DRUG TREATMENT OF INFLAMMATORY BOWEL DISEASE
advertisement

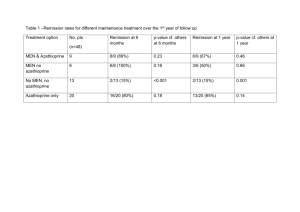
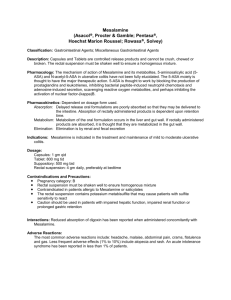
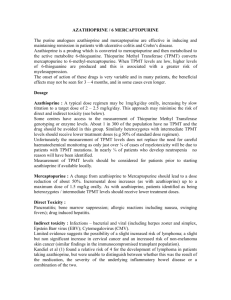
DRUG TREATMENT OF INFLAMMATORY BOWEL DISEASE Objectives Describe the mechanism of action, pharmacokinetics and adverse effects of drugs in IBD INFLAMMATORY BOWEL DISEASE Ulcerative Colitis Crohn’s disease Inflammatory bowel disease Inappropriate inflammatory response to intestinal microbes in a genetically susceptible host Ulcerative colitis - diffuse mucosal inflammation - limited to colon - defined by location (eg proctitis;pancolitis) Crohn’s disease - patchy transmural inflammation - fistulae, strictures - any part of GI tract AIMS OF THERAPY Suppress inflammatory response Suppress the immune reaction Aminosalicylates Acute maintenance corticosteroids acute Aminosalicylates • precise MOA unknown • act on epithelial cells • anti-inflammatory • modulate release of cytokines and reactive oxygen species Aminosalicylates Local effect on mucosa in reducing inflammation Aminosalicylates Sulfasalazine Mesalamine Olsalazine Aminosalicylates Sulfasalazine Mesalamine Olsalazine Sulphasalazine Broken down by gut bacterial azoreductase to 5aminosalicylate & sulphapyridine SULFASALAZINE Bacterial Flora Bacterial azoreductase (Colon) Sulfapyridine Absorbed Systemic Adverse Effect 5-aminosalicylic Acid Acts through the lumen Anti-inflammatory Effect Aminosalicylates 5-ASA absorbed in small intestine Acetylated by N- acetyltransferase-1 Excreted in urine Indications Maintaining remission in UC Reduce risk of colorectal cancer by 75% (long term Rx for extensive disease) Less effective for maintenance in CD Inducing remission in mild UC/CD (higher doses) Contraindications /cautions 5-ASA - Salicylate hypersensitivity Sulfapyridine - G6PD deficiency (haemolysis) - Slow acetylator status ( risk of hepatic and blood disorders) Adverse effects Dose-related Idiosyncratic (rare) - blood disorders - skin reactions – lupus like syndrome; Stevens-Johnson syndrome; alopecia Blood disorders Agranulocytosis; aplastic anaemia; leucopenia; neutropenia; thrombocytopenia; methaemoglobinemia Patients should advised to report any unexplained bleeding; bruising; purpura; sore throat; fever or malaise Steven’s Johnson syndrome immune-complex– mediated hypersensitivity erythema multiforme target lesions, mucosal involvement Newer formulations Mesalazine (5-ASA) Balsalazide (a prodrug of 5-ASA) Olsalazine (5-ASA dimer) Mesalazine Available as Enteric-coated tablets (for ileal Crohn’s disease) Slow release tablets (for proximal bowel Crohn’s) Enemas, suppositories (for distal colonic disease) Used when sulphasalazine can not be tolerated Aminosalicylates Sulfasalazine Oral use Mesalamine (5-aminosalicylic acid). Oral delayed release capsules Enema Olsalazine. 5-ASA-n=n-5-ASA Bacterial flora breaks it into 5-ASA Anti-inflammatory & Immunosuppressive Drugs Corticosteroids Prednisolone Hydrocortisone Corticosteroids USES Remission Induction Route of Administration Oral Intravenous Topical (Enema) Indications Moderate to severe relapse UC & CD No role in maintenance therapy Combination oral and rectal Immunomodulators Azathioprine Cyclosporine Infliximab (Anti-TNF-) Thiopurines Azathioprine MOA: inhibit ribonucleotide synthesis; induce T cell apoptosis by modulating cell (Rac1) signalling Indications Steroid sparing agents Active disease CD/UC Maintenance of remission CD/UC Generally continue treatment x 3-4years Ciclosporin MOA:inhibitor of calcineurin preventing clonal expansion of T cells Indicated in Severe UC No value in CD Methotrexate MOA: inhibitor of dihyrofolate reductase; anti-inflammatory Inducing remission/preventing relapse in CD Refractory to or intolerant of Azathioprine Infliximab Indicated active and fistulating CD - in severe CD refractory or intolerant of steroids & immunosupressants - for whom surgery is inappropriate MOA: anti-TNF monoclonal antibody Potent anti-inflammatory Antibiotics Metronidazole Ciprofloxacin Clarithromycin “Probiotics” (administration of “healthy” bacteria) Summary Drugs for IBD Aminosalicylates Glucocorticoids Immunosuppressives Cytokine modulators Antibiotics Management of UC to induce remission 1. 2. 3. 4. oral +- topical 5-ASA +- oral corticosteroids Azathioprine iv steroids/Colectomy/ ciclosporin (severe) Maintaining remission 1. oral +- topical 5-ASA 2. +- Azathioprine (frequent relapses) Management of CD to induce remission 1. oral high dose of 5-ASA 1. +- oral corticosteroids reducing over 8/52 2. Azathioprine 3. iv steroids/ metronidazole/elemental diet/surgery/infliximab Maintaining remission +- Azathioprine (frequent relapses) Methotrexate (intolerant of azathioprine) Infliximab infusions (8 weekly)