated within the powerpoint presentation course, participants can obtain a more in depth understanding of this subject by seeking further information in review articles. These include those describing classic physiologic – pathophysiologic research findings 1, cellular mechanisms underlying active fluid transport within the distal lung unit 2 3 and a detailed reviews with descriptions of pediatric 4 and adult 5 disorders associated with pulmonary edema. ACKNOWLEDGEMENT: The above transcript was also utilized by the author as the syllabus for a Postgraduate Course scheduled prior to the American Thoracic Society Meeting held in New OrleansMay 15th, 2010 Reference List 1. Staub, N. C. 1976. Pathogenesis of pulmonary edema. Am.Rev.Respir.Dis. 109:358-372. 2. Matthay, M. A., H. G. Folkesson, and C. Clerici. 2002. Lung epithelial fluid transport and the resolution of pulmonary edema. Physiol Rev. 82:569-600. 3. Folkesson, H. G. and M. A. Matthay. 2006. Alveolar epithelial ion and fluid transport: recent progress. Am.J.Respir.Cell Mol.Biol. 35:10-19. PULMONARY EDEMA HUGH O’BRODOVICH PAGE 6 4. O'Brodovich, H. 2006. Pulmonary Edema. In V. Chernick, T. Boat, R. Wilmott, and A. Bush, editors Kendig's Disorders of the Respiratory Tract in Children,7 ed. Saunders Elsevier, Philadelphia. 622-638. 5. Ware, L. B. and M. A. Matthay. 2005. Clinical practice. Acute pulmonary edema. N.Engl.J.Med. 353:2788-2796.