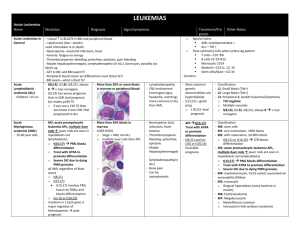
Hairy Cell Leukemia-Myelodysplastic Syndromes
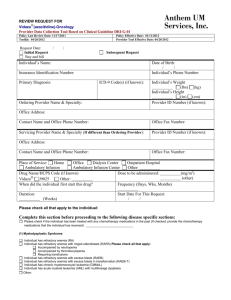
advertisement

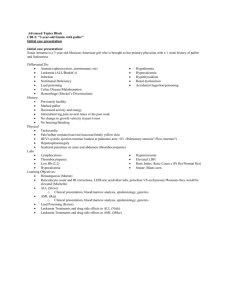
HAIRY CELL LEUKEMIA Rachel Freedman, MD August 1, 2005 Hairy Cell Leukemia (HCL) Uncommon malignancy (2% of all leukemias, 600-800 new cases per year in the U.S.) Chronic/Indolent; B-Lymphocyte origin Originally called Leukemic Reticuloendotheliosis (in the 1920’s) Median age 52 at onset, male:female:4:1 Pathogenesis is unknown but possible etiologies include ionizing radiation exposure, EBV, organic chemicals, farming, and woodworking. There are also some familial cases. The B-lymphocyte/Hairy Cell has the following characteristics Clonal immunoglobulin light and heavy chain gene rearrangement with monoclonal immunoglobulin expression Expresses pan-B surface antigens (CD19, CD20, CD22). Does not express CD21, which is an immature B cell marker Expresses atypical antigens (for B Cells) such as CD11c, CD25, CD103 Produces and assembles fibronectin and elaborates cytokines (basic fibroblast growth factor bFGF-, and TNF-). Fibronectin and bFGF are thought to cause fibrosis of the bone marrow and TNF- is felt to play a role in the pancytopenia that develops. Clonal karyotypic abnormalities in 2/3 cases: often in chromosome 5 (ie trisomy 5, pericentric inversions, and interstitial deletions involving 5q13) Presentation 25% present with abdominal fullness from splenomegaly (which may be massive) 25% have systemic complaints (fatigue, weight loss, weakness), but lack fever or night sweats 25% have bruising, easy bleeding or recurrent infections 25% are asymptomatic/incidental diagnosis PE: 80-90% have clinically evident splenomegaly. Some also have hepatomegaly and lymphadenopathy. Lab findings: 60-80% have pancytopenia, Hct ranging from 20-35, WBC usually < 4000, plt 20200K. However, 10-20% of patients will have a leukocytosis with WBC > 10K, and rarely as high as 200K. Identifying the Hairy Cell Romanovsky-stained peripheral blood - 90% of patients will have a positive stain for Hairy cells. Morphologically is a mononuclear cell, 1-2x the size of a small lymphocyte with eccentric nuclei. The chromatin pattern is reticular and nucleoli are indistinct. The cytoplasm is pale blue to blue-gray, abundant and sometimes described as fluffy. The outline of the cytoplasm is indistinct with projections giving rise to the name Hairy Cells. Bone Marrow - Can have a “dry tap” due to fibrosis (10-20%), or alternatively, the BM shows a hypercellular marrow with diffuse, focal or interstitial infiltration of the marrow by the Hairy Cell. TRAP activity - tartrate-resistant acid phosphatase = historically used to confirm the diagnosis if positive Immunophenotypic findings: Express pan-B-Cell antigens and lack CD5 expression; CD103 is sensitive cell marker for Hairy Cell as well as overexpression of Annexin A1 gene. Cells have “fried egg” appearance because nuclei are spread out given large cytoplasm of cells Differential Diagnosis Other small B-Cell lymphoproliferative disorders associated with splenomegaly O CLL, prolymphocytic leukemia, splenic marginal zone lymphoma Treatment Beth Israel Deaconess Medical Center Residents’ Report Many patients are asymptomatic and can be observed for a number of years before treatment as there is no clear advantage to early treatment Therapy is indicated for the following conditions o Significant cytopenias (ANC < 1000 with repeated infections, Hgb < 11 g/dL, plt < 100K) o Symptomatic splenomegaly o Constitutional symptoms First Line = Purine Analogs: pentostatin (irreversible inhibitor or adenosine deaminase) or cladribine (phosphorylates cladaribine-leads to lymphocytic toxicity) o Induce durable response rates in most patients (60-90%) o Cladribine is the newer agent, but easier to dose - one continuous infusion for 7 days than pentostatin so is preferred for this reason. o Cause immunosuppression for at least 6 months after the dose is given, with CD4+ and CD8+ cells < 200 cells/L. However, opportunistic infections do not seem to be a problem unless there is concurrent use of steroids. Interferon Alpha o one of IFNa’s first uses was on HCL. Administered thrice weekly for 12-18 months with side effects of flu-like symptoms, anorexia and fatigue, nausea and vomiting. o Limited in use b/c after cessation of the infusion, the disease recurs (75-90% response rate but usually only partial remission) o Used now for purine-refractory HCL Splenectomy o First effective therapy for HCL, but does not produce pathologic remissions o 40-70% of patients will see their peripheral counts return to normal (particularly in patients with a hairy cell index (cellularity of bone marrow core biopsy specimen stated as a fraction multiplied by the fraction of the hairy cells in the cellular portion of the bone marrow specimen) of 0.7 or less. o Response is maintained for a median of 20 months, 50% will have disease progression in 5 years o Overall survival at 5 years is 60-70% o Possible indications for splenectomy despite newer agents include: Symptomatic splenomegaly Pancytopenia persistent after chemotherapy Temporizing measure in pregnant women · Also mononuclear antibodies, ie Rituximab (anti CD 20), and anti CD 25, CD 22 Myelodysplastic Syndromes heterogenous group of malignant stem cell d/o marked by dysplastic and inffective blood cell production with variable risk of transformation to acute leukemia Acquired (mutagenic, PV, aplastic anemia) or heritable (ie downs, trisomies, neurofibromatosis, etc) Characterized by cytopenias, hypercellular marrow, cytogeneic abnormalities Usually idiopathic but may be seen after cytotoxic chemotherapy called “preleukemia” as may evolve into acute leukemia (likelihood is proportional to # blasts seen) Annual incidence is 4.1/100K Increased risk with age and male sex FAB Classification Refractory Anemia (RA) (<5% blasts in bone marrow and <1% in peripheral blood) Refractory Anemia with ringed sideroblasts (> 15%) and no excess blasts (RARS) Refractory Cytopenia with multilineage dysplasia (RCMD) (< 5% blasts and 2+ cell lineages w/ severe dysplasia) Refractory Anemia with excess blasts (RAEB 5-19% blasts) Refractory Anemia with excess blasts in transformation (RAEB-T 21-30% blasts +/auer rods) Beth Israel Deaconess Medical Center Residents’ Report Chronic Myelomonocytic leukemia (CMML) = prolif. syndrome with peripheral blood monocytosis (> 1000/mL) (Can have up to20% blasts in marrow, <5% peripheral blood, no auer rods, +/- ringed sideroblasts) Clinical Signs and Symptoms Usually > 60 yo, Increased incidence with age, male predominance Often diagnosed in asymptomatic person due to routine blood work Symptoms are related to the presence of cytopenias - include fatigue, bleeding (thrombocytopenia and/or platelet dysfunction) and infection (due to neutropenia and/or granulocyte dysfunction) May have an indolent course, presenting with weight loss and fever PE: +/- splenomegaly, pallor, signs of infection, petechiae, purpura Skin manifestations = sweet’s and granulocytic sarcoma Labs/Data/Morphology Anemia, almost uniformly present with low reticulocyte count - often requiring transfusion, nl or high MCV (often see ovalomyelocytes, elliptocytes, teardrops, basophilic stippling, etc) Thrombocytopenia (can also have giant platelets) or neutropenia Morphologically abnormal PMNs (bilobed “Pelger-Huet” nucleus, diminished granules, hypersegmeted polys) Hypercellular marrow, often with erythroid hyperplasia, +/- ringed sideroblasts Specialized cytochemistry and immunophenotyping studies Diagnosis much enhanced by cytochemical stains and immunophenotyping Differential Diagnosis: alcohol abuse, Vit B12, folate deficiency, drug effect (VPA), HIV, exposures, aplastic anemia, CML, myelofibrosis etc. Must exclude all of these. Treatment and Prognosis Prognosis difficult to assess with current classification systems so there are now scoring systems as well, which include karyotype, percent blasts, presence of cytopenias) Supportive RBC transfusions Trial of erythropoietin (sometimes effective) Low dose chemotherapy if symptoms are severe (cytarabine/ azacitidine, etc) Supportive G-CSF to raise PMNs and decrease infection If < 60 yo, consider allogeneic BMT Most often fatal due to infections Risk of developing AML is proportional to the degree of blasts found. Other treatments: IL-3, IL-6, IL-11, all-trans-retinoic acid, anifostine, immunosuppressants, thalidomide derivatives (ie lenalidomide), arsenic Beth Israel Deaconess Medical Center Residents’ Report