outline24077 - American Academy of Optometry
advertisement

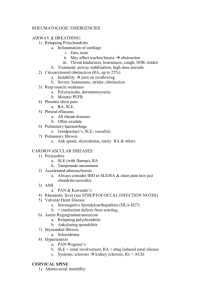
Greg Black and Julie Tyler 881 Camellia Court Plantation, FL 33317 Cell (954) 815 2020 Ocular Manifestations of Rheumatoid Diseases I. Rheumatic diseases- Characterized by inflammation and loss of function of one or more connecting or supporting structures of the body A. Joints, tendons, muscles, ligaments and bones typically affected with extra-articular manifestations B. Pain, swelling and stiffness are common symptoms C. Over 100 rheumatic diseases some with ocular manifestations 1. Rheumatoid arthritis 2. Systemic lupus erythematosus 3. Scleroderma 4. Juvenile rheumatoid arthritis 5. Spondyloarthropathies II. Rheumatoid Arthritis- a chronic, progressive inflammatory disease with several ocular associations A. Periods of exacerbations and remissions B. Incidence 1. In the United States, RA is found in approximately 1% of the adult population 2. Peak incidence between the fourth and sixth decades 3. Prevalence rate about 2.5x greater in women than men C. Etiology 1. Specific etiology of RA is unidentified 2. Current theory suggests a genetic predisposition involving multiple genes that are initiated by an unknown trigger(s) 3. An association with female sex hormones has been postulated D. Disease Process 1. Onset of RA is usually insidious over a period of weeks to months 2. Primary (but not solitary) target of the abnormal immune response in RA is the synovial membranes and articular structures 3. RA progresses from swelling of the synovial lining to synovial thickening and finally resulting in deformity of the joints 4. Common extra-articular manifestations include rheumatoid nodules, ocular disease, Sjögren’s syndrome, rheumatoid vasculitis and neurologic disease E. Common symptoms 1. Symmetrical stiffness in multiple joints 2. Morning stiffness greater in duration than one hour 3. Generalized fatigue F. Clinical Signs 1. Joint swelling 2. Tenderness G. Ocular Manifestations 1. Approximately 25% of patients with RA will report ocular manifestations 2. Keratoconjunctivitis sicca (KCS) a. Combination of inflammation of the lacrimal gland and meibomian gland dysfunction b. Ocular findings include conjunctival staining, punctate epithelial keratitis (PEK), diminished tear meniscus and decreased tear break-up time. 3. Episcleritis - Inflammation of the tissue overlying the sclera 4. Scleritis - Inflammation of the sclera including the presence of scleral edema 5. Keratitis - Peripheral corneal ulceration H. Making the Diagnosis 1. Diagnosis is made based on the 1987 criteria for the classification of RA 2. Based on medical history, physical examination, serology, and imaging studies 3. Serologic testing consists of a complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein and rheumatoid factor (RF) I. Treatment 1. Dependent on the individual and severity of disease 2. First-line medications, NSAIDS and corticosteroids 3. Second-line medications, disease-modifying antirheumatic drugs (DMARDs) suppress the immune system and inhibit the loss of cartilage and bone, while biologic response modifiers (BRMs) influence the activity of cytokines. 4. Consideration of Hydroxychloroquine III. Systemic Lupus Erythematosus (SLE) A. SLE Qualities 1. Considered an “imitator” disorder because its symptoms and clinical course vary widely and mimic other conditions 2. Chronic autoimmune inflammatory disease can affect the skin, kidneys, joints, nervous system, blood, eyes and other organs B. Incidence, Prevalence and Mortality 1. In the U. S., SLE prevalence is approximately 1 in 2,000, and frequency varies by ethnicity. 2. SLE is also two to three times more prevalent in nonwhites, including blacks, Asians, Hispanics and Native Americans 3. An estimated 1.5 million Americans have some form of lupus. 4. Peak incidence: 80% develop SLE between ages 15 and 45 5. Predominant among females (90% are female) 6. Five-year survival rate of patients has increased from 50% in the 1950s to between 91% to 97% today 7. Mortalitiy rates are higher among SLE patients who develop infectious complications, seizures, lupus nephritis and renal failure. C. Etiology 1. Complex disease with an unknown etiology a combination of genetic, environmental and hormonal factors that are initiated by a trigger a. Trigger may be bacterial infection b. Trigger may be viral infection 2. Flares are also associated with periods of significant hormonal changes, such as pregnancy and initiation of hormone replacement therapy. D. Disease Process 1. Patients initially experience a flu-like syndrome: including fatigue, fever, weight loss, and muscle & joint pain 2. The pathology of SLE consists of vascular abnormalities and inflammation. 3. Vascular abnormalities and inflammation lead to immune complex deposition, occlusive vasculopathy and vasculitis 4. As SLE progresses, complications become more diverse and severe E. Common symptoms 1. Initial flu-like syndromePatients initially experience a flu-like syndrome, including fatigue 2. Fatigue, fever, weight loss, and muscle and joint pain F. Clinical Signs 1. Malar Rash 2. Alopecia G. Ocular Manifestations 1. Ocular complications of SLE are variable 2. Ocular findings occur more frequently in patients who have concurrent systemic disease 3. Conditions: a. Keratoconjunctivitis Sicca (KCS) – combination of inflammation of the lacrimal gland and meibomian gland dysfunction b. Episcleritis – Inflammation of the tissue overlying the sclera c. Scleritis – An indicator of significant, concurrent SLE d. Uveitis – Initially tends to present as acute, bilateral and non-granulomatous iridocyclitis e. Vacular occlusive disease 1) Retinal vein occlusion 2) Retinal artery occlusion f. Retinopathy 1) Hemorrhages 2) Candle wax dripping 3) Cotton wool spots H. Making the Diagnosis 1. Diagnosis is made based on the presence of at least four of eleven diagnostic criteria established by the American College of Rheumatology a. Symptoms DO NOT need to be concurrent 2. Serologic testing may be beneficial but is not necessary for diagnosing 3. Lab tests may help in the diagnosis and be monitored for management I. Treatment 1. Currently there is no cure for SLE - goal of therapy is: a. Alleviate symptoms b. Prolong remissions c. Reverse immune dysregulatoin d. Prevent organ damage 2. First-line drugs include NSAIDs and corticosteroids 3. Second-line drugs include disease-modifying antirheumatic drugs (DMARDs), and biologic response modifiers (BRMs) IV Sjogren’s Syndrome A. A multi-factoral, chronic inflammatory condition resulting in lymphocytic infiltration of the lacrimal and salivary glands resulting in xerophthalmia and xerostomia respectively a. Dry eyes (KCS) b. Dry mouth c. Accompanied by associated, specific systemic conditions, including SLE B. Other conditions associated with Sjogren’s syndrome autoimmune disorders that compromise lacrimal system a. Rheumatoid arthritis (RA) b. Systemic sclerosis c. Psoriatic arthritis d. Hashimoto’s thyroiditis e. Juvenile chronic arthritis C. Ocular complications and treatment a. Filamentary keratitis b. Medications i. Artificial tears ii. Restasis iii. Topical steroids iv. Neutraceuticals and others Reference: Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988 Mar;31(3):315-24. Tan EM et al. The 1982 Revised Criteria for the Classification of SLE. Arth Rheum 1982;25: 1271-1277. Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus [letter]. Arth Rheum 1997;40:1725. Black GS, Tyler JA. Lessons on Lupus in the Eye. Review of Optometry 2006; 143(4):59-66. Black GS, Tyler JA, Kabat AG. Arthritis as Seen Through the Eyes. Review of Optometry 2006; 143(1):39-45.