CBI 2 (Michelle) - U
advertisement
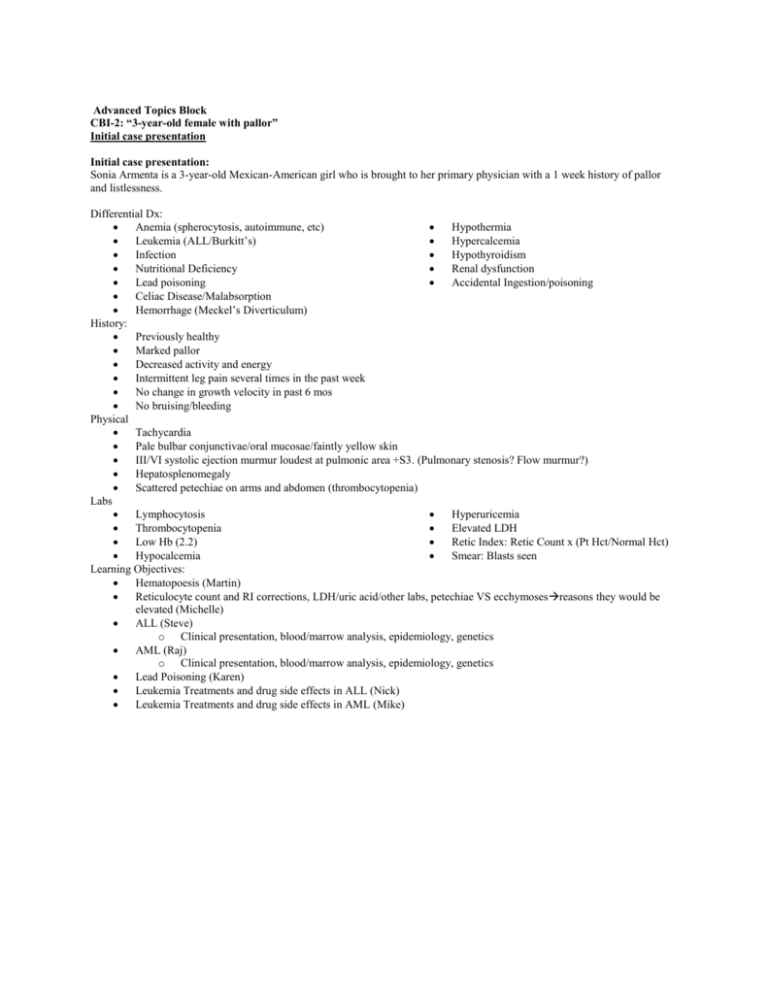
Advanced Topics Block CBI-2: “3-year-old female with pallor” Initial case presentation Initial case presentation: Sonia Armenta is a 3-year-old Mexican-American girl who is brought to her primary physician with a 1 week history of pallor and listlessness. Differential Dx: Anemia (spherocytosis, autoimmune, etc) Hypothermia Leukemia (ALL/Burkitt’s) Hypercalcemia Infection Hypothyroidism Nutritional Deficiency Renal dysfunction Lead poisoning Accidental Ingestion/poisoning Celiac Disease/Malabsorption Hemorrhage (Meckel’s Diverticulum) History: Previously healthy Marked pallor Decreased activity and energy Intermittent leg pain several times in the past week No change in growth velocity in past 6 mos No bruising/bleeding Physical Tachycardia Pale bulbar conjunctivae/oral mucosae/faintly yellow skin III/VI systolic ejection murmur loudest at pulmonic area +S3. (Pulmonary stenosis? Flow murmur?) Hepatosplenomegaly Scattered petechiae on arms and abdomen (thrombocytopenia) Labs Lymphocytosis Hyperuricemia Thrombocytopenia Elevated LDH Low Hb (2.2) Retic Index: Retic Count x (Pt Hct/Normal Hct) Hypocalcemia Smear: Blasts seen Learning Objectives: Hematopoesis (Martin) Reticulocyte count and RI corrections, LDH/uric acid/other labs, petechiae VS ecchymosesreasons they would be elevated (Michelle) ALL (Steve) o Clinical presentation, blood/marrow analysis, epidemiology, genetics AML (Raj) o Clinical presentation, blood/marrow analysis, epidemiology, genetics Lead Poisoning (Karen) Leukemia Treatments and drug side effects in ALL (Nick) Leukemia Treatments and drug side effects in AML (Mike) Friday Session-Presentations Hematopoiesis Formation of all blood cellular components. Components: Erythroid (RBC), lymphocyte (B, plasma, T, NK cells), myelocytes (PMN, eos, basos, MKC’s, monos). PMN>lymphos>monos>eos>basos (Neutrophils Like Making Everything Better) ALL Malignant aggressive neoplasm of immature undifferentiated lymphoid precursor cells with abnormal hematopoiesis. (B cell>T cell). Most common pediatric hematologic neoplasm. B-cell ALL presents as leukemia, T-cell ALL presents as a lymphoma. Presentation: Anemia, thrombocytopenia, neutropenia, B symptoms, HSM (invasion), lymphadenopathy, CNS symptoms (invasion), mediastinal masses (in T-cell). Due to overwhelming of the bone marrow by hyperplastic blasts. Bone marrow analysis: Infiltration of blasts (dark condensed chromatin with little cytoplasm) Cytogenetics: Hyperdiploidy, hypodiploidy, Philadelphia chromosome (t(9:22), TEL/AML (t(12:21) most common), MLL, translocations involving chromosome 14 (T-cell). Risk Stratification: o Low Risk: 1-10 yrs, WBC <50x10^9, hyperdiploid, TEL-AML. (>85% survival) o High Risk: <1 or >10, WBC>50X10^9, BCR-ABL, MLL, hypodiploid, failure of induction, CNS Dz. (>75% survival) ALL Treatment Supportive: antibiotics, transfusions, metabolic, electrolyte. Induction: Vincristine + corticosteroids + asparaginase (90% enter CR). 3-6 cycles, short term. o Response monitored by bone marrow assessment o AML Adverse effects: tumor lysis syndrome (high uric acid, PO4, and K), thrombosis, bleeding, infection Consolidation: Methotrexate/cytarabine/anthracyclines/alkylating agents for 4-6 months. o Goal: Prevent leukemic re-growth and reduce residual tumor burden. o Levels based on risk Maintenance: Daily 6-mercaptopurine with weekly methotrexate for 2-3 years. Stem Cell Transplant: o 1st remission high risk o 2nd remission normal risk Malignant aggressive neoplasm of immature undifferentiated myeloid precursor cells with abnormal hematopoiesis. Clinical Presentation: Anemia, thrombocytopenia, neutropenia, headache, B symptoms, coagulopathies (think DIC), HSM. Bone Marrow: Replacement of the normal marrow by myeloblasts with AUER RODS in the cytoplasm. (Auer rods: composed of fused lysosomes with cytoperoxidase +. (Also seen in APL).) + Elevated circulating blasts. Cytogenetics: Multiple translocations are causative, t(15:17) most common. AML Treatment Considerations: Patient age, past medical history, cytogenetics, functional capacity (Karnofsky/ECOG score). Induction: Reduce tumor burden. o 7+3 (7 cytarabine + 3 anthracycline) Consolidation: Eliminate leukemic cells. o Good prognosis: Cytarabine (3 courses). o Bad prognosis/2nd remission: Stem cell transplant. o Anti CD33 Monoclonal Antibody (Gemtuzimab). Experimental. Relapse Therapy: Prophylaxis o Hydroxyurea (lowering WBC counts), antibiotics. PML (M3 Leukemia): Treated with ATRA (VITAMIN A). Lab Values Reticulocyte: Immature RBC. EPO stimulates marrow in response to low blood O2. Reticulocyte count: Measure of bone marrow response to anemia Corrections: Reticulocyte Index: (Retic%)(Pt Hct/45)(RMT) o <1 indicates failure of the bone marrow response o 4-5 considered good response LDH: Present in many tissues throughout the body. Nonspecific indicator of tissue destruction/cell turnover. Uric Acid: Byproduct of purine nucleotide metabolism. Nonspecific indicator of cell turnover. Lead Poisoning Cause: Repeated exposure to lead (ammunition factories, radiator repairs, lead paint, pica (in children), lead plumbing, and gunshot wounds). Pathogenesis: Lead denatures enzymes involved in heme synthesis and ribosomal degradation. Clinical Presentation: o Mental deterioration & slow growth in children o Peripheral neuropathy (foot and wrist drop) and renal failure in adults o Lead Lines (gums and long bones) o Abdominal colic Lab: o Microcytic sideroblastic anemia. o Basophilic stipling of RBC’s o Blood lead levels: >10 children, >15 adults (>70 MEDICAL EMERGENCY use chelation therapy) Treatment: Chelation therapy (dimercaprol, CaEDTA, succimer-pediatric) CBI-2: “3-year-old female with pallor” RELEASE 4: Conclusion Session #2 (Friday) Sonia had early B-lineage ALL (Acute Lymphoblastic Leukemia). Her flow cytometry revealed an early (precursor) Bcell leukemia with the following pattern of reactivity: CD19 (for B cells), CD34 and Tdt (early lineage), CD10 (B –cell associated) and HLA-DR (HLA Class II). Her cells do not express myeloid (CD13, CD33) or lymphoid linage markers (CD2, CD3, CD7). Additionally, her cells are not mature enough to express surface immunoglobulins. She had standard risk disease based on clinical and molecular features. She responded well to induction therapy and went promptly into remission. She tolerated consolidation and maintenance well. She never required radiotherapy or bone marrow transplantation. She is cured. The majority of children diagnosed with ALL in the United States are treated on clinical trials, and it is through these trials that improvements in treatment come about. ALL is the most common cancer in children, so a large portion of the improvement in outcome shown in the figure below can be attributed to improvements in ALL therapy. Induction, consolidation and maintenance regimens are revised in an iterative fashion as clinical trials are developed in order to improve outcomes for those with the poorest prognoses and decrease toxicity for those with the most favorable prognoses. Looking to the future for Sonia: It is now 5 years later and you are seeing Sonia for a well child check. She is 8 years old but is one year behind in school. Her mother explains that she had difficulty concentrating in school and did not catch on to math and reading the way the other children in her class did. You find out that S. A.’s father had had learning disabilities, as did her older brother. Learning Objectives: 1. 2. 3. 4. Integrate pathophysiologic and morphologic approaches to the classification of anemia in children. Pathophysiologic Classification: o Increased Destruction: Hemolytic Anemia Intrinsic (IE spherocytosis, HbS) VS Extrinsic (IE WAIHA, CAIHA) Intravascular VS Extravascular Mechanical Hemolysis o Decreased Production of RBC (IE aplastic anemia, renal failure w/low EPO, B12/folate deficiency) o Increased Loss Chronic hemorrhage Acute hemorrhage Morphologic Classification: o Macrocytic: B12/folate deficiency o Microcytic: Fe deficiency, anemia of chronic disease, hemosiderosis, thalassemia o Normocytic: Aplastic anemia o Hemolytic: Spherocytosis, G6PD deficiency, HbS, WAIHA, CAIHA, etc Identify the 2 most common types of leukemia in children and explain the specific diagnostic procedures needed to make a correct diagnosis. ALL: Bone marrow biopsy showing >20% blasts with immunohistochemical staining showing B-cell markers (CD19, CD20, CD34 [general blast marker] TdT. Blasts may or may not be seen on peripheral smears, but neutropenia, anemia, and thrombocytopenia are common. AML: Bone marrow biopsy showing <20% blasts with immunohistochemical staining showing myeloid markers (CD13, 14, 15, and CD34). Blasts may or may not be seen on peripheral smears, but neutropenia, anemia, and thrombocytopenia are common. Analyze the concept of risk stratification in pediatric leukemia and identify the key determinants of risk in childhood. High Risk: o Philadelphia Chromosome o MLL Karyotype o Complex karyotypes o Hypodiploid o <1 or >10y/o o >50x10^9 WBC’s o Induction Failure Low Risk: o TEL/AML o 1-10 Y/o o <50x10^9 WBC’s o Hyperdiploid Define the term “remission” and identify major components of therapy used to induce and sustain remission in children with leukemia. Remission: Absence of disease activity in individuals with a chronic disease that cannot be cured. Usually indicates complete absence of symptoms of disease, absence of serum biomarkers, and cessation of growth in the case of cancer remission. Components of Therapy: o Induction: Consists of vincristine, prednisone, and L aspariginase. Designed to get the patient into remission. 90% of children attain remission after induction. Those that do not are considered high risk cases. o Consolidation: Consists of approximately 4-6 months of methotrexate (or another selected chemotherapeutic drug). Designed to reduce residual tumor burden (it can never be completely cleared), prevent drug resistance from occurring, and prevent regrowth of the tumor. o Maintenance: Maintenance can last up to 2 years and consists of weekly treatments of oral methotrexate and daily oral vincristine. Designed to keep the patient in remission. o CNS Prophylaxis: Intrathecal administration of methotrexate is often given to prevent spread of the cancer into the CNS. 5. Explain the concept of “late effects” of therapy in the context of curable malignancies and connect late effects to specific therapies. Agents thought to be associated with long-term cognitive impairment are methotrexate, corticosteroids, and possibly cytarabine. Two thirds of the studies of patients who received chemotherapy alone for ALL have indicated that survivors experience some degree of cognitive decline. It has been postulated that CNS prophylaxis with intrathecal chemotherapy may contribute to neural sequelae (ie chronic demyelinating encephalopathy), but studies to date have not been conclusive. Learning disabilities are often multifactorial, and many children with ALL are diagnosed during their preschool and early primary years. Therefore, in addition to having been exposed to both systemic and intrathecal chemotherapy, these children have also been absent from preschool, kindergarten, and the early grades to a greater extent than most of their peers. Whether effects of therapy are based on pharmacology or early educational experiences, it does appear that young children surviving ALL therapy face specific challenges that require attention from parents, health care providers, and educators.