Smooth Muscle
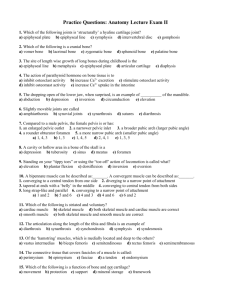
advertisement
Muscle These notes were made by Hadley Wickham, hadley@technologist.com and are licensed under the Creative Commons NonCommercial-ShareAlike License. To view a copy of this license, visit http://creativecommons.org/licenses/nc-sa/1.0/ or send a letter to Creative Commons, 559 Nathan Abbott Way, Stanford, California 94305, USA. Introduction contractile mechanism in all cells, but some cells in multi-cellular organism specialised for contraction = muscle three major types: skeletal, smooth, cardiac all types surrounded by thin basement membrane or external lamina that binds them to adjacent cells Skeletal responsible for movement of the skeleton and organ, voluntary and striated wide variety of forms and functions, but all have same basic structure, composed of extremely elongated multinucleate cells bound together by ct, diameter: 10-100m, length: up to 35cm contraction controlled by large motor nerves, individual nerve fibres branch within muscle to supply a group of muscle fibres collective known as a muscle unit, excitation of one motor nerve results in contraction of all muscle fibres in muscle unit, vitality of muscle depends on maintenance of nerve supply, skeletal muscle also contains highly specialised stretch receptors Connective Tissue individual muscle fibres grouped into bundles called fasciculi with delicate ct called endomysium connecting individual muscles each fascicle is surrounded by loose ct called perimysium supporting tissue component contains both collagen & elastin and acts as a flexible skeleton to which muscle fibres can attach becomes continuous with that of tendons and muscle attachments entire muscle is covered by epimysium size of fasciculi reflects function of muscle: small, highly controlled muscles have small fasciculi & more perimysium, while large less controlled muscles contain large fasciculi and less perimysium large blood vessels enter perimysium and divide to ramify epimysium, fine branches pass transversely through muscle fibres and give rise to numerous longitudinal capillaries Muscle Growth certain mesenchymal cells differentiate into long mononuclear myoblasts which then proliferate (via mitosis) these myoblasts fuse end to end forming progressively longer multinucleate myotubes (<100 nuclei) contractile proteins are laid down in the centre of the myotube pushing the nuclei to the outer edge by birth most muscle growth is completed as is innervation most growth after birth is a result of increase in muscle bulk mature muscle cells are highly differentiated and have little capacity for repair a few myoblasts (satellite cells) persist after maturity which can aid in repair Striations A H I M contractile proteins within cell highly organised, giving rise to A (anisotropic), I (isotropic), H, M and Z bands cross sections show similar organised arrangement Sarcoplasm hardly any sacroplasm, surrounds myofibrils known as T-system, lumen continuous with extracellular space on either side of t-tubule SR forms flattened terminal cisternae, together with T-tubule forming a triad rich with very large mitochondria and glycogen for energy to permit simultaneous excitation of all myofibrils extensive system of tubular invaginations of the sarcolemma surrounds each myofibril at A-I junction between t-tubules a secod mebrance system derived from smooth ER the sarcoplasmic reticulum embraces each myofibril Smooth Muscle specialised for long contractions of relatively low force contraction occurs independently of neural stimulation. influenced by autonomic NS and hormones relatively small and elongated single nucleus located at widest part of cytoplasm bound together in irregular branching fasciculi, with considerable variation b/w organs arranged roughly in parallel within fasciculi contractile proteins not arranged in a parallel orderly fasihion in many tubular structures there are often two layers: one circumferential and the other longitudinal relatively few mitochondria and other intracellular organelles membrane contains numerous flask shaped invaginations called cavelae, though to analogous to T-tubules connected with gap and spot junctions Cardiac Muscle in many ways intermediate between skeletal and smooth long, cylindrical, branching cells one or sometimes two nuclei, centrally located delicate ct b/w cells supports capillary system, analogous to endomysium sarcomeres arranged in continuous 3-D structure also have T-tubule and SR system similar to skeletal but less well organised dyads instead of triads, located at Z disk Intercalated Disks specialised intercellular junctions provide mechanical and chemical/electrical connection always coincide with Z-disks terminal actin filaments of Z-disk attached to fascia adherens which transmit forces b/w cells desmosomes occur less frequently and provide anchorage for intermediate filaments Skin Introduction differs in thickness, colour, presence of hairs, glands and nails all types of skin have same basic structure external surface consists of a keratinised squamous epithelium called the epidermis dermis supports and nourishes epidermis, is fibro-elastic and contains many blood vessels and sensory receptors dermis attached to underlying fatty hypodermis, represents superficial layer of fascia hair follicles, glands, and nails are termed epidermal derivatives because they originate from epidermis Functions protection – UV, mechanical abrasion, chemical, thermal, micro-organisms, prevents dehydration sensation – largest sensory organ, touch, pressure, pain, temperature thermoregulation – major organ of thermoregulation, insulation against heat loss, sweat glands, AV shunts metabolic functions – vit D production, major store of energy (subcutaneous fat) Thick Skin Epidermis very thick epidermal layer has 5 layers stratum germintivum (aka. basale or malpighii) stratum spinosum cuboidal most replication occurs here desmosomes connect adjacent cells ‘prickle-cell’ layer large and polyhedral cells, numerous ribosomes cytokeratin (keratin precursor) aggregates to form tonofibrils which converge upon desmosomes stratum granulosum cells characterised by numerous dense granules within cells more flattened stratum lucidum v thin layer, translucent stratum corneum dead and dying cells and flattened and devoid of organelles Merkel cells are free nerve endings found in thick skin, presumed to be sensory receptors Langerhan’s cells are specialised antigen presenting cells Melanocytes are responsible for skin colour synthesise melanin which is excreted as melasomes and taken up by epidermal cells to be arranged around the nucleus found in basal layers neural crest (neuro-ectodermal) origin long dendritic processes which extend between cells Dermis provides robust supporting layer for epidermis as well as blood supply divided in to 2 zones: Papillary zone Reticular zone most superficial layer relatively loose, highly vascular, contains free sensory nerve endings main bulk of dermis collagen fibres are coarse and disposed in thick irregular bundles elastin is an important component of both layers cells are mainly fibroblasts responsible for laying down connective tissue Skin Appendages variety of appendages principally hairs, sebaceous glands and sweat glands distribution shows large variation b/w tissues but has the same pattern Hair highly modified keratinised structures produced by hair follicles arrector pili muscle attaches the follicular sheath to the dermal papillary zone, contraction erects hair = ‘goose flesh’ hair + muscle + sebaceous gland = pilosebaceous gland hair growth takes place with a terminal hair bulb which consists of actively dividing epithelial cells surrounding a vascular dermal papilla Sebaceous Glands one or more are associated with each follicle (at about 1/3 the way to the skin) secrete sebum, a water-proofing substance branched acinar form found independently in transitions b/w internal and external epithelia Sweat Glands most are simple, tangled coiled tubular glands which secrete a watery fluid onto skin, called merocrine sweat glands important in thermoregulation in axilla and genital region another form is found: the apocrine sweat glands secrete viscous fluid onto hair follicle analogous to odiferous glands in animals, biological important in humans unknown Cartilage Introduction semi-rigid form of connective tissue large proportion of ground substance matrix growth can occur both appositionally and interstitially three types (fibro-,elastic, hylaine) arise from different proportions of matrix components cartilage formation starts with differentiation of mesenchymal cells to chondroblasts subsequent mitotic divisions and matrix deposition give rise to small, round chondrocytes sitting in cells nests, or lacunae most is avascular limiting the thickness to which cartilage can grow forms much of the template for bone growth Hyaline Cartilage most common type of cartilage, also bone precursor characterised by small aggregations of chondrocytes embedded in amorphous matrix reinforced by collagen continuum of cellular characteristics b/w outer zone and perichondrium in adult, cell proliferation does not occur unless stimulated matrix appears rather amorphous, contains collagen type II in interlacing network of fine fibrils chondrocytes rich in glycogen and lipid Fibrocartilage intermediate between cartilage and dense ct found in intervertebral discs, some articular cartilages, pubic symphysis and in some joint capsules consists of alternating layers of hyaline cartilage and thick collagen fibres Elastic Cartilage occurs in external ear, epiglottis, parts of larynx and Eustachian tubes histologically similar to hyaline cartilage but contains large bundles of elastic fibres Bone Introduction specialised form of supporting tissue in which extracellular components are mineralised store of calcium and other inorganic ions all bones are in a continual state of resorption and growth inorganic salts 70% and organic matrix 30% calcium hydroxyapatite is the major inorganic salt involved in the mineralisation of bone the fibrous component in mainly type I collagen (90% of organic matrix) bone exists in two main types: woven lamellar characterised by random arrangement of coarse collagen fibres first type of bone to be formed, and then remodelled to lamellar boen composed of highly organised layers two types of lamellar bone: compact and cancellous Bone Cells three types on cells found in bone: osteoblasts osteocytes derived from osteoprogenitor cells responsible for synthesis of and secretion of organic component: osteoid derived from osteoprogenitor cells formed from osteoblasts, responsible for maintenance of the bone matrix osteoclasts derived from monocyte/macrophage lineage involved in resorptive process Cancellous open sponge-like form forms trabeculae, Compact made of parallel columns of bone which are parallel to axis of bone connect to adjacent Haversian canals via Volkman’s canals each column consists of concentric layers of bone called lamellae arranged around a central containing blood vessels, lymphatics and nerves called Haversian canals remainder of lamellae no longer surrounding Haversian canals are called interstitial systems Generalised Structure of a Long Bone long shaft of compact bone: diaphysis the articular joint surfaces of the bone (epiphyses) are covered by articular cartilage cancellous bone forms medullary cavity which in immature animals is filled with active (red) bone marrow, while in adults most are filled with inactive (yellow) bone marrow external surface invested with periosteum, a thick fibrous layer inner surfaces invested with a delicate endosteum endo- & periosteum contain cells responsible for growth, remodelling and repair