Result of Protodioscin (Tribulus terrestris) treatment in
advertisement

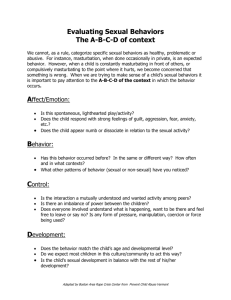
Result of Protodioscin (Tribulus terrestris) treatment in males diagnosed with infertility and impotence K.M. Arsyad Medical Biology Division of Andrology, University of Sriwijaya, Indonesia (1996) SUMMARY Libilov treatment consisting of oral administration of 3 x 1 to 3 x 2 tablets / day for 14 to 60 days was shown to be effective in improving the concentration and quality of spermatozoa in patients with oligozoospermia. Furthermore, the treated men also reported improvement in sexual libido, erection, ejaculation and orgasm. Libilov treatment also resulted in improved spermatogenesis in the Sertoli and germinal cells, and increased the efficiency of testosterone conversion to dihydrotestosterone (DHT). As DHT played an important role in the improvement of red blood cell formation (erythropoiesis) as well as muscle development, this contributed to the sense of physical well-being and improved oxygen circulation in the body. Indirectly, these effects also added to the improvement in sexual functions, including libido, erection, and orgasm. INTRODUCTION Protodioscin is the active ingredient found in the extract of the plant Tribulus terrestris L., available under the tradename Libilov™. This herbal plant has been traditionally used in Asian and European countries to treat infertility and impotence (Viktorof et al. 1994). Male fertility is defined as a man's ability to impregnate his spouse or partner, leading to a successful birth within the first twelve months of continuous effort to conceive. In contrast, the inability of the male to achieve conception is defined as male infertility. In primary male infertility, it is the woman's first time trying to conceive. On the other hand, if a man has successfully impregnated the woman in the past, leading to a normal pregnancy, or spontaneous or intentional abortion, but is currently unable to impregnate his wife successfully within one year of effort, then his infertility is characterized as secondary infertility (Rowe et al. 1993). Generally defined, impotence is a collection of sexual dysfunctions that can be manifested as reduction in sexual drive, desire or libido, penile erection, ejaculation or even the ability to achieve orgasm. As impotence can occur in all sexual response phases, we can classify impotence as follows (Susilo 1994, Adimoelja 1985, Barry and Hodges 1987, Ellenberg 1971): 1. Impotensia libidinis or impotensia concupiciency ( manifests as lowered sexual drive) 2. Impotensia erectionis (the inability to achieve or maintain penis erection for normal sexual intercourse) 3. Impotensia ejaculationis (involves ejaculation dysfunctions, which includes premature, retarded, retrograde, incomplete ejaculations and non-ejaculations) 4. Impotensia satisfactionis / emotionis (manifests as unsatisfactory orgasm or inability to reach orgasm during sexual intercourse) Here, we review the mechanism of how protodioscin treatment works, as well as the result of Libilov clinical trials on male subjects diagnosed with either impotence or infertility. CLINICAL ACTION OF PROTODIOSCIN ON THE MALE REPRODUCTIVE SYSTEM In comparison to currently available treatments for infertility and impotence, protodioscin has been shown to be more efficient, less costly, and more importantly, to carry significantly less risk of unwanted side-effects. The rapid development of Libilov, a non-hormonal and natural herbal preparation of Tribulus terrestris L., was accompanied by intensive clinical and laboratory tests. Based on those tests, we conclude that Libilov provides an effective viable alternative in treating male impotence and infertility. Chemical and Physical Characteristics of Protodioscin Protodioscin is the active ingredient of the plant extract of Tribulus terrestris L., and is produced by PT Teguhsindo Lestaritama, Indonesia. Protodioscin is classified as a furostanol saponin, and is present in the extract at no less than 45% of the total weight. The chemical structure of this compound is shown below in Figure 1. Figure 1. The chemical structure of protodioscin, the active ingredient of Tribulus terrestris L. extract. Protodioscin is physically characterized as a bitter-tasting amorphous powder, with a yellow-brown color. It is soluble in water, slightly soluble in methanol, but not soluble in chloroform. Gonadal steroid Three male sex steroids or androgens, namely testosterone, dihydrotestosterone and estradiol, are important for the male reproductive system (Greenspan 1991). From a quantitative perspective, the most important androgen is testosterone. More than 95% of this hormone is produced by Leydig cells, with the rest produced by the adrenal glands. To supplement testosterone, the testes also produces a small amount of potent form of androgen called dihydrotestosterone (DHT), as well as weaker forms such as dehydroepiandrosterone (DHEA) and androstenedione. These cells also secrete a small quantity of estradiol (E), estrone, pregnenolone, and progesterone, and 17-alphahydroxyprogesterone. In addition to their production in testes, DHT and E are also produced by the breakdown of androgens in the peripheral circulatory networks. The biosynthetic steps of androgen in the testes is diagrammed in Figure 2. The contribution of testes, adrenal and peripheral networks on the serum level of the male sexual steroids is shown in Table 1. Figure 2. The biosynthetic steps of androgen production in the testes. Testes Secretion Adrenal Secretion Peripheral Conversion Testosterone 95 <1 <5 Dihydrotestosterone 20 <1 80 Estradiol 20 <1 80 Estrone 2 <1 98 < 10 90 - Androgen DHEA-Sulphate Table I. The contribution of testes adrenal secretion and peripheral network conversion on the total level of androgens in the bloodstream. Values are in percent. In the bloodstream, androgen and estrogen are either in free form, or are in a form bound to serum proteins. Although approximately 38% of bound testosterone is bound to albumin, its major binding partner is the Sex Hormone Binding Globulin (SHBG), which associates with more than 60% of bound testosterone. SHBG is different from the Androgen Binding Protein (ABP), which is synthesized by the heart and the Sertoli cells, as SHBG level can be increased by treatment with estrogen or thyroid hormones, or by medical conditions of hyperthyroidism and hepatic cirrhosis. Conversely, treatment with growth hormone, or condition of hypothyroidism, acromegaly or obesity can lower the level of this protein. Approximately 20% of testosterone in the bloodstream is in the unbound or free form. This form of testosterone is free to enter and metabolically affect cells. In addition to the level of the free form, the bioavailability of testosterone is also influenced by the dissociation of testosterone from its binding proteins. The majority of testosterone is converted in the heart into metabolites such as androsterone and eticholanolone, which are secreted in the urine after they react chemically with glucoronatic or sulfuric acid into 17-keto-steroid. However, since this is not the major source of 17-ketosteroid, simple measurement of this compound in the urine does not provide an accurate picture of testes steroid production. Moreover, this measurement would also not be able to detect the small amount of testosterone that is converted into a specific form of androgen called dihydrotestosterone (DHT) in specific target tissues. In the majority of target cells, some testosterone is enzymatically converted into DHT by the microsomal enzyme 5-alpha-reductase. Similar to testosterone, DHT is then bound by an intracytoplasmic receptor protein specific for it (becoming DHT-Rc, Figure 3). After the DHTprotein complex formation, the bound hormone is transported into the nucleus (becoming DHT-Rn, Figure 3). There the protein complex undergoes a conformational transformation, which is thought to involve chromatin binding. This results in mRNA syntheses, and subsequently in syntheses of cytoplasmic proteins, which lead to cell growth and other secondary effects mediated by androgens (Figure 3). Figure 3. The mechanism of the androgen's action. Free testosterone is transported into the cell and some is converted to dihydrotestosterone (DHT). Cytoplasmic receptors (Rc) bind these molecules, which are subsequently transported into the nucleus. These protein-hormone complexes (DHT-Rn, T-Rn) activate transcriptions of androgen-sensitive genes, resulting in the production of transcript mRNAs. These mRNAs are transported to the cytoplasm and are translated into proteins responsible for the androgen's action. The biological effects of androgens in males include the appropriate fetal differentiation of the internal and external tissues which comprise the male genitalia. During puberty, androgens act to stimulate the development of the scrotum, epididymis, vas deferens, seminal vesicles, prostate, and penis tissues development. The functional integrity of these organs also depends on the androgen levels. Furthermore, androgen also induced larynx and muscle developments, which lead to the development of secondary sexual characteristics. The ambi-sexual development of pubic and armpit hair, as well as the male-specific development of facial, chest, abdomen, and back hairs are induced by the stimulation of the sebaceous glands with androgen. Other effects of androgens include stimulation of erythropoiesis, as well as psychological and behavioral changes. Mechanism of Protodioscin Protodioscin acts by stimulating the enzyme 5-alpha-reductase, which plays a role in the conversion of testosterone into dihydrotestosterone (Viktorof et al. 1994). In addition, protodioscin also stimulates the hypothalamus secretion of luteinizing hormone (LH), but not of follicle stimulating hormone (FSH). Protodioscin is shown to increase the density of the Leydig, but not that of the Sertoli cells, and to improve the level of spermatogonia and to increase the production of spermatocytes and spermatids without changing the diameter of the seminiferous tubules. Physically, protodioscin treatment results in increased male fertility and sexual functions. In respect to improving fertility, protodioscin increases the level of spermatogenesis by stimulating the Sertoli and germinal cells, resulting in the increased production of sperms. In this process, protodioscin improves the conversion of testosterone to DHT, which in turn stimulates the production of Androgen Binding Protein (ABP) in the Sertoli cells. Increased ABP production results in increased formation of DHT-ABP complex, which stimulates spermatogenesis in the germinal cells. Another fraction of the DHT-ABP complex is transported to the epididymis, which increases the efficiency of the maturation of spermatozoa into fertile sperms. In respect to increasing sexual functions, protodioscin works by increasing the conversion of testosterone into the potent DHT(Figure 4). In addition to the increase in sexual drive or libido, DHT also stimulates erythropoiesis or production of red blood cells, and muscle developments, thus contributing to the improvement of blood circulation as well as the oxygen transport systems. Importantly, regular use of protodioscin has also been shown to increase the duration of penile erection and improve ejaculation in males. Figure 4. The mechanism of protodioscin's action. Protodioscin increases the production of serum testosterone and the conversion of testosterone to dihydrotestosterone. Dihydrotestosterone, in turn enhances erythropoiesis and muscle development. More erythropoiesis or production of red blood cell increases the hemoglobin level, which results in better oxygen transport throughout the body, resulting in a more optimal health. Both increased production of testosterone and better health contribute to the increase in sexual functions, especially the increase in sex drive. Fertility and the Male Sexual Potential Male fertility is clinically quantified by laboratory analyses of semen. The normal boundaries are determined by the World Health Organization in 1992 as described in Table 2. Male sexual dysfunctions are listed in Table 3. Parameter Value Volume > 2.0 ml pH 7.2 - 7.8 Sperm concentration > 20 million sperms / ml Sperm concentration / ejaculate > 40 million sperms / ejaculate Motility > 50% progressively motile category (a+b); or >25% rapid progressively motile (a) within 60 minutes of ejaculation Morphology > 30% with normal morphology Vitality > 70% viability, i.e. without supravital color Leukocyte cells < 1 million / ml Immune droplet test Binding to less than 20% of sperms MAR test Binding to less than 10% of sperms Other tests: alpha-glucosidase zinc citric acid phosphatase fructose > 20 mU / ejaculate < 2.4 µmol /ejaculate >52 µmol / ejaculate >200 U / ejaculate >13 µmol / ejaculate Table II. Parameter of semen analyses as determined by the World Health Organization (1992). Nomenclature Definition Normozoospermia Normal ejaculation based on concentration, mobility and morphology of sperms Oligozoospermia Concentration of sperm < 20 million / ml Severe oligozoospermia Concentration of sperm < 3 million / ml Asthenozoospermia Mobility < 50% (a+b) or grade a mobility < 30% Teratozoospermia Normal morphology < 30% Oligoashtenoteratozoospermia Defects in concentration, mobility and morphology of sperms Azoospermia No sperm in ejaculate Aspermia No ejaculate Hemospermia Red blood cells in ejaculate Pyospermia White blood cells in ejaculate at concentration > 1 million / ml Table III. Nomenclature of sexual dysfunctions based on semen analyses. Male infertility can be diagnosed by routine semen analyses or by causative etiology (Comhaire 1991, Adimoelja 1990, Lee 1983, Kolodny et al. 1979). In a routine semen analyses, abnormal semen volume (hypo- or hyperspermia), abnormal sperm concentration such as polyzoospermia (<25 million sperms / ml), oligozoospermia (<20 million sperm / ml), and abnormal sperm quality, such as asthenozoospermia or defect in motility, and teratozoospermia or defect in morphology, can be detected. Some of these disorders, such as oligozoospermia and abnormal sperm qualities, can be treated either by medication or by artificial insemination. Causative etiology allows doctors to distinguish infertility that are treatable, such as that caused by varicocele, accessory glands infections, immunological factors, psychological dysfunctions and endocrinopathy from those that are currently not treatable such as Klinefelter's syndrome, bilateral cryptorchidism, testes atrophy, Sertoli only syndrome and vas deferens agenesis. MALE SEXUAL FUNCTION In order to understand the male sexual function, we need to understand the male sexual response and mechanism of penile erection. Sexual Response Phases There are four sexual phases in both males and females (Kolodny et al. 1979): 1. Excitement phase This is the first sexual phase, reached after physical or psychological sexual attraction or excitement. In males, this also takes the form of penis erection. 2. Plateau phase In this phase, sexual excitement reaches a high level. This level, however, is below the level required for orgasm. In this phase, the proximal penis glands increase in size and fluid that may contain live spermatozoa is secreted from the bulbourethral (Cowper's) glands. 3. Orgasmic phase Orgasm is the apex of sexual activity, and includes both physical and psychological factors. This phase is triggered by a neural reflex arc once the degree of excitement, or the discharge of semen due to the cooperative contraction of the urethra, penis and the prostate glands, occurs. 4. Resolution phase After orgasm and ejaculation, males enter a resolution phase. In this phase, ejaculation does not take place, although sometimes erection can occur. Anatomic and physiological changes in the genitalia organs take place to reset the reproductive systems to pre-sexual excitement phases. Mechanism of Penile Erection The physiology of penile erection mechanism, according to Watterauer (1988), is divided into the following phases: 1. Sinusoid phase In this phase, relaxation of the corpus cavernosum blood vessels results in the elongation of the penis. 2. Arterial phase Blood flows into penis arteries, resulting in increased volume of the cavernosum until passive pressures stop the blood flow out of the veins. This internal pressure in the cavernosum cavities causes stiffening of the penis. 3. Vein phase In this phase, erection is achieved due to increased blood flow resistance in the capillaries of the penis. 4. Muscle phase Increased bulbocavernosum and ischiocavernosum muscles activities result in penile blood pressure much higher than that of the systolic pressure. In this phase, penile erection reaches its maximum. 5. Resistance phase In this phase there is increased sinusoidal muscle contraction that causes blood to flow out of the penis. The penis begins to lose stiffness and length. Therapies for all classes of impotence include sexual counseling, sex therapy, mechanical options, surgeries, and pharmacological treatments (Susilo 1994). RESULT AND DISCUSSION OF LIBILOV TREATMENT Male Infertility Male infertility can manifest in many forms, including abnormalities in sperm concentration and quality. The result of Libilov treatment for infertility are discussed below. 1. Spermatozoa concentration Viktorof et al. (1994) reported a significant increase in the spermatozoa concentration. Oligoasthenozoospermic patients were given a dose of 3 x 1 tablet / day for 60 days. Varicocelectomy patients were given 3 x 1 to 3 x 2 tablets / day for 60 days. Moeloek et al. (1994) reported an increase in the sperm concentration in patients diagnosed with oligozoospermia. These patients were given Libilov at a dose of 3 x 2 tablets / day for 9 weeks. Arsyad (1996) reported that 3 x 2 tablets / day treatment of Libilov for 60 days given to patients with idiopathic, moderate oligozoospermia resulted in almost doubling of the spermatozoa concentration. This increase in sperm concentration continued for 30 days post-administration of the herbal preparation. 2. Spermatozoa quality Moeloek et al. (1994) reported morphological, but not motility improvement in patients diagnosed with oligozoospermia after treatment with Libilov at 3 x 2 tablets / day for 9 weeks. Viktorof et al. (1994) reported an increased spermatozoa motility. In this study, oligoasthenozoospermic patients were given protodioscin tablets at 3 x 1 tablet / day for 60 days. Patients diagnosed with varicocele were given 3 x 1 to 3 x 2 tablets / day for 60 days. Arsyad (1996) reported that 3 x 2 tablets / day for 60 days in patients with moderate idiopathic oligozoospermia results in increased motility and improved spermatozoa morphology in all patients. This improvement continued for 30 days post-administration of the treatment. Impotence Impotence can manifest itself in all phases of the sexual response. Its most common forms are decreased sexual libido and erection, and impairment in ejaculation and orgasm. According to Pangkahila (1993), patients diagnosed with non-organic sexual dysfunctions treated with Libilov 3 x 2 tablets / day for 90 days reported significant increase in sex drive. Nasution (1993) reported that patients diagnosed with libidinal and erectionic impotence treated with 3 x 1 tablets / day for 14 days showed significant improvement in libido and erection without any side-effects. Finally, in Arsyad (1996), 33% of patients with moderate idiopathic oligozoospermia treated with Libilov at 3 x 2 tablets / day dosage reported improvement in sex drives within 30 days. This number increased to 80% by day 60 of treatment. After only 30 days of treatment, penis erection was improved in 53% of the patients. Likewise, this increased to 87% of patients after 60 days of treatment. Better ejaculation was experienced by 47% and 67% of patients after 30 and 60 days of treatment, respectively. Importantly, orgasm was improved in 40% of males after 30 days of treatment. This increased to 87% after 60 days. DISCUSSION The increase in the concentration, mobility and morphology of spermatozoa after treatment with Libilov (protodioscin) can be expected from what we know of its mechanism of action. Here, protodioscin treatment results in improved spermatogenesis in the Sertoli and germinal cells. Furthermore, protodioscin results in increased efficiency of testosterone conversion to DHT. This results in the stimulation of the Sertoli cells to produce Androgen Binding Protein, which binds to DHT and improves the function of the epididymis tissues in spermatozoa maturation. Protodioscin also increased the secretion of luteinizing hormone that subsequently induced Leydig cells to produce testosterone (Greenspan 1991). The increase in the level of DHT, the most potent form of androgens, is also an important mechanism of protodioscin treatment. DHT plays an important role in the improvement of red blood cell formation as well as muscle development. This contributes directly to the sense of physical well-being and improves oxygen circulation in the body (Greeenspan 1991). Indirectly, these effects also adds to the improvement in sexual functions, including sexual libido, erection, ejaculation and orgasm. SUMMARY In this report we discussed male fertility and sexual functions, as well as the mechanism of action of protodioscin or Libilov treatment. We also briefly reviewed results of protodioscin treatment in males diagnosed with infertility and impotence. Generally, Libilov treatment consists of oral administration of 3 x 1 to 3 x 2 tablets / day for 14 to 60 days. This regiment has been successfully shown to be effective in improving the concentration and quality of spermatozoa in patients with oligozoospermia. Furthermore, these men also report improvements in sexual libido, erection, ejaculation, and orgasm after Libilov treatment. REFERENCES Adimoelja A. Male infertility. Scientific IDI Meeting in Surabaya, Indonesia (1985). Adimoelja A. Infertility therapy for men. National Congress of Indonesian Association of Andrology Scientific Symposium VIII in Padang (1990). Arsyad K.M. Steps to treat male infertility. Maj. Kedok. Indon. 44 (1): 19-24 (1994). Arsyad K.M. Effect of Protodioscin on the quantity and quality of sperms from males with moderate idiopathic oligozoospermia. Medika 22(8): 614-618 (1996). Barry J.M., Hodges C.V. Impotence, a diagnostic approach. J. Urol. 119: 575-578 (1987). Comhaire F.H. A logical approach to the management of male infertility. Clin. Adv. Androl. 1(3): 8-13 (1991). Ellenberg M. Impotence in diabetes, the neurological factor. Ann. Int. Medicine 75: 213-219 (1971). Greenspan F.S. Basic and clinical endocrinology, 3rd ed. pp. 407-442. Appleton & Lange, Nortwik (1991). Kolodny R.C., Masters W.H., and Johnson V.E. Textbook of sexual medicine. pp. 1-27. Little Brown and Co. Boston (1979). Lee H.Y. Evaluation and management of male infertility. Second Annual Conference of the Korean Andrology Society (1983). Moeloek N., Adimoelja A., Tanojo T., Pangkahila W. Trials on Tribulus terrestris on oligozoospermia. National Congress of Indonesian Association of Andrology Scientific Meeting VI in Manado, Indonesia. Nasution A.W. Treatment of impotence with Libilov. National Congress of Indonesian Association of Andrology Scientific Meeting X in Denpasar (1993). Pangkahila J.A. Libilov™ increases men's sex drives. National Congress of Indonesian Association of Andrology Scientific Meeting X in Denpasar (1993). Rowe P.J., Comhaire F.H., Hargreave T.B., and Mellows H.J. World Health Organization manual for the standardized investigation and diagnosis of the infertile couple. WHO, Cambridge University Press, Cambridge (1993). Susilo W. Impotence, causes and pharmacological solutions. Seminar in Solving Impotence in Semarang, Indonesia (1994). Viktorof I., Bozadjieva E., Protich M., et al. Pharmacological, pharmacokinetic, toxicological and clinical studies on protodioscin. IIMS Therapeutic Focus Vol 2 (1994). Watterauer U. Anatomy of the penis and physiology of erection. In Sexology. Eicher W., and Kockott G. editors. Pp. 115-26. Springer-verlag Berlin, Heidelberg (1988). World Health Organization manual for the examination of human semen and sperm-cervical mucus inter- action, 3rd ed. WHO, Cambridge University Press, Cambridge (1992).