Clear
advertisement
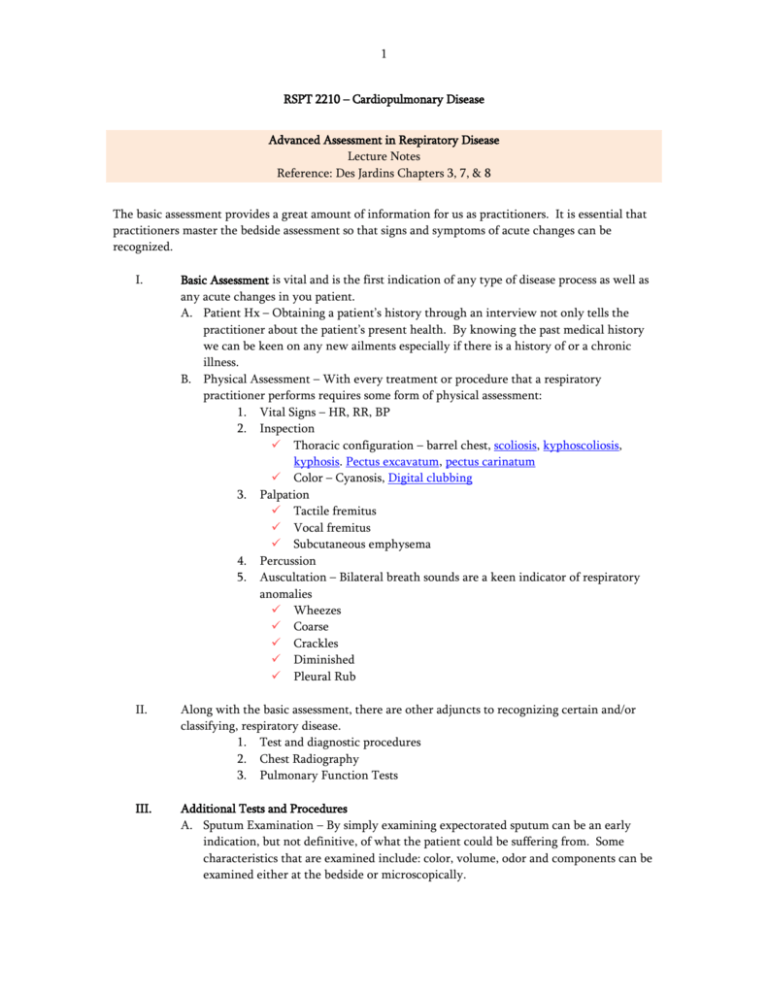
1 RSPT 2210 – Cardiopulmonary Disease Advanced Assessment in Respiratory Disease Lecture Notes Reference: Des Jardins Chapters 3, 7, & 8 The basic assessment provides a great amount of information for us as practitioners. It is essential that practitioners master the bedside assessment so that signs and symptoms of acute changes can be recognized. I. Basic Assessment is vital and is the first indication of any type of disease process as well as any acute changes in you patient. A. Patient Hx – Obtaining a patient’s history through an interview not only tells the practitioner about the patient’s present health. By knowing the past medical history we can be keen on any new ailments especially if there is a history of or a chronic illness. B. Physical Assessment – With every treatment or procedure that a respiratory practitioner performs requires some form of physical assessment: 1. Vital Signs – HR, RR, BP 2. Inspection Thoracic configuration – barrel chest, scoliosis, kyphoscoliosis, kyphosis. Pectus excavatum, pectus carinatum Color – Cyanosis, Digital clubbing 3. Palpation Tactile fremitus Vocal fremitus Subcutaneous emphysema 4. Percussion 5. Auscultation – Bilateral breath sounds are a keen indicator of respiratory anomalies Wheezes Coarse Crackles Diminished Pleural Rub II. Along with the basic assessment, there are other adjuncts to recognizing certain and/or classifying, respiratory disease. 1. Test and diagnostic procedures 2. Chest Radiography 3. Pulmonary Function Tests III. Additional Tests and Procedures A. Sputum Examination – By simply examining expectorated sputum can be an early indication, but not definitive, of what the patient could be suffering from. Some characteristics that are examined include: color, volume, odor and components can be examined either at the bedside or microscopically. 2 1. Color Color/Description Yellow Green Green & foul smelling Brown Bright Red Pink & frothy 2. Association Normal Bronchial Asthma Acute Retained secretions Pseudomonas Old Blood Fresh Blood Pulmonary edema Microscopic examination can help determine the microbes that are causing the infection. The organism can be identified and therapy adjusted to treat the infection. The most common organisms associated with respiratory disorders in listed. (pp. 105, Box 7-1) B. Skin Tests - There are several different types of skin tests. A positive result indicates that the patient has been exposed (but does not mean the disease is present) to the antigen. A negative test result means the patient has not been exposed to the antigen. Common tests include: 1. TB skin test – Identifies if the patient has been exposed to Tuberculosis Bacilli 2. Sweat Chloride test – Presence of increased sodium (Na+) in a sweat test is an indication for Cystic Fibrosis 3. Allergy Test – Performed to determine what allergens a patient will react to. C. Bronchoscopy – This procedure can be diagnostic or therapeutic. The flexible bronchoscope is more commonly used because there is minimal risk to the patient and usually does not interrupt a patient’s ventilation. 1. During a bronchoscopy the following can be directly visualized Upper airways (nose, oral cavity, pharynx) Larynx Vocal cords Subglottic area Trachea Carina Bronchi Lobar bronchi Segmental bronchi (down to 3rd and 4th generations) 2. Diagnostic bronchoscopy – A bronchoscopy is used diagnostically with a patient has a suspected (undiagnosed) infectious disease or to obtain a lung biopsy that is located on or near the bronchi. There are multiple indications for a diagnostic bronchoscopy (refer to pp. 106). Images can be taken while performing a diagnostic bronchoscopy as a record for any abnormalities that are found. 3 3. Therapeutic bronchoscopy – The therapeutic bronchoscopy is used to perform procedures such as bronchial lavage, removing foreign objects, managing life-threatening hemoptysis. *Note: Routine procedures (CPT, deep breathing/cough techniques, postural drainage, etc.) should be the first line of defense in preventing/treating atelectasis. D. Lung Biopsy - performed to diagnose abnormalities that have been found by some other means of investigation, for example an abnormal CXR, or CAT scan. 1. Although many abnormalities can be reached with a bronchoscopy, a lung biopsy is obtained for abnormalities usually found in the periphery of the lung. 2. Tissues collected from a lung biopsy are sent to pathology to be analyzed for any type of malignancy or to determine the presence and origin of an infection. 3. A lung biopsy can be collected two ways: Transbronchial lung biopsy: Utilizing a bronchoscope, forceps or a needle is guided to obtain a sample Open-lung biopsy: An open-lung biopsy is a surgical procedure and the patient must undergo general anesthesia. a. An incision is made and varies according to the suspected problem area. b. Because it is a thoracic surgery, a chest tube is required for 7 – 14 days. There are also larger risks in this procedure, for example pneumothorax, bleeding, infection etc. (pp.106) c. Open lung biopsies are usually performed when a transbronchial biopsy is unsuccessful or a larger tissue sample is required. d. There are contraindications to this type of biopsy including cor pulmonale, pulmonary hypertension, etc. (pp.106-107). E. Thoracentesis – also known, as a thoracocentesis is a procedure used to remove excess or collected fluid in the pleural space. A thoracentesis can be performed diagnostically or therapeutically. 1. Diagnostic thoracentesis – Performed to diagnose the origin of a malignancy and especially pleural effusion. Once the fluid is collected it can be sent to pathology to determine the diagnosing and/or staging of a malignancy. 2. Therapeutic thoracentesis is usually performed to relieve an increased WOB or pain from a pleural effusion, to administer medication to treat fluid accumulation or cancer. 3. The fluid that is in the pleural space can be classified as transudate or exudate. Transudate: fluid from the capillaries spill into the pleural space, usually thin and watery, has a low WBC and protein level a. Usually not caused by pleural surfaces, but can be caused by left ventricular failure, peritoneal dialysis, cirrhosis Exudate: can be caused by a variety of states including infection, cancer, chest trauma etc (pp.108). Each condition will have different 4 protein, WBC and enzyme levels, along with other components such as cellular debris, and blood (pp.108). F. IV. Hematology, Blood Chemistry, and Electrolytes 1. Hematology – The most common blood test is the CBC (Complete Blood Count). Include: (refer to table 7-1, and box 7-2 for normal values and etiology) Red Blood Count (RBC) – The larger portion of the blood. Helps in assessing the patient’s overall oxygen-carrying capacity Hematocrit (Hct) – the volume of RBCs in 100 mL of blood. Hemoglobin (Hb) – oxygen that passes into the pulmonary capillary bed attaches to Hb. White Blood Cell Count (WBC) – WBCs function to fight infection, defend the body using phagocytosis, and produce antibodies in the immune response. 2. Blood chemistry – The RCP should be aware of and have basic knowledge of blood chemistry is important in patient assessment. Refer to table 7-2 for blood chemistry that RCPs should have some knowledge on. a. Glucose – increased glucose indicates that the body is undergoing stress b. Bilirubin – especially in newborns is monitored closely. c. Blood Urea Nitrogen (BUN) – increased levels indicate acute or chronic renal failure 3. Electrolytes-Variances in electrolyte levels can be indications for impending failure, the source of cardiac arrhythmias or in diagnosing diseases (Table 7-3) Sodium (Na+) – increased levels can indicate dehydration Potassium (K+) – increased or decreased levels can lead to cardiac arrest Chloride (Cl-) – related to metabolic acidosis (increased) and alkalosis (decreased) Calcium (Ca+) – Changes in the level of Ca+ can directly affect a patient’s EKG Radiologic Examination of the Chest - Radiography plays an important role in assessing, diagnosis, and evaluating the present state of a patient. An X-ray is an image of internal body structures by passing x-rays through the body to and x-ray film. The most common type of radiographs that a practitioner will be utilizing is the chest x-ray. A. Standard Positions for Chest X-Rays (CXR) 1. Posteranterior (PA) – The image is captured by the patient standing (or sitting) with the film on the anterior portion of his chest and the x-ray apparatus facing his posterior approximately 6 feet away 2. Anteroposterior (AP) – This type of radiograph is utilized most often when a patient is debilitated or unable to stand or sit for the CXR. The film is place against the patient’s back the x-ray source is placed in front of the patient. 5 3. Lateral: Used to complement the PA film. The film is pressed against the side of the chest. To see the right lung and heart the right side is on the film. When placed on the left the left lung and heart is captured. 4. Lateral Decubitus: Similar to the lateral film, but the patient is lying on her left or right side. When the image is named it is referring to which side the patient is lying. Example: “Left lateral decubitus” means – patient with left side down. This film is helpful in the diagnosis of pleural effusion, or free air in the abdomen or thorax. Fluid will accumulate in gravity dependant areas, free air will rise to top of the film. Right lateral decubitus with pleural effusion. B. Radiologic terminology (Table 8-1) 1. Radioluency – describes darker areas (air - black) 2. Radiodensity - appear white on x-ray (dense areas – white) 3. Consolidation – becoming solid; areas of the lung that are solidifying because of pathologic engorgement. 4. Bleb – superficial air cyst 5. Infiltrate – poorly defined radiodensity C. Assessing quality of an X-ray – An x-ray that is properly taken by the technician, will include: 1. Proper position – When the image is captured the patient should be in proper position. The spine should be in the center of the chest with the distance between the costophrenic angles equal. Any rotation could result in false diagnosis i.e. – tracheal deviation, cardiac enlargement. 2. Exposure – Normal exposure is determined by the ability to visualize to the 5th or 6th thoracic vertebrae. Degree of exposure can be determined by examining heart and lung fields Overexposed films – the heart and lungs will be more radiolucent with more exposure Underexposed films – the heart and lungs will appear dense (white). The lungs may have erroneous infiltrates and little to no visualization of the vertebrae. 3. Level of Inspiration – the film should be captured at full inspiration if possible. The diaphragm should be at the level of the 9 th or 10th rib. When a film is taken on exhalation the lungs are denser, diaphragm is elevated and heart looks larger and wider. D. Examining a Chest Radiograph – The best approach to examining a Chest X-ray is to use a systematic approach. The most common is an “inside-out approach.” 1. Mediastinum – Any shifts from midline or increase/decrease in size of the anatomical portions of the mediastinum should be noted. 6 2. 3. 4. 5. 6. Trachea – The trachea is a translucent column that lies on top of the spinal column. The trachea can be shifted by certain conditions. In collapse (atelectasis) the trachea will shift toward the affected area. With fluid or gas accumulation the trachea will shift away from the affected area. Heart – The size of the heart should take no more than half of the chest on the film. When it is larger it is known as an “enlarged heart” and be investigated. Hilar region – The hilar region includes the major vasculature from the heart. Increased density indicates engorgement which is usually related to increase pulmonary vascular resistance. Lung Parenchyma (Tissue) – The lungs should be examined systematically from top to bottom. There are some normal lung tissue markings, but when absent there is a possibility of a pneumothorax, overinflation or overexposure of the film. Pleura – the periphery of the lungs should be examined for fluid (pleural effusion), air (pneumothorax) or lesions in the pleural space. Diaphragm – Right and left hemidiaphragms should be in a dome-shaped contour. The right is usually higher because of the liver. Gastric Air Bubble – Located under the left hemidiaphragm. Bony Thorax – Includes inspection of the ribs, vertebrae, clavicles, sternum, and scapulae. E. Other Radiologic Exams 1. Computed Tomography (CT Scan) – Uses beams of x-ray that rotate in a continuous 360-degree mothion to provide cross-sectional images of the patient. 2. Magnetic Resonance Imaging – Uses magnetic resonance for its source of energy to capture cross-sectional images. Much better than CT scan because the high-contrast images that MRIs show more subtle lesions that would of otherwise been overlooked on a CT scan. 3. Pulmonary Angiography – helps identify pulmonary emboli or AV malformations. Radiopaque contrast is injected through the right side of the heart and into the pulmonary artery to follow pulmonary circulation. 4. Ventilation/Perfusion Scan (V/Q Scan) – Also used in the detection of a pulmonary embolism. Perfusion scan involve the injection of albumin in combination with a radioactive material and distributed by the pulmonary arteries. The lungs are scanned with a gamma camera, dark areas = good blood flow, white or opaque areas = decreased or absent blood flow. Ventilation Scan the patient breathes a radioactive gas, scanned by the gamma camera to display distribution of the gas. Dark areas = good ventilation, light/white areas = decreased or absence of ventilation. If results indicate normal ventilation scan, but abnormal perfusion scan then a pulmonary emboli is present. 5. Bronchography – used in diagnosis or extent of bronchiectasis; the film is called a bronchogram. Radiopaque contrast is instilled into tracheobronchial tree. 7 V. Identifying location of involved areas will allow better administration of postural drainage in bronchiectasis. Pulmonary Function Testing (PFT) – Indicated any time that an assessment of the respiratory system is required or desired A. PFTs will evaluate: 1. Presence of lung disease 2. Extent of abnormal lung function 3. Amount of disability due to dysfunction 4. Progression of the disease 5. Nature of the dysfunction or type of disease 6. Course of therapy for the dysfunction B. Lung Volumes and Capacities 1. LUNG VOLUMES – There are 4 lung volumes that can be measured in a PFT: Tidal volume (Vt) – the amount of gas that is inhaled and exhaled on a normal, daily basis. 10% of the total lung capacity Inspiratory Reserve volume (IRV) – the maximum volume of air inhaled after a normal inspiration. 50% of TLC Expiratory Reserve volume (ERV) – the volume of air that can be exhaled from the end of a normal exhalation. 20% of TLC Residual volume (RV) – the volume remaining after a maximal exhalation. 20% of TLC 2. LUNG CAPACITIES – By adding 2 or more of the lung volumes, 4 lung capacities are formed Total Lung Capacity (TLC) is the maximal amount of air that the lungs can accommodate. It is the sum of all four volumes: TLC = 100%= IRV + 50% + ERV + RV 20% + 20% Inspiratory Capacity (IC) is the volume of gas found in the lung that can be inhaled from a normal resting end exhalation. It is the sum of Vt and IRV: IC = 60% = Vt + 10% + Vt + 10% + IRV 50% Vital Capacity (VC) is the largest volume of gas that can be moved in or out of the lung, represents all the air that can be inhaled and exhaled forcibly leaving only the RV in the lung. It is the sum of the Vt, IRV and ERV: VC = 80% = Vt+ 10% IRV+ 50% ERV 20% 8 Functional Residual Capacity (FRC) is the volume of gas that is left in the lung at the end of a normal exhalation. It is the sum of RV and ERV: FRC = 40% 3. RV+ 20%+ ERV 20% Pulmonary disorders will change the volumes of the patient to be: Obstructive: INCREASED RV, Vt, FRC; VC, IC, IRV and ERV are DECREASED Restrictive: VC, IC, RV, FRC, Vt are all DECREASED Obstructive and Restrictive: DECREASED flows and DECREASED volumes C. Expiratory Flow Measurements 1. Vital Capacity – There are two types of Vital capacity: Slow Vital Capacity – used to measure restrictive disease; decreased volumes will indicate restrictive disease Forced Vital Capacity – the volume that can be exhaled as forcefully and as rapidly as possible after a maximum inspiration 2. Forced Vital Capacity – the patient is instructed to take a maximal inspiration followed by a maximal expiration as forcefully and rapidly as possible. The FVC will provide the important flow rates used to measure obstructive disease. The following values can be measured: FEV1: Forced Expiratory Volume in 1 second; Volume of gas expired over a given time (@0.5, 1.0, 2.0, 3.0 seconds); FEV1 is best indicator of obstructive disease. FEF200-1200: Forced Expiratory Flow 200-1200 is the average flow during the first 1000 mL after 200 mL have been exhaled. Decreased values are associated with large airway obstruction. FEF25-75: Forced Expiratory Flow 25%-75% is the average flow rate during the mid-portion of the FVC. Decreased values are found in the early stages of obstructive disease and associated with small airway obstruction. FEV/FVC ratio: FEV for a given interval expressed as a % of FVC; Decreased values indicate obstructive disease; can have normal values, but may be restrictive. Measurement Min Acceptable FEV 0.5/FVC 60% FEV1/FVC 75% FEV2/FVC 94% FEV3/FVC 97% 9 PEFR - Peak Expiratory Flow Rate is patient effort dependant, may appear normal in abnormal patients, sometimes used to evaluate asthmatic patients (pre & post bronchodilator) D. MVV – Maximum volume ventilation is the largest volume and rate that can be breathed per minute by voluntary effort for usually about 12-15 seconds. Decreased values are associated with obstructive disease; increased Raw, muscle weakness, decreased compliance, or poor pt effort. E. Pre and Post Bronchodilator PFT testing: performed to measure the reversibility of an obstructive pattern. An increase of 15% or more is considered significant. ALL bronchodilator therapy should be held 8 hours prior to testing. F. FRC Measurement (RV, TLC): There are several methods available: 1. He dilution – A % of He is inhaled and diluted by the patient’s FRC the change in He% is used to determine the FRC. 2. N2 wash out – The FRC is washed out of the lung by having the patient inhale 100% O@ to replace the N2 from FRC. The amount of N2 is used to calculate FRC. 3. Plethysmograph/Body Box- uses Boyle’s law to determine total thoracic gas volume at FRC. G. Flow-Volume Loops – Measures the volumes and flow rates of the FVC 1. The patient performs a FEV followed by a FIV. 2. Flow rates are measured directly on the vertical axis. Expiratory flows are above baseline, inspiratory flows are below the baseline 3. Volume is measure directly on the horizontal axis 4. The shape of the flow-volume loop is diagnostic Obstructive – short and wide - Figure 3-10 Restrictive – tall and skinny - Figure 3-11 Flow-volume loops can also help evaluate partial vocal cord paralysis – appears like a large obstruction 10 H. Gas Diffusion (DLCO) – Measures all the factors that affect the diffusion of a gas across the A-C membrane. The CO single breath technique is the most common. 1. The patient inhales a VC of gas containing a known amount of CO, He, and air. 2. Holds breath for 10 seconds, then exhales in to the machine where the gas concentrations are analyzed. 3. The amount of CO that diffuses across the A-C membrane is equal to the toal amount of CO used, minus the amount returned plus the amount remaining in residual volume. Normal DLCO is 25 mL CO/min/mmHg Decreases in DLCO are lung disorders that affect the A-C membrane such as pulmonary fibrosis, scardosis, ARDS. Emphysema is the only obstructive disease that has a decreased D LCO because of the destructive nature of the disease.