file
advertisement

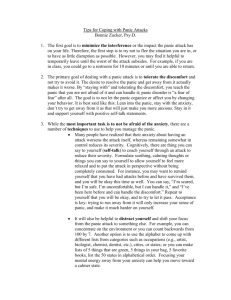
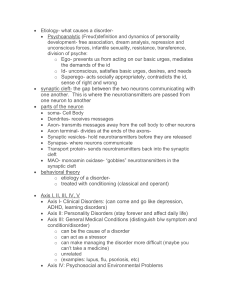
Panic Attack Description: The essential feature of panic disorder is recurrent attacks of severe anxiety (panic), which are not restricted to any particular situation or set of circumstances and are therefore unpredictable. As with other anxiety disorders, the dominant symptoms include sudden onset of palpitations, chest pain, choking sensations, dizziness, and feelings of unreality. There is often also a secondary fear of dying, losing control, or going mad. Panic disorder should not be given as the main diagnosis if the patient has a depressive disorder at the time the attacks start; in these circumstances the panic attacks are probably secondary to depression. Between attacks patients show persistent concern about having another panic attack, and are very worried about the possible implications of such attacks. (1) Diagnosis: A panic attack is a period (usually less that 10 minutes) of intense fear during which a patient has four of the following symptoms: palpitations, sweating, shaking, shortness of breath, feeling of choking, chest pain, nausea, dizziness, fear of going crazy, fear of dying, numbness or tingling, and chills or hot flashes. In panic disorder a patient complains of repeated panic attacks and worries about the next time when a panic attack may occur. Panic Disorder is diagnosed when a patient has had these symptoms for at least a month this worry about future attacks called anticipatory anxiety (2) Differential Diagnosis: Many medical conditions may cause symptoms similar to panic attacks (arrhythmia, cerebral ischemia, coronary disease, and thyrotoxicosis). History and physical examination should be sufficient to exclude many of these. If attacks occur only in specific feared situations, see Phobic disorders. If low or sad mood is also present, see Depression. (3) Management: A.Non Pharmacologic treatment: 1. Basic counseling five sessions should be completed (Problem solving, psychosocial stress management, resources identification, relaxation exercises, improving communication- relations etc) Refer to Counselor.(2 ) 2. Advise the patient to take the following steps if a panic attack occurs: - Stay where you are until the attack passes. - Concentrate on controlling anxiety, not on physical symptoms. - Practice slow, relaxed breathing. Breathing too deeply or rapidly (hyperventilation) can cause Some of the physical symptoms of panic. Controlled breathing will reduce physical symptoms - Tell yourself that this is a panic attack and that frightening thoughts and sensations will soon Pass. Note the time passing on your watch. It may feel like a long time but it will be only a few Minutes. - Identify exaggerated fears which occur during panic (e.g., patient fears that he/she is having a heart attack). - Discuss ways to challenge these fears during panic (e. g., patient reminds him/herself, “I am not having a heart attack. This is a panic attack, and it will pass in a few minutes”). - Self-help groups may help the patient manage panic symptoms and overcome fears.(4) B. Pharmacological treatment: The choice is between a fast acting benzodiazepine and antidepressants, which are well tolerated but have a much slower onset of action. Benzodiazepines are rapidly effective, but Panic symptoms commonly recur after withdrawal, even with slow tapered discontinuation. For pained disorder essential medicine includes: Alprazolam 0.5-2 mg/day or Diazepam 5-20 mg/day. Due dependence risk its better to try benzodiazepine at the beginning and switch to antidepressant latter. (2) 1. Fluoxetine Therapeutic dose: 20-40 mg/day orally. Further increases to 60 mg daily may be considered if no improvement is seen after several weeks Common adverse effects: gastrointestinal disturbances such as nausea, vomiting, dyspepsia, constipation, diarrhea, anorexia, weight loss, anxiety, restlessness, nervousness, insomnia; headache, tremor, dizziness, Sexual dysfunction (1), (2). 2. Amitriptyline: Starting dose: 25-50mg/day orally in divided doses (or as a single dose at night).(1)(2) Therapeutic dose: 75-150- mg/day orally Common adverse effects: dry mouth, constipation, urinary retention, blurred vision and disturbances in accommodation, increased intra-ocular pressure, hyperthermia, drowsiness and increased appetite with weight gain, orthostatic hypotension, tachycardia, sexual dysfunction. Serious adverse effects: electrocardiogram changes, confusion or delirium, hyponatraemia associated with inappropriate secretion of ant diuretic hormone, peripheral neuropathy, tremor, ataxia, dysarthria, convulsions. (1), (2) 3. Benzodiazepines: Diazepam may be given in oral doses of 2 mg one to three times daily, up to oral doses of 5-10 mg twice a day. Lower doses are generally advised in children and adolescents. (1) or Alprazolam 0.5 mg orally up to 2 mg .day (2) Patients should be advised not to drive or operate machinery while taking benzodiazepines. Health care providers should not prescribe two or more benzodiazepines concurrently. Health care providers should avoid benzodiazepines in addiction-prone individuals. Health care providers should not prescribe benzodiazepines in patients with respiratory failure. (1) D. Adverse reactions of benzodiazepines Drowsiness, sedation and muscle weakness are the most frequent adverse effects of Benzodiazepine use. Less frequent effects include vertigo, headache, confusion, depression Health care providers should consider that risk factors for dependence include high dosage, continuous use, use of short half-life benzodiazepines, use in addiction-prone individuals or in those with a history of medicine or alcohol dependence.(1) E. Overdosage of benzodiazepines The outcome of benzodiazepine overdoses is generally favorable unless other medicines, such as alcohol, antipsychotics and antidepressants, have been ingested. If benzodiazepine over dosage is suspected, referral to acute medical facility is recommended.(1) G.Potentially relevant interactions: Alcohol and other sedatives with benzodiazepines enhance sedation.(1) Referral: - Symptoms are severe and attacks are frequent Not controlled by adequate pharmacotherapy Severe depression coexists There is risk of suicide Counseling was not effective There is associated physical illness(2) General advices for patient and family: Panic attack is common and can be treated. Anxiety often produces frightening physical sensations. Chest pain, dizziness or shortness of breath is not necessarily signs of a physical illness; they will pass when anxiety is controlled. Panic attack also causes frightening thoughts: fear of dying, a feeling that one is going mad or will lose control. These also pass when anxiety is controlled. Mental and physical anxiety reinforces each other. Concentrating on physical symptoms will increase fear. A person who withdraws from or avoids situations where attacks have occurred will only strengthen his/her anxiety. Discuss treatment plan with patient(2) Medication instruction: Start antidepressants at low doses Carefully increase the dose to minimize side effects Required doses for panic disorder is similar to that of depression Benzodiazepines are useful for anticipatory anxiety not underlying depression Patient may require repeated reassurance and explanation about the disorder Follow up is important particularly during the initial treatment phase If not effective switch to another A(2) Follow up: Follow up is the essential part of intervention for panic disorder which is for: Assessing compliance, symptoms improvement, referral for counseling, risk of suicide, monitoring side effects, evaluation of psychosocial stresses and family support.(2) References: 1. 2. 3. Pharmacological treatment of mental disorders in primary health care pages 46, 28, 40, 41, WHO 2009 Professional Package for Medical Doctors for Mental Health Working in the BPHS in Afghanistan pages 21, 24, 26, 27 MoPH 2010 Mental Health in Primary Care – Diagnostic and Treatment Guidelines Page 3 WHO 2010