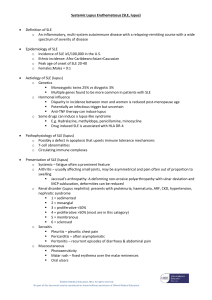
Rheumatology 9 – Systemic Lupus Erythematosus
advertisement

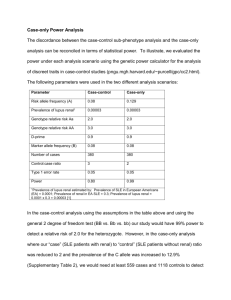
Rheumatology 9 – Systemic Lupus Erythematosus Anil Chopra 1. 2. 3. 4. 5. 6. Epidemiology of SLE including genetic predisposition. Understand principles underlying pathogenesis of SLE. To be able to describe the clinical features of SLE. To understand the means by which SLE is diagnosed. To understand basic principles involved in treatment of SLE. To understand the concept of a spectrum of connective tissue diseases. Systemic Lupus Erythematosus is one condition of a family of overlapping autoimmune diseases which includes rheumatoid arthritis, systemic sclerosis e.t.c. Chronic Autoimmune disease - Incredibly rare (3 in 10 000) - More common in women (male: female ratio is 1:9) - Disease of young people (generally after puberty) - Increased incidence from Afro Carribean, Asian. - Disease of skin and joints - Can also affect lungs, kidney, bone marrow. Clinical Features - malaise - fever - fatigue - weight loss - lymphadenopathy Specific Features - butterfly rash (sparing of nasolabial folds) - alopecia (increased loss of hair) - arthralgia (joint pain) - Raynaud’s phenomenon (discolouration of fingers and toes) - Vasculitis (a.k.a. angiitis) Other Features - Inflammation of the kidney, heart, lungs, - Accelerated atherosclerosis - High levels of immune cells/complement in biopsy - Antiphospholipid syndrome – disorder of coagulation resulting in thrombi Pathogenesis The main player in the pathogenesis of SLE is the Bcell. It occurs when apoptotic debris is insufficiently cleared, resulting in uptake of autoantigens and B-cell mediated immune response. IgG autoantibodies are produced and immune complexes are formed. Diagnosis The 1982 ARA criteria are used to diagnose SLE. SLE can be diagnosed if 4 out of the 11 criteria below are present… Malar rash. Discoid rash. This is a rash that occurs in discoid lupus erythematosus (DLE) which is basically a milder form of SLE. In DLE, only the skin is affected (i.e. a discoid rash is present, but there is no progressive damage to the kidneys, heart or lungs etc.). Photosensitivity. Oral ulcers. Arthritis. Serositis (inflammation of a serous membrane, such as the lining of the thoracic cavity (pleura)). In SLE, serositis causes either pleuritis and/or pericarditis. Renal disorders may be present and can be diagnosed with many tests. For example, proteinuria can be diagnosed by taking urine samples for 24 hours. If more than 0.5g of protein is passed, proteinuria can be diagnosed. Neurological disorders such as seizures or psychosis may be present. Haematological disorders may occur. Immunologic disorders such as anti-dsDNA antibodies may be present. A titre may reveal a raised antinuclear antibody level. The main form Homogenous Speckled of diagnosis is the antinuclear antibody test, SLE however this is nonspecific. The pattern is important. Scl Nucleolar Fine speckled SLE Overlap syndrome s CREST Homogenous – this is where the ANAs present bind to DNA (the double-stranded helix). This type of staining is characteristic in SLE. Speckled – here the ANAs bind to Ro*, La*, Sm*, and RNPs. This type of staining is characteristic in SLE, but may be due to other syndromes as well as SLE, and it is possible to have this pattern of staining in patients who do not have SLE. Nucleolar – here the ANAs bind to topoisomerase – this is characteristic of scleroderma. Centromere – this pattern of staining is characteristic of limited cutaneous scleroderma. *Ro, La, and Sm are nuclear ribonucleoproteins (which are important in RNA processing) Other tests include: Assess complement consumption. (increased complement consumption SLE). Anti cardilolipin antibodies. Lupus anticoagulant β1 glycoprotien Raised urea and creatinine level Renal-related tests which may also suggest presence of SLE… Proteinuria (the presence of abnormally high levels of protein in the urine) may lead to protein loss (and even deficiency in severe cases). Therefore, the patient may have a low serum albumin level, for example. Haematuria (the passage of blood in the urine). This may be as a result of kidney inflammation which is commonly caused by SLE. Active urinary sediment is very important as it is will offer a poor prognosis for the patient. It is the presence of clumps of red and white blood cells in the urine. It probably occurs with severe inflammation of the kidneys associated with SLE. Haematological tests: looking for Lymphopaenia – low lymphocytes Normochromic anaemia – anaemia where Hb is within normal range Leukopaenia – low white blood cell AIHA – autoimmune haemolytic anaemia Thrombocytopaenia – low platelet count Severity In SLE, it is important to assess the severity of the disease as it affects the course of treatment administered. The most important assessments are… 1. Identifying the pattern of organ involvement. 2. Monitoring function of the affected organs… – Renal: the blood pressure is monitored (an uncontrolled blood pressure in young people leads to a poor prognosis for the patient as renal failure will be advanced if this occurs), urea and electrolyte levels are recorded, as is the urine sediment. – Heart and lungs: echocardiography is performed to monitor the heart for any changes, and lung function testing is important for the patient as progression of the disease may lead to the patient becoming short of breath. – The skin should be assessed for the advancing of the rash. – The eyes should also be assessed for visual problems which are common with autoimmune inflammatory diseases (such as conjunctivitis in reactive arthritis). – The blood (haematological) tests are important to pick up on several problems with the organs (such as proteinuria with renal failure), and also blood disorders such as normochromic anaemia. 3. Identifying the pattern of autoantibodies expressed is important to identify episodes of SLE flaring, and also various other problems that may occur… – Anti-dsDNA, anti-Sm, and anti-C1q are important as they predispose to renal disease. – Anti-cardiolipin antibodies are important as they predispose to thrombosis. Prediction of Disease Markers Clinical Features Wt loss, fatigue, malaise, hair loss Alopecia Rash Laboratory markers ESR Increased complement consumption (therefore complement deficiency) Increased anti-dsDNA Other Abs e.g ANA and CRP poor indicators NB: Lupus patients have RAISED ESR but normal CRP. HLA B8, DR2, and DR3 are also involved Treatment - Depends on severity. MILD – joint and possible skin involvement Paracetemol + NSAID. Hydroxychloroquine Topical corticosteroids. MODERATE – inflammation of other organs Oral corticosteroids with IV methylprednisolone SEVERE – severe inflammation of vital organs (nephritis, CNS disease, Cardiac pulmonary disease) Azathoiprine (immunosuppression) Cyclophosphamide. Mycophenolate mofetil Rituximab Prognosis and survival of SLE SLE is a life-threatening disease, but early diagnosis and effective treatment can offer the patient a good long-term prognosis. The 15-year survival rate if the patient has no nephritis is 85%, in patients who do have nephritis; the rate is reduced to 60%. However, the prognosis is further worsened if the patient is black, male, and has a low socio-economic status.