Case:
advertisement
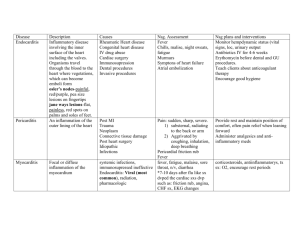
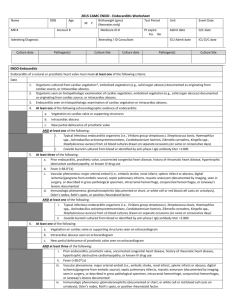
Resident Version Infective Endocarditis Module Created by Dr. Wendy Gerstein Updated 5/09 Objectives: 1. Identify 4 risk factors and organisms associated with endocarditis. 2. Be able to use Duke Criteria to diagnose endocarditis. 3. Be able to choose initial empiric therapy for suspected endocarditis. 4. Recognize 3 common complications of endocarditis and institute appropriate management. References: 1. Mandell, Douglas, and Bennets Principles and Practices of Infectious Diseases, sixth edition, Volume I; Cardiovascular Infections. 2. www.uptodate.com “infective endocarditis” and “prosthetic valve infections” 3. Reese and Betts ’ a Practical Approach to Infectious Diseases, Fifth Edition, chapter 12 “Infective Endocarditis.” CASE Patient is a 79 yo male with past medical history notable for diabetes, hypertension, and aortic prosthetic valve replacement who presents with abrupt onset of dizziness, fever to 103 F, weakness, and associated cough with sputum (unknown color). Patient denied chest pain or tightness, denied sob, no GI or GU symptoms. He had no sick contacts, no recent travel or procedures. No rashes and no recent breaks in skin except small wound on left shin from bumping into metal chair, occurred one week ago, wife and patient did not notice any signs of infection. Past medical history: AVR with mechanical valve 18 years ago Hypertension Diabetes Hypercholesterolemia Claudication Sciatica BPH Medications: Percocet prn Asa 81 mg daily Finasteride 5 mg daily Irbesartan 150 mg daily Lovastatin 40 mg daily Methocarbamol 500 mg tid Warfarin 5 mg daily Allergies: PCN – does not recollect reaction Social history: Lives with wife, retired military, quit tobacco and alcohol 40 years ago PE: T = 101.0 F, P 92-98, BP 101/40, RR 22 O2 Sat 93% RA Gen: alert and oriented x 3, appears comfortable Skin: no rashes, lesions, or evidence of embolic events; has one small dime size wound on left shin, no surrounding erythema, scab in place. Heent: PERRLA, EOMI, conjunctiva non-injected; mouth with pink, moist membranes, no petechiae; neck without adenopathy, supple; teeth in good repair. Lungs: few crackles at bases bilaterally, L>R; no wheezing, no egophony/dullness noted. CV: Regular, s1, prominent s2, 2-3/6 SEM LUSB, and 2-3/6 SEM heard over apex. Apex non-displaced. Normal pulses present. Abd: soft, nt/nd, + bs, no masses, liver normal size. Ext: no edema, warm, well-perfused. Neuro exam – CN 2-12 intact/symmetric, strength normal, sensation intact. Initial labs/studies: UA completely negative except trace blood and 3 rbc/hpf BUN/creatinine 48/1.8 (baseline 1.0) Sodium 129, K 4.4, Cl 97, CO2 22 Transaminases and lfts wnl Wbc 12.7, 94.9% neutrophils Hct 43, platelets 151 INR 1.8 CXR: read by your resident:? patchy opacity LLL (small) – could be atelectasis vs small infiltrate. EKG: no acute ST changes, normal intervals, no conduction abnormalities. 1. What is your initial differential diagnosis and management plan for this patient based on the above information? 2. What is your working diagnosis now and how should management change? TEE results: negative for vegetation, and shows a functioning AVR, and thickened mitral valve leaflets with calcification. 3. Has endocarditis been ruled out, and can you safely stop the antibiotics? Review Questions: 1. Predictors of mortality in prosthetic valve endocarditis (PVE) include which of the following? A) Late prosthetic valve infection B) S. viridans infection C) Severe heart failure D) Persistent fever after 48 hours of antibiotics 2. Which organism is most frequently isolated in early (<60 days after implantation) PVE? A) S. viridans B) S. aureus C) E. faecalis D) S. epidermidis E) No organism identified 3. True or False questions A) The Duke criteria for diagnosing endocarditis include echocardiography. B) The TEE has 100% negative predictive value for endocarditis. C) You can diagnose endocarditis with five minor criteria in the Duke Classification system. D) Osler nodes and Roth spots are both immunologic phenomena. E) Streptococcus species cause 60-80% of all native valve endocarditis. Outline for discussion: 1. Definition of infective endocarditis (IE): Infection of the endocardial surface of the heart; can include heart valves, septal defects, mural endocardium. In addition arteriovenous, arterioarterial shunts (PDA), and infections associated with coarctation of the aorta are clinically similar. 2. Epidemiology A) Accounts for one case per 1000 hospital admissions B) Annual incidence in the US is 10-20,000 new cases a year C) Median age 58, men affected more commonly D) Risk factors: most structural heart disease predisposes to IE (particularly if creates disturbance in blood flow). - Rheumatic heart disease major risk factor in the past in the US, but now most predisposing cardiac condition only in developing countries. - Congenital heart disease - Marfan syndrome - Degenerative cardiac lesions - Mitral valve prolapse with thickened leaflets/redundancy - Hemodialysis shunts/fistulas/nosocomial bacteremia - Intracardiac prothesis (prosthetic valves), pacemaker wires, defibrillators - IVDU - HIV infection 3. Pathophysiology (simplified version) A) Alteration of valve surface appears to be a prerequisite for subsequent bacterial colonization. Initial alteration or trauma of the valve causes sterile fibrin-platelet deposits to form, with associated interstitial edema and cellular distortion (called nonbacterial thrombotic endocarditis – NTBE). B) Areas of turbulent blood flow create conditions that subsequently lead to bacterial colonization of NTBE lesion during transient bacteremia. C) Transient bacteremia occurs whenever a mucosal surface heavily colonized with bacteria is traumatized (dental extractions, GI/GU procedures). Low grade bacteremia, usually lasts < 15-30 minutes. D) These organisms can then adhere to the NBTE lesion on the valve, multiply, causing IE. E) Certain organisms are much more likely than others to adhere to the NBTE lesion. 4. Signs and Symptoms (severity related to causative agent) A) Subacute Bacterial Endocarditis (SBE): insidious onset, weakness, fatigue, night sweats, myalgias, fevers, can be for weeks to months. On exam there is evidence of chronic illness, fever, and new murmur. Stigmata of endocarditis may be present. B) Acute Bacterial Endocarditis (ABE): abrupt onset of symptoms with high fevers, chills, back pain, myalgias, usually ongoing for only a few days. On exam patient is usually clinically ill with high fever, new murmur. Stigmata of endocarditis may be present. C) Other signs to look for include evidence of CHF, heart block or arrhythmias, pericarditis (rare), and neurological symptoms. 5. Pathogens A) Streptococci species are responsible for 60-80% of native valve IE. This includes alpha-hemolytic strep species, Group D strep, S. pneumoniae, Group B strep, Group G strep, Group A strep (in order of frequency). Reminder: S. bovis is associated with colonic carcinoma – all patients with this organism need a colonoscopy. B) Staphylococci (coagulase positive > >> negative) are seen in 20-30% of cases. In 1/3rd of cases of S. aureus acute IE, bacteria attack “normal” valves. S. aureus IE is very acute/fulminant, 40% mortality. C) Enterococci species: 5-18% of cases, usually subacute process, high mortality due to intrinsic resistance of organisms. D) Gram negative bacilli: 1-5% of cases. Persistent bacteremia common, CHF common, mortality high (40-50%). Salmonella, E. coli, Klebsiella, Pseudomonas, Serratia (IVDU). E) Fungi: associated with IVDU, health care associated infection, cardiovascular surgery. 2-4% of cases. F) Rare: Neisseria species, HACEK organisms (Haemophilus, Actinobacillus, Cardiobacterium, Eikenella, Kingella), anaerobic bacteria. G) IVDUs: S. aureus (MRSA), Pseudomonas, Serratia, strep species, polymicrobial, fungal. H) Culture negative: Coxiella burnetii, Bartonella species, presence of antibiotics. 6. Diagnosis A) Duke Criteria: uses both clinical and pathological criteria to classify cases as definite. Definite cases of endocarditis require one of the following: - Direct evidence of IE based on histology - Gram’s stain results or cultures of specimens obtained from surgery or autopsy. - Two major criteria (see table below) - One major and any three minor criteria - Five minor criteria Table 1. Modified Duke criteria for the diagnosis of infective endocarditis (IE) Major criteria: 1) Positive Blood cultures for IE A) Typical microorganisms consistent with IE from 2 separate blood cultures: - viridans streptococci - Streptococcus bovis, HACEK group, - Staphylococcus aureus; - Community-acquired enterococci, in the absence of a primary focus; OR B) Persistently positive blood cultures, defined as recovery of microorganisms consistent with IE from: -At least 2 positive cultures of blood samples drawn 12 h apart - All of 3 or a majority of >4 separate cultures of blood (with first and last sample drawn at least 1 h apart) OR C) Single positive blood culture for Coxiella burnetii or antiphase I IgG antibody titer >1:800. 2) Evidence of endocardial involvement A) Echocardiogram positive for IE (TEE recommended in: patients with prosthetic valves, rated at least “possible IE” by clinical criteria, or complicated IE [paravalvular abscess]; TTE as first test in other patients): -Oscillating intracardiac mass on valve or supporting structures, in the path of regurgitant jets, or on implanted material in the absence of an alternative anatomic explanation. -Abscess -New partial dehiscence of prosthetic valve OR B) New valvular regurgitation (worsening or changing of pre-existing murmur not sufficient. Minor criteria 1) Predisposition: predisposing heart condition or injection drug use. 2) Fever, temperature 38.0C. 3) Vascular phenomena: major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhages, and Janeway’s lesions. 4) Immunologic phenomena: glomerulonephritis, Osler’s nodes, Roth’s spots, and rheumatoid factor. 5) Microbiological evidence: positive blood culture but does not meet a major criterion as noted above or serological evidence of active infection with organism consistent with IE. 7. Treatment – will discuss empiric coverage only – need ID consult and specific recommendations when organism isolated. A) Native valve, no h/o IVDU: obtain 3 sets of blood cultures over 24 hours; vancomycin plus synergistic gentamicin dosing (1 mg/kg q 8 hours); other option is ampicillin (for enterococcus) + nafcillin + synergistic gentamicin. B) IVDU or R-sided endocarditis: vancomycin C) Prosthetic valve: vancomycin, gentamicin (1mg/kg q 8 h), plus rifampin 300 mg po q 8 hours. D) Obtain CT surgery consult for the following: prosthetic valve, any S. aureus IE, evidence of heart failure, valvular dysfunction, persistent fever for 10 days while on appropriate antibiotics, new EKG conduction abnormalities, fungal IE, recurrent embolic events, abscess, highly resistant organism, persistent bacteremia on appropriate antibiotics (rule out metastatic infection), relapse after completion of therapy. E) Duration of antibiotics dependent on organism/resistance profile – average is 6 weeks. 8. Complications/associated clinical syndromes A) Mycotic aneurysms (cerebral vessels, abdominal aorta, splenic, coronary, pulmonary vessels). B) Cerebral emboli: seen in 20% of cases, MCA most common C) Splenic infarctions D) Glomerulonephritis (seen in 40-80% of cases) and renal abscesses E) Skin lesions – Osler nodes, janeway lesions, petechiae, splinter hemorrhages F) Pulmonary septic emboli in right sided lesions G) Septic emboli can involve virtually every organ system Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111). 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle). 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern Medical student