6 Optimization Strategies for Adoption of Standard Terminology to
advertisement

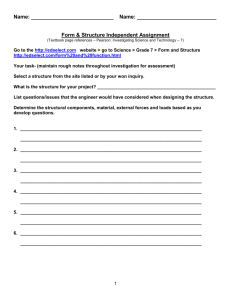
Section 6.5 Optimize Optimization Strategies for Adopting Standard Terminology to Support Semantic Interoperability Standard terminology used at the point of care facilitates good documentation results in improved care. Use this tool to assist with adoption of standard terminology. Time needed: 2 hours Suggested other tools: NA Introduction The health care industry has a number of terminologies. Each terminology generally has a primary focus and the users become very familiar and comfortable with that terminology. A disadvantage is that if each type of health care user has a different terminology, communication across providers is difficult. To overcome lack of semantic interoperability among terminologies for use of health information technology (HIT), many of them have been mapped to more broadly focused terminologies that are more universally used. How to Use 1. Appreciate the importance of adopting a standard terminology. 2. Understand the role of terminology mapping. 3. Adopt appropriate terminologies for each type of use. Importance of Standard Terminology This toolkit provides a summary of the major terminologies in use in healthcare (see Section 1.3 Interoperability for EHR and HIE). The most universally used health care terminology in the United States is the International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9CM). After October 1, 2014, it will be the International Classification of Diseases, Tenth Edition, Clinical Modification (ICD-10-CM). This terminology is maintained by the federal government and drives hospital reimbursement. It is also used for statistical reporting to the World Health Organization. The Current Procedural Terminology (CPT), maintained by the American Medical Association, is the predominant terminology used for provider reimbursement. Although ICD-10-CM contains by far more terms and greater specificity than its predecessors, it is still not as comprehensive or expressive as SNOMED-CT, a multi-axial, clinical terminology created by the College of American Pathologists and maintained by the International Health Terminology Standards Development Organization. SNOMED-CT has been licensed for perpetual use in the United States by the National Library of Medicine , which also supports the tools and processes to map many other terminologies to SNOMED-CT—making it not only extremely comprehensive but universal. Documentation is very important in reimbursement. (“If it’s not documented, it wasn’t done” is the standard mantra.) However, standard terminology for documentation is increasingly important for quality patient care, especially with greater reliance on HIE across disparate providers, without the Section 6 Optimize—Optimization Strategies for Adoption of Standard Terminology to Support Semantic Interoperability - 1 immediate ability to validate understanding and offer clarification. Consider the example of a client saying “I took an aspirin this morning.” If you are in the home, you can validate exactly what form of “aspirin” is meant. However, if the client documents “aspirin” in a personal health record and you review this between visits, you may not know whether it was an acetaminophen, ibuprofen, or other form of pain reliever. There are many uses for standard terminology: Clarity in documentation Clarity in HIE Ability to generate valid reports Generation of knowledge by aggregating a large volume of data and identify useful patterns Incorporation of new knowledge into clinical protocols that improve quality of care Ability to develop logic rules for clinical decision support systems Mapping Terminologies Because we want documentation to be precise and specific to the user’s needs as well as standardized, a number of terminologies have emerged over the years. Several of these are used to describe drugs, including the National Drug Code and a constellation of RxNorm drug databases—all consistent with each other yet offering additional and corollary information. Nursing has many terminologies. There is regularly serious consideration of using SNOMED-CT directly for all aspects of electronic health record (EHR) documentation in support of HIE. If this happens, it will be greatly facilitated by the NLM mapping—so long as current documentation adheres to the standard terminologies for which there are maps. If any individual user or group of users fail to use standard terminology, it will be impossible to accurately correlate a proprietary term with a standard term. The illustration below demonstrates how a single concept, “acute pain” can be documented by a nurse in a hospital which the hospital’s EHR stores as a (North American Nursing Diagnosis Association) NANDA code (00132), sent to a home health agency (HHA) nurse, whose EHR stores “acute pain” as an Omaha code (24). When ready to generate reports and knowledge, a health information exchange organization (HIO) with a terminology server can map both NANDA and Omaha codes to SNOMED-CT (274663001). The use of SNOMED-CT, combined with the various nursing terminologies1 , provides unambiguous data storage and retrieval along with the richness required for clinicians to use the data. This architecture allows coded data to be converted into meaningful reports for secondary data uses. 1 For a comprehensive discussion of the nursing terminologies, see: Lundberg, C. et al. (June, 2008). Selecting a Standardized Terminology for the Electronic Health Record that Reveals the Impact of Nursing on Patient Care. Online Journal of Nursing Informatics (OJNI), 12, (2). Available at http:ojni.org/12_2/lundberg.pdf Section 6 Optimize—Optimization Strategies for Adoption of Standard Terminology to Support Semantic Interoperability - 2 Terminology Adoption Nurse adoption of the appropriate terminology is obviously critical to incorporating standard terminology into our EHRs and make use of it in HIE, as well as knowledge generation and other uses which an HIO can support. Nurse adoption of a standard terminology appears to be heavily influenced by training, previous usage,2 the presence and use of care plans3, especially via EHRs that incorporate nursing terminology through templated menu selection, and potentially the requirement for standard nursing terminologies to be used as part of the collection of federally required data sets. Although most four-year nurse training programs cover nursing terminologies, most other nurse training programs do not address terminologies. Lack of familiarity with the terminology and a lack of understanding why a standard terminology is important, may explain a lack of interest among nurses when it comes to use of standard terminologies in EHRs and other HIT. Few EHRs have embedded nursing terminologies and there are no requirements to do so. This is beginning to change for hospitals and their use of the NANDA terminology, although even in hospitals nursing terminologies often are still often proprietary. The Omaha System is the predominant nursing terminology used in home health care. There are some home health EHR vendors who support the Omaha System. The Minnesota Omaha System Users Group is an excellent resource for care plans and other tools. (See: http://omahasystemmn.org/KBS_care_plans.php. ) In 2013, the federal Office of the National Coordinator for Health Information Technology (ONC) has begun working with the American Health Information Management Association and Regenstrief 2 Thede, L., Schwiran, P., (February 25, 2011) "Informatics: The Standardized Nursing Terminologies: A National Survey of Nurses’ Experiences and Attitudes - Survey I*" OJIN: The Online Journal of Issues in Nursing Vol. 16 No. 2. Available at: http://www.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/Columns/Informatics/ Standardized-Nursing-Terminologies.html Keenan, G. Standardized Nursing Terminology and Communication Protocols Lead to Increased Use of Patients’ Plan of Care, Agency for Healthcare Research and Quality (AHRQ), AHRQ Health Care Innovations Exchange. Available at: http://www.innovations.ahrq.gov/content.aspx?id=1848 3 Section 6 Optimize—Optimization Strategies for Adoption of Standard Terminology to Support Semantic Interoperability - 3 Institute, which manages the standard terminology LOINC (Logical Observations Identifiers Names and Codes), to incorporate LOINC codes into the Outcome and Assessment Information Set (OASIS) C version as a first step toward interoperability standards. (See: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-AssessmentInstruments/HomeHealthQualityInits/OASISC.html. In the absence of federal mandate, home health agencies looking to improve the quality of care offered through their nurses should consider taking the following steps: 1. Determine how standard terminology use fits the agency’s vision and goals. 2. Learn more about standard terminologies and educate nurse leaders who can translate that knowledge into practical applications. 3. Include standard terminologies in requirements specifications for EHR. If your agency already has an EHR, seek information from the vendor as to when standard terminologies may be incorporated. If there are no such plans, encourage consideration. 4. Review requirements for HIE in your HIO. If the HIO has a terminology server, use this as leverage with the agency’s EHR vendor. 5. Evaluate ways to use care plans and other tools that incorporate standard terminologies in conjunction with the agency’s EHR or other health information technology (HIT). 6. As standard terminologies become available in the EHR, train nurses on how and why to use them. 7. Produce reports that demonstrate the results of using standard terminologies. 8. Monitor the research and potential for requirements for adoption of standard terminologies so your agency can be ahead of the curve in preparing for their use. Copyright © 2013 Updated 11-20-13 Section 6 Optimize—Optimization Strategies for Adoption of Standard Terminology to Support Semantic Interoperability - 4