RHEUMATOLOGIC EMERGENCIES
advertisement
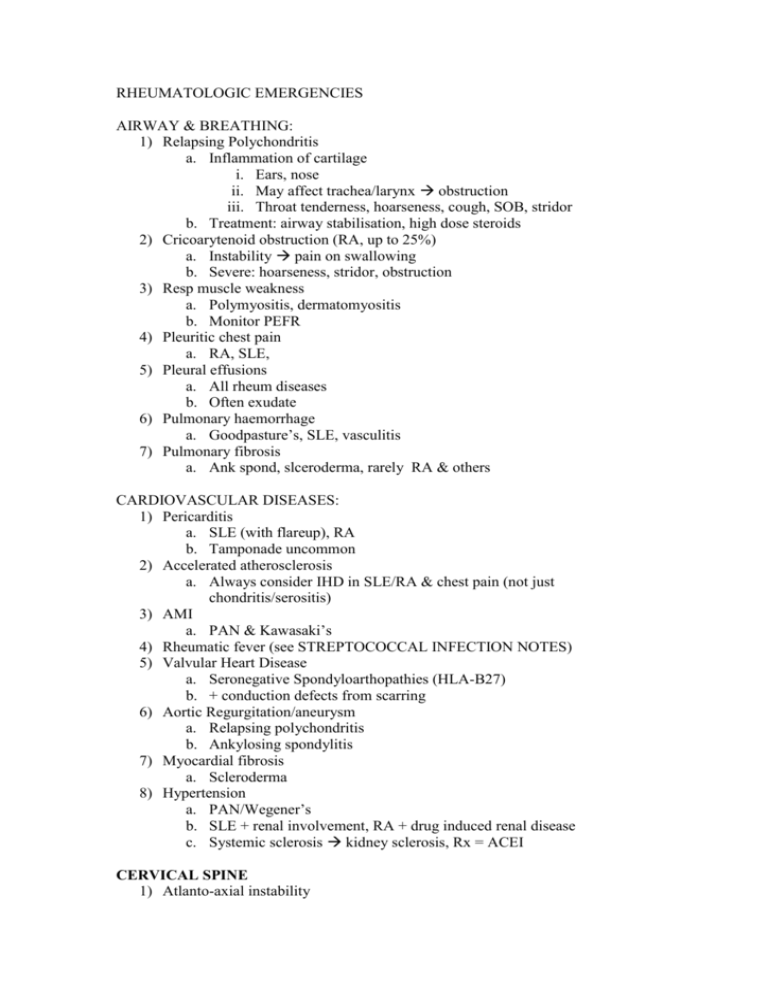
RHEUMATOLOGIC EMERGENCIES AIRWAY & BREATHING: 1) Relapsing Polychondritis a. Inflammation of cartilage i. Ears, nose ii. May affect trachea/larynx obstruction iii. Throat tenderness, hoarseness, cough, SOB, stridor b. Treatment: airway stabilisation, high dose steroids 2) Cricoarytenoid obstruction (RA, up to 25%) a. Instability pain on swallowing b. Severe: hoarseness, stridor, obstruction 3) Resp muscle weakness a. Polymyositis, dermatomyositis b. Monitor PEFR 4) Pleuritic chest pain a. RA, SLE, 5) Pleural effusions a. All rheum diseases b. Often exudate 6) Pulmonary haemorrhage a. Goodpasture’s, SLE, vasculitis 7) Pulmonary fibrosis a. Ank spond, slceroderma, rarely RA & others CARDIOVASCULAR DISEASES: 1) Pericarditis a. SLE (with flareup), RA b. Tamponade uncommon 2) Accelerated atherosclerosis a. Always consider IHD in SLE/RA & chest pain (not just chondritis/serositis) 3) AMI a. PAN & Kawasaki’s 4) Rheumatic fever (see STREPTOCOCCAL INFECTION NOTES) 5) Valvular Heart Disease a. Seronegative Spondyloarthopathies (HLA-B27) b. + conduction defects from scarring 6) Aortic Regurgitation/aneurysm a. Relapsing polychondritis b. Ankylosing spondylitis 7) Myocardial fibrosis a. Scleroderma 8) Hypertension a. PAN/Wegener’s b. SLE + renal involvement, RA + drug induced renal disease c. Systemic sclerosis kidney sclerosis, Rx = ACEI CERVICAL SPINE 1) Atlanto-axial instability 2) 3) 4) 5) a. RA b. Atlanto-dental distance >3.5mm c. May get overt cord injury d. Or: subtle signs: bowel/bladder changes, weakness, paraesthesia e. NB: Strength may be difficult to assess in RA – REFLEXES best clue Fracture with minor trauma a. Espec Ank Spond Transverse myelitis a. SLE Spinal vascular issues (infarcts, dissection) a. Vasculitis AIRWAY ISSUES: a. RA: assume instability – manual in line stabilisation, most experienced operator OPHTHALMOLOGICAL 1) TEMPORAL ARTERITIS a. Vasculitis of thoracic aorta & branches b. Age > 50 c. Occurs in 30% with PMR i. PMR: Unexplained anaemia, fatigue, prox limb pain d. Symptoms: i. Headache ii. Scalp Tenderness iii. Jaw/tongue/upper extremity claudication iv. Fluctuating vision v. Diminished or lost brachial pulse e. Investigations i. ESR > 50mm/hr ii. CRP > ____ (additive sensitivity) f. NB Visual changes: prodromal Syx usually present prior to permanent damage/blindness g. Diagnosis i. Biopsy h. Treatment: Prednisolone i. START PRIOR TO BIOPSY (biopsy unaffected if done < 1 week of treatment) 2) SJOGREN’S SYNDROME a. Lymphocytic infiltration of lacrimal & salivary glands b. Can occur alone or as Cx of Rheum diseases c. Complications: i. Corneal ulceration +/- infection 3) SCLERITIS = very rare a. Severe RA/Vasculitis (& IBD) b. Exquisite occular tenderness/pain, deep, boring pain c. Pain not relieved by topical LA d. Eye looks more BLUE du to thin sclera e. Urgent referral – can rupture 4) EPISCLERITIS a. More common, less serious, self limiting, painless, pink-red RENAL 1) ANY Rheumatic disease can cause kidney damage (& treatments) 2) GN: a. SLE, Wegener’s i. Haem/proteinuria & HT present before Ur/Cr b. Scleroderma (as above) 3) RHABDO (& ARF) a. Polymyositis flare 4) MEDICATION: a. NSAIDS